Pulmonary veno-occlusive disease (PVOD) is a subgroup of pulmonary arterial hypertension with a poor prognosis. The diagnosis is usually delayed and treatment options other than lung transplantation are unfortunately limited. We report the case of a 51-year-old female gardener diagnosed with PVOD by open lung biopsy before her death. Although there are many reported cases of hepatic veno-occlusive disease due to toxic agents present in nature, such as pyrrolizidine alkaloid exposure, to date this has not been linked to PVOD.
La enfermedad pulmonar venooclusiva es una forma infrecuente de hipertensión arterial pulmonar y su pronóstico es sombrío. El diagnóstico suele ser tardío y el único tratamiento curativo en la actualidad es el trasplante pulmonar. Presentamos el caso de una mujer jardinera de 51años cuyo diagnóstico se obtuvo por biopsia pulmonar abierta realizada previamente a su fallecimiento. Si bien existen casos reportados de enfermedad venooclusiva hepática secundaria a agentes tóxicos presentes en la naturaleza, como el alcaloide pirrolizidina, hasta el momento no se han relacionado con la enfermedad a nivel pulmonar.
Pulmonary veno-occlusive disease (PVOD) is an entity that occurs infrequently among a group of conditions causing pulmonary arterial hypertension (PAH). Risk factors include exposure to toxins, such as anorexigens and some chemotherapeutic agents.1 Exposure to naturally occurring pyrrolizidine alkaloids has until now only been related with hepatic veno-occlusive disease.2 We present a case of PVOD in a female gardener, with a slow and complicated course and late diagnosis of the disease.
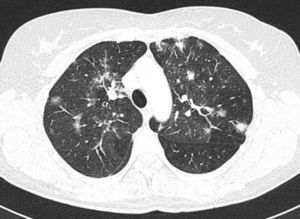
Clinical CaseFemale, 51 years of age, ex-smoker, working as a gardener, seen in another center for progressive dyspnea and dry cough which began 8 months previously. Initial spirometry showed severe obstructive disease. Bilateral pseudonodular opacities were seen on simple chest X-ray. Computed tomography (CT) of the chest revealed patchy, bilateral ground-glass opacities tending to converge in the upper lobes, with areas of consolidation in the right middle and lower lobes, and nodular images of up to 1cm in diameter (Fig. 1). In view of these findings, fiberoptic bronchoscopy was performed, giving negative cytology and microbiology results. Transbronchial biopsy did not provide any significant findings.
Wide-spectrum antibiotics, antifungals and high-dose systemic corticosteroids were subsequently started, but respiratory function continued to decline. Transthoracic ultrasound was then requested, showing severe pulmonary hypertension (pulmonary artery systolic pressure 95mmHg), dilation and slightly reduced right ventricular systolic function and mild-to-moderate tricuspid insufficiency. Thromboembolic disease was ruled out on a repeat chest CT scan, although in this examination, progression of pulmonary interstitial involvement was observed.
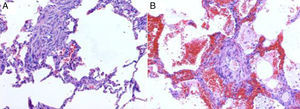
The patient's condition continued to worsen, so she was transferred to our center and admitted to the intensive care unit, where progression of the lung lesions was confirmed by radiology. A lung biopsy was performed by thoracotomy, but the patient could not be extubated after the procedure and died a few days later. Autopsy showed signs of severe pulmonary hypertension, with peripheral areas of ischemic infarction and foci of interstitial fibrosis–all compatible with PVOD (Fig. 2).
DiscussionPVOD is an uncommon and underdiagnosed manifestation that is frequently misclassified among the group of idiopathic PAHs (IPAHs).1 Early diagnosis is important, due to its poor prognosis and poor response to pulmonary vasodilators, which can cause severe pulmonary edema.3
In contrast to IPAH, which is associated with mainly precapillary involvement, the physiopathological effect of PVOD is to produce lesions in the post-capillary pulmonary vessels. There is media hypertrophy and intimal fibrosis, causing occlusion of the vascular lumen. Muscle cell proliferation, calcium accumulation in the vascular wall, thrombotic occlusion of the microvessels and occult pulmonary hemorrhage due to post-capillary blockage are also often observed.
Diagnosis is complicated by a clinical presentation similar to that of IPAH. The most common symptom is progressively increasing dyspnea. There may be mild hemoptysis and chronic cough. When pulmonary hypertension is severe, cyanosis, chest pain or syncope with exercise may be observed. Infrequent presentations include diffuse alveolar hemorrhage and sudden death.
Open lung biopsy is the reference test for diagnosis. However, it must be taken into account that while histological proof is needed for diagnosis, the risks presented to patients by this procedure limit its extensive use.
The diffusing capacity of carbon monoxide is usually reduced, and in most cases ventilation is restricted. Hypoxemia is more severe than in IPAH, since it is negatively affected by pulmonary edema, alveolar hemorrhage and extensive vascular obstruction due to fibrosis. The most frequent findings on CT are centrilobular ground-glass opacities, septal lines and mediastinal lymphadenopathies. Pleural effusion may occur in the final stages of the disease. Hemosiderin-laden macrophages may be found in bronchoalveolar lavage. Transbronchial biopsy does not usually lead to a diagnosis.1,4
PVOD has a poorer prognosis than other forms of PAH. The only curative treatment option is lung transplant. Mean survival is 24 months from diagnosis and mortality usually is a result of severe right ventricular dysfunction and massive pulmonary edema.4
Risk factors for this disease include BMPR2 gene mutations. PVOD has also been associated with various connective tissue diseases. Association with toxin exposure has also been documented.1,4 Although there have been cases of hepatic veno-occlusive disease due to inhalation of pyrrolizidine, a naturally occurring alkaloid present in various trees and bushes,5 until now, no case of PVOD associated with this toxin has been reported. Our patient was a gardener and may have been exposed to this type of agent, although it cannot be definitively established that this was the cause of her disease.
Please cite this article as: Rodríguez Rodríguez P, Pedraza Serrano F, Morán Caicedo LP, Rodríguez de Guzmán MC, Cebollero Presmanes M, de Miguel Díez J. Enfermedad pulmonar venooclusiva en una mujer jardinera. Arch Bronconeumol. 2014;50:40–41.