Meningeal carcinomatosis (MC) is an uncommon and devastating entity characterized by malignant infiltration of the leptomeninges and subarachnoid space. Although it is usually a later finding in patients with known disseminated disease, it can also be the initial manifestation.
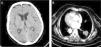
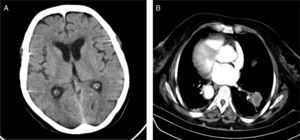
We report the case of a 71-year-old woman, non-smoker, with situs inversus totalis who was admitted to a neurology department due to a 2-month history of progressive visual and hearing loss. Physical examination showed bilateral amaurosis and hypoacusia. Brain computed tomography (CT) showed no intracranial lesions (Fig. 1A) and gadolinium-enhanced magnetic resonance imaging (MRI) of the brain showed no focal or diffuse leptomeningeal enhancement or tumoral lesions. A lumbar puncture was performed and pathological analysis of the cerebrospinal fluid (CSF) revealed adenocarcinoma cells with immunohistochemistry showing positivity for TTF-1 and cytokeratin 7, indicative of a pulmonary origin. A chest CT showed a 3cm lobulated mass in the right lower lobe (RLL) (Fig. 1B). A percutaneous CT-guided core biopsy was conducted in an attempt to obtain additional tumor tissue to perform EGFR mutation sequencing. Histology showed pulmonary parenchyma occupied by neoplastic structures with adenocarcinoma features which stained diffusely for TTF-1 and cytokeratin 7. The patient died during hospital admission due to aspiration pneumonia. One week later the biopsy of the RLL mass showed that the tumor harbored EGFR G719C mutation in exon 18.
MC is more commonly diagnosed in patients with hematological tumors followed by breast and lung cancer.1 Of the latter, small cell lung cancer has the highest rate of meningeal dissemination.2 Non-small cell lung cancer (NSCLC) presenting with MC and without brain parenchymal metastasis is an extremely rare event. Furthermore, simultaneous presentation of blindness and deafness has been exceptionally reported in the literature.3
Prognosis is extremely poor and an optimal treatment modality is difficult to determine since most performed studies are small and retrospective and often include multiple concomitant regimens. In our case, the use of EGFR tyrosine kinase inhibitors (TKIs) could have had a relevant impact in the patient's evolution, as these agents seem to be particularly effective, improving performance status and survival in patients with EGFR positive NSCLC.4
Our report illustrates an extremely rare case of a NSCLC presenting with MC, itself with an exceptional clinical manifestation – simultaneous blindness and deafness – in the absence of brain parenchymal metastasis and brain MRI changes.
Please cite this article as: Nascimento LM, Reis R, Fernandes A. Ceguera y sordera como manifestación inicial de un cáncer de pulmón no microcítico. Arch Bronconeumol. 2016;52:115–116.