Inflammatory pseudotumor is a rare entity that represents less than 1 % of all tumors of the lung.1 Its radiological characteristics when viewed with standard tomographic techniques overlap with those of other entities,2 complicating differential diagnosis, especially in lung cancer.
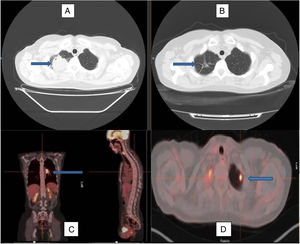
We report the case of a 49-year-old woman, former smoker with a pack-year index of 2, and a history of hypothyroidism. Her regular treatment was levothyroxine 75 mcg, 1 tablet a day. She attended the emergency department due to headache following an episode of sinusitis, with no associated respiratory symptoms. The baseline study included a standard chest X-ray, which revealed an incidental finding of a right apical lesion of irregular contours. An initial CT scan was requested that revealed a “rounded tumor mass in the right lung vertex, irregular contours, lobulated and spiculated towards the surrounding parenchyma. Lesion with heterogeneous enhancement with contrast, in extended contact with the posterior and superior apical pleura, measuring about 45×42mm, with no evidence of pleural or extrapleural infiltration or extension; at the apex of the left lung, a small, nodular subpleural, lesion measuring less than 1cm of dubious significance is observed”. In light of these findings, positron emission tomography was performed. This highlighted the presence of this lesion, which was metabolically active with a maximum standardized uptake value (standarized SUVmax) of 27.5, and the lesion in the left upper lobe, which had an SUVmax of 7.5. Bilateral hilar adenopathies were seen in the mediastinum, in particular a left hilar conglomerate measuring 3.2×2.1×4.1cm with a SUVmax of 14.1 (Fig. 1). Given the high suspicion of malignancy, we decided to conduct a core needle biopsy of the larger lesion, the result of which showed the presence of fibrosis and polymorphous lymphohistiocytic exudate suggestive of an inflammatory process or inflammatory pseudotumor. The molecular study was negative for EGFR gene mutations, but genetic studies were not performed for ALK. Tumor markers (CEA, CA 15.3, CA 19.9, CYFRA-21, squamous cell carcinoma Ag, Pro-GAP, and enolase) were negative. No anemia or thrombocytosis was detected. These results needed to be confirmed by a repeat core needle biopsy, which provided a similar diagnosis. We also performed fiberoptic bronchoscopy, which revealed mucosal thickening of inflammatory appearance in the left lower lobe. Blind bronchial brushing was performed of this region, yielding no neoplastic cells. In the absence of any suggestion of malignancy, and the existence of several lesions that prevented a surgical approach, we decided to start treatment with deflazacor at doses of 1mg/kg body weight per day for 2 months, tapering to half in the following 2 months, and discontinuing the following month. Three computed axial tomography scans were performed during treatment, showing a progressive decrease in tumor size, as well as the presence of linear tracts of fibrotic scar tissue and traction bronchiectasis in the area, with disappearance of the contralateral nodule.
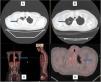
Computed axial tomography image at diagnosis (A) and after treatment with corticosteroids (B), showing remission of the lesion in the right upper lobe, with some remnants of residual fibrous tracts (arrows). PET-CT image with enhanced uptake in the left pulmonary hilum (C) and in the left upper lobe (D), marked by arrows, reflecting the multilocular involvement of this case.
Inflammatory pseudotumor can occur in any organ, but it mainly affects the lung1 and occurs more frequently in the first 2 decades of life.2 It usually presents as a single, circumscribed mass measuring more than 3cm, and is more common in the lower lobes.3 It has been described in the literature under different names (plasma cell granuloma, inflammatory myofibroblastic tumor or proliferation, xanthoma, fibroxanthoma, xanthogranuloma, fibrous xanthoma, xanthomatous pseudotumor, plasmocytoma, solitary mast cell granuloma, inflammatory fibrosarcoma),4 bearing witness to the complexity, histological heterogeneity, and variable behavior of this entity that, at times, can even be classified as a true neoplasm.5 Its etiology is unknown, although there are believed to be several predisposing factors: surgeries, trauma, immune reactions, steroids, radiation therapy, and infections.6 The role of an infectious agent seems to be restricted to the early stages, when it triggers a cascade of reactions, through which the tumor develops autonomy.7 The microorganisms most frequently associated with inflammatory pseudotumor include mycobacteria, Epstein-Barr virus, Actinomycetos and Mycoplasma, and some cases have been reported in association with Corynebacterium equi, Escherichia coli, Klebsiella, Bacillus sphaericus, Pseudomonas, Helicobacter pylori, Coxiella burnetii,4,8,9 herpes simplex virus, and even with HIV infection.10 Pathological study shows fibrous bands interspersed by irregular layers of lymphocytes, histiocytes, and polyclonal plasma cells.11 Although surgical resection is the treatment of choice,12 several recent studies have reported rearrangements of the ALK gene on chromosome 2p23 causing aberrant expression in about 50 % of cases.13 This suggests that this subgroup could show sensitivity to tyrosine kinase inhibitors such as crizotinib.14 The only publications supporting their effectiveness are case series,6,13 and no trials have been conducted to compare the administration of crizotinib compared to corticosteroids in this subgroup.
The efficacy of corticosteroid therapy varies, and the results reported in the literature1,12,14,15 from first-line use in patients who are not candidates for surgery1,14,15 (e.g., bilateral presentation) are limited and inconclusive. Lee et al. reported a similar case in which the response to corticosteroids was excellent, showing no evidence of recurrence after 20 months of follow-up after disappearance of the lesions.14 Díez et al. obtained similar results after a 30-month course of low-dose corticosteroid therapy.15 Few cases of bilateral lesions, such as those presented in our patient, have been reported, and the effectiveness and recurrence rate after steroid treatment are unknown, due to the absence of studies in this area.
Please cite this article as: Delgado Torralbo JA, Masa MP, Crespo EL. Afectación pulmonar bilateral. Opciones no quirúrgicas del pseudotumor inflamatorio, a propósito de un caso. Arch Bronconeumol. 2020;56:49–51.