A 63-year-old non-smoking, asthmatic man, employed as a manual worker in a timber factory, presented with 3-day history of productive cough associated with greenish sputum, wheezing, shortness of breath and left-sided pleuritic chest pain. On examination, he was pyrexic (38°C) and hypoxic (oxygen saturation 87% on room air). Bilateral wheezing and coarse crackles were heard at the left base of his lung on auscultation.
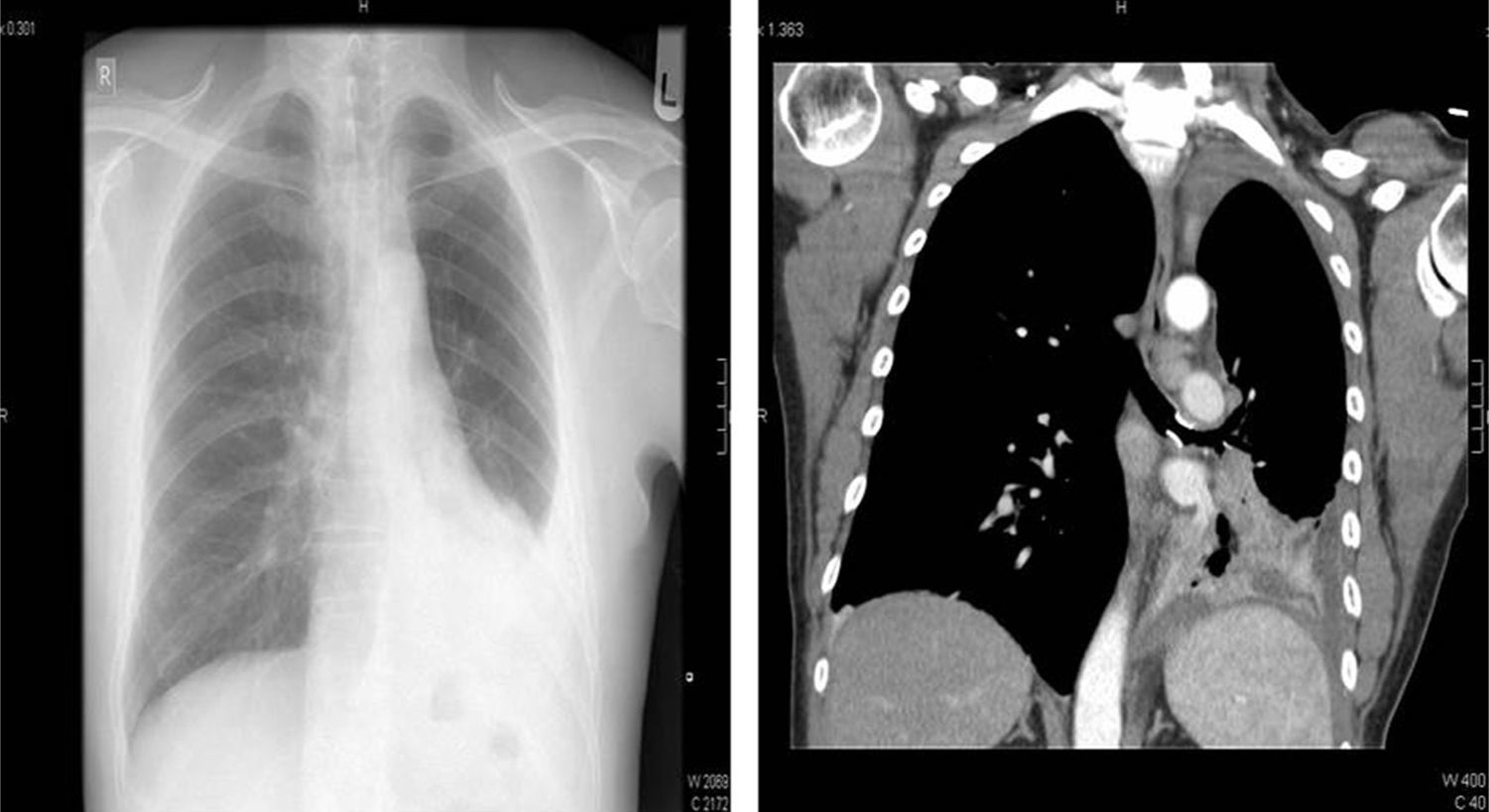
Chest radiograph showed a moderate amount of left-sided pleural effusion. A chest drain was subsequently inserted, as the pH of the exudative fluid was 6.8. Interestingly, chest computed tomography revealed a metallic foreign body within the main bronchus with collapse of the left lower lobe (Fig. 1). Bronchoscopy confirmed the presence of a metal stent-like object overlain by granulation tissue in the left main bronchus. The granulation tissue was firmly embedded into the foreign body making it hard to extract the foreign body. We therefore referred the patient to the cardiothoracic surgeon for removal of the foreign body via rigid bronchoscopy under general anesthesia. The foreign body turned out to be a pigeon foot ring. Upon close questioning, the patient did not recall any choking episode but did admit to being a pigeon fancier 20 years previously.
Foreign body aspiration is uncommon in adults.1 A study performed by the Mayo Clinic retrieved 60 adult cases over a period 33 years.2 In Taiwan, two studies reported 47 and 43 cases over a 13- and a 15-year period, respectively.3,4 The nature of the inhaled foreign bodies tends to differ among different populations. In the Western population, it is more common to find vegetable matter, while bones and watermelon seeds are more common in Chinese and Middle Eastern population, respectively. Surprisingly, acute presentation of foreign body inhalation is rare. Up to 80% and 25% of the cases present with cough and dyspnea, respectively. Patients do not always recall choking and the diagnosis is often missed. Foreign body are usually dislodged in the lower bronchi or the bronchus intermedius. Chest radiograph may sometimes show an opaque subject along the airway or consolidation, atelectasis or effusion. Computed tomography scan of the thorax frequently shows the presence of a radio-opaque object. Flexible bronchoscopy has become the diagnostic procedure of choice for foreign body aspiration in adults. Complications of foreign body aspiration include asphyxia, haemoptysis, post-obstruction infection and bronchiectasis. Glucocorticoids can be useful in cases where foreign body is encased in bulky and friable granulation tissue. Rigid bronchoscopy is usually required for difficult cases such as our case, as it allows the coaxial passage of multiple instruments, including grasping forceps and suction catheter, for a successful extraction. This technique is characterized by specific technical problems in that the anesthesiologist and the operators share the same space, namely the airway. Several potential complications (hemorrhage inside the airway, threat to ventilation, etc.) may therefore arise.5
Please cite this article as: Kooblall M. Un cuerpo extraño insólito. Arch Bronconeumol. 2016;52:116–117.