Bronchobiliary fistula is an abnormal communication between the bile duct and the bronchial tree. In 1850, Peacock described the first case in a 20-year-old woman with hepatic echinococcosis.1 It is a rare entity,2 and few cases have been reported in the literature. Morbidity and mortality are high, and the diagnosis is essentially clinical, guided by the pathognomonic presence of biliptysis, or bile in the sputum.3 Bile has a corrosive effect on the lung and pleural space.
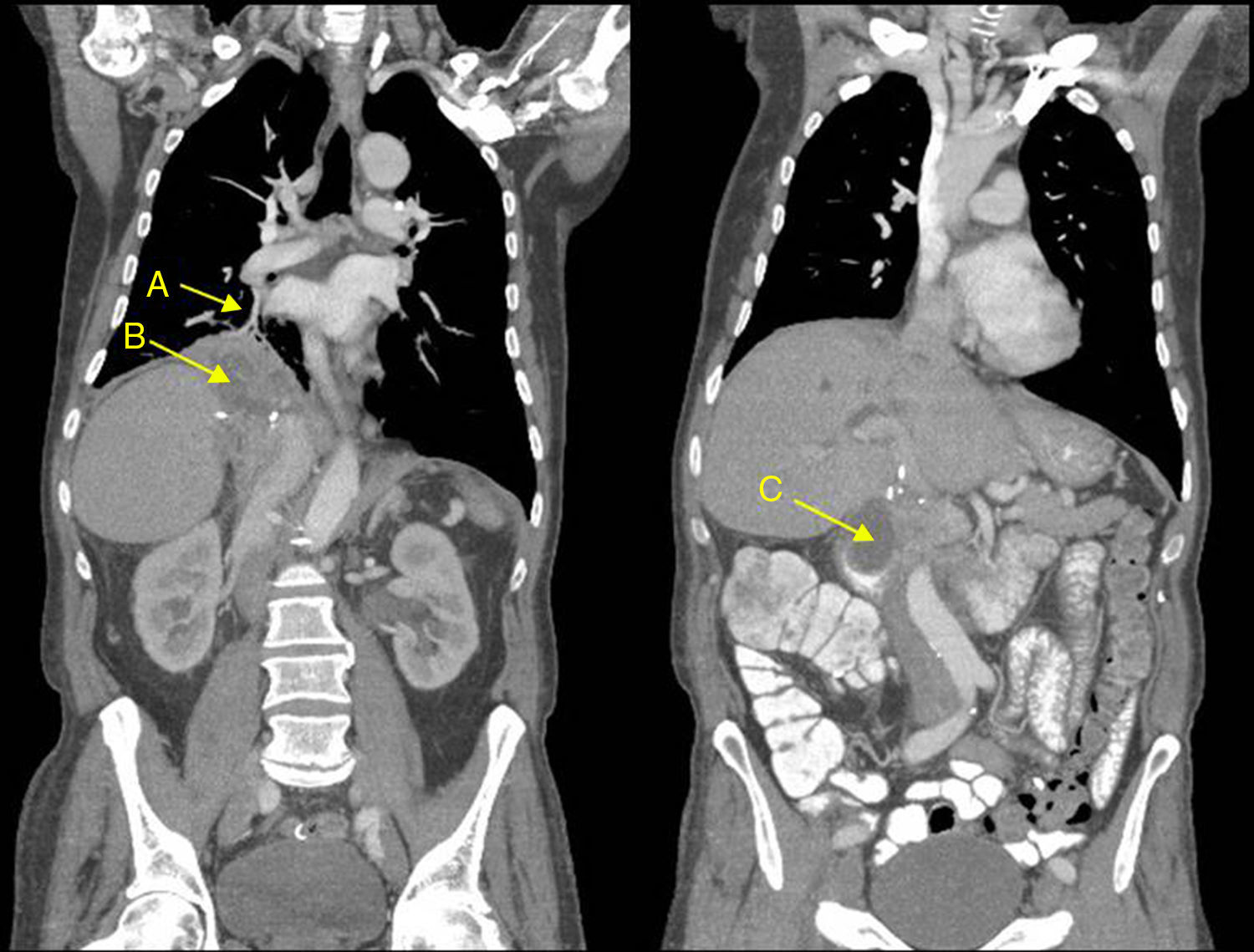
We report the case of a 57-year-old man who presented in the emergency room with a 3-day history of fever 38.5°C and bilous expectoration. Significant history included sigma adenocarcinoma with liver metastases, for which he received neoadjuvant chemotherapy with irinotecan and cetuximab. Portal vein embolization and surgical resection of the liver metastasis (right hepatectomy, section of segment 4 A, and left lobe), cholecystectomy and splenectomy were subsequently performed. He received single-agent cetuximab until sigmoidectomy with colorectal anastomosis, which was performed 8 months before he presented in the emergency room. At that time, the sigma cancer was in remission (CEA 3.9ng/ml), and the patient was being treated with cetuximab every 15 days. On physical examination, arterial blood pressure was 130/80mmHg, heart rate 115bpm, temperature 37.5°C, and oxygen saturation 89%. Poor general condition, conjunctival icterus, reduced breath sounds in the right field with crackles, and hepatomegaly of 2 finger breadths. Clinical laboratory tests showed significant leukocytosis (25790/μl) with neutrophilia (80%). Chest X-ray revealed consolidation in the right lower lobe. Given the likelihood of a biliopulmonary fistula as a late complication of liver surgery, a computed tomography (CT) of the chest-abdomen was requested, which showed parenchymal involvement in the right lower lobe due to a fistula between the right lower lung and the hepatobiliary and subphrenic space. Both the CT and the nuclear magnetic resonance cholangiography showed a large collection extending craniocaudally from the right hemithorax to the subhepatic region, measuring 16cm. This was composed of a multiseptated subphrenic collection (7.5×12cm) connecting with a subhepatic collection (4.5×4.5cm) (bilioma) (Fig. 1).
Empirical antibiotic therapy began with a 12-day course of meropenem. Percutaneous cholangiography was performed, with placement of double external percutaneous biliary drainage in segments II and III. The procedure was incident-free.
Although the patient was initially transferred to the intensive care unit, his clinical and radiological course were very favorable with resolution of fever on day 3, improvement of respiratory failure, and resolution of radiological infiltrate. At discharge, he was prescribed a third-generation cephalosporin (cefixime) for 1 week. The follow-up chest-abdomen CT 11 days after discharge showed reduced involvement of the right lower lung, with some small residual image along the length of the fistula and reduced subphrenic collection (6.2×3.67cm).
Bronchobiliary fistulas can be congenital or acquired. Acquired fistula occur due to 3 mechanisms:
- 1.
Fistula due to trauma is the most frequent, caused by injuries penetrating the lung, diaphragm and liver. Bile duct surgery is included in this category, particularly laparoscopic interventions. In our case, the fistula was a secondary complication of previous liver surgery.
- 2.
Fistula due to liver disease, the most common causes being hydatid cyst and amebic liver abscess.
- 3.
Fistula due to bile duct obstruction.
Recommended diagnostic procedures for bronchobiliary fistulas are percutaneous transhepatic cholangiography,4 bronchoscopy, 3-dimensional CT reconstruction,5 and cholescintigraphy.4 Magnetic resonance imaging with contrast medium contributes functional data. There is no consensus regarding the therapeutic management of these fistulas; a review of the literature suggests reserving surgery for fistulas that do not respond to conservative treatment or for complicated cases.
Please cite this article as: García MM, María AM, Briz MC. Fístula biliobronquial, una complicación tardía de la cirugía hepática. Arch Bronconeumol. 2018;54:285–286.