Lung cancer is the leading cause of cancer death in both sexes worldwide.1 Typical techniques for the anatomopathological diagnosis of lung lesions are transthoracic needle aspiration and biopsy obtained by fiberoptic bronchoscopy. The first can be performed by fine needle aspiration and biopsy (FNAB) or by core needle biopsy (CNB), guided by either ultrasound or computed tomography (CT), depending on the site of the lesion. The second technique includes bronchial biopsy of lesions visible on endoscopy, linear endobronchial ultrasound-guided aspiration of nodules or mediastinal lymphadenopathies, and radial endobronchial ultrasound with electromagnetic navigation to sample lesions located in the periphery of the lung and thus not accessible by conventional bronchoscopy.2
The technique is selected on the basis of a series of parameters, such as lesion site, the presence of pulmonary emphysema, or other comorbidities. In recent years we have witnessed the rise of thoracic ultrasound, both in the diagnosis of different lung diseases and in interventions, and this technique is proving useful for guiding lung lesion biopsies.3,4 Because air does not transmit ultrasounds, lesions must be located in the periphery of the lung or within a suitable acoustic window. Although ultrasound-guided biopsy of lesions in central lung cancer with atelectasis has been described,5 very few reports have been published in the literature on ultrasound-guided biopsy of intrapulmonary nodular lesions in patients with atelectasis and pleural effusion.6
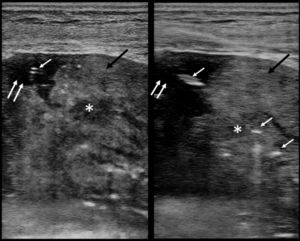
We report a series of 5 patients who, between August 2017 and December 2019, underwent transthoracic biopsy of central lung lesions in the presence of atelectasis and pleural effusion, in whom no nodular lesions were clearly visualized on chest CT. We used a Siemens Acuson X300™ echograph for this study. Color Doppler was used at the entry point to minimize the risk of puncturing vascular structures. All procedures were performed by a single operator using the freehand technique. The probe size was selected on the basis of the distance from the chest wall to the lesion. A linear probe (6.2–10MHz) was used in 3 cases, a convex probe (1.5–5MHz) was used in another case, and in 1 case both types of probe were used. A Trucut-type core needle (Acecut®, TSK Laboratory, Europe, Molenstraat 15, 2513 BH, The Hague, The Netherlands), 14G in diameter and 22mm in length, was used to obtain the histological sample. Hypoechoic lesions were identified within the atelectasis and biopsied under ultrasound guidance (Fig. 1). Pleural implants were also observed in 2 cases, so to complete staging, a pleural biopsy was also performed through the same access port, using a second Acecut®.
B-mode ultrasound showing heterogeneous echostructure (black arrows) corresponding to pulmonary atelectasis with small pleural effusion (anechoic area indicated with double arrow). Hypoechoic lesion (asterisk) corresponding to the nodular lesion to be biopsied identified inside the atelectasis. The hyperechoic linear images (white arrows) correspond to core needle biopsy.
Four of the 5 patients were men. Mean age was 70 years (70±18.12 years). Biopsies were obtained from the right hemithorax in 3 patients, and from the left hemithorax in 2 patients. All lesions were located in the lower lobes.
An adequate sample was obtained in all cases. The diagnoses from the intrapulmonary biopsy were: 4 adenocarcinomas, 2 of which were EGFR mutation-positive, and 1 epidermoid carcinoma. Pleural biopsies were positive for epidermoid carcinoma in 1 case and for adenocarcinoma in the other. Pleural biopsy and lung lesion biopsy were performed on an outpatient basis in 1 patient, and during hospital admission in all others.
Ultrasound-guided aspiration offers several advantages over CT-guided procedures, including the absence of ionizing radiation, a shorter procedure time,7 a lower complication rate,8 and a similar diagnostic yield in peripheral lesions, although the existence of small nodular lesions seems to have less influence on ultrasound-guided biopsy,9 while infiltration of the chest wall can be better visualized.10 Ultrasound aspiration is performed in real time, allowing the needle tip to be clearly visualized inside the lesion, while the use of color Doppler also minimizes the risk of puncturing intercostal arteries or other vascularized regions. In CT, in contrast, the aspiration is not performed in real time and diagnostic yield is reduced in small lesions whose position may be affected by artefacts caused by respiratory movements or association with the costal arches.11
CT, moreover, is not the ideal method for locating pulmonary nodules in pulmonary atelectasis, since it often does not properly distinguish areas suggestive of tumor involvement from the rest of the parenchyma. In our series, the simple visualization of hypo- or anechoic lesions in the pulmonary parenchyma of lungs with atelectasis on ultrasound helps differentiate lesions suggestive of malignancy from the surrounding parenchyma. In many cases, certain tools such as ultrasound contrast12 and color Doppler,13 which are useful for assessing the decrease in vascularization of the area to be biopsied, and elastography14,15 help increase the diagnostic accuracy of lesions suggestive of malignancy. An additional benefit of ultrasound is that it can be performed at the patient's bedside, which is an advantage in patients with poor general condition and restricted mobility. It is important to obtain an adequate sample by core needle techniques, so that molecular receptors may be identified in some cases, guiding the use of other specific treatments that are more effective and better tolerated than conventional chemotherapy.
Although our results should be interpreted cautiously because of the small number of patients included, it should be noted that no complications occurred due to the procedure. Indeed, performing the biopsy under ultrasound guidance helps reduce the chance of accidentally puncturing areas such as vascular structures. The existence of underlying pulmonary atelectasis is likely to reduce the chances of complications such as hemorrhage or pneumothorax. The imaging technique, moreover, is harmless, because it does not emit radiation. For all these reasons, we believe that this could be a good diagnostic alternative, although more comparative studies with the techniques in current use are needed.
Please cite this article as: López González FJ, García Alfonso L, Cascón Hernández J, Ariza Prota M, Herrero Huertas J, Hermida Valverde T, et al. Biopsia de lesiones intrapulmonares en pulmones con atelectasia y derrame pleural. Arch Bronconeumol. 2021;57:438–439.