Hypercoagulable states in cancer are well known to be closely associated with thromboembolic phenomena. After a thromboembolic event, the incidence of malignant tumors, mainly of the blood, pancreas, ovary, liver, kidney and lung, ranges between 2% and 25%. The most common sites are venous thrombosis of the lower limbs and pulmonary thromboembolism, and reports of cases in other venous territories are unusual.
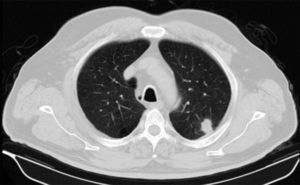
We report a 68-year-old man, smoker of more than 40 pack-years, who was seen in the ophthalmology clinic for a 20-day history of loss of sight in the right eye. Examination of the eye revealed bilateral venous thrombosis of the retina. Additional examinations were performed to rule out secondary systemic disease. Clinical laboratory, coagulation, serological and autoimmune examinations and computed tomography (CT) of the brain were performed; all results were negative. A chest X-ray was performed, revealing a nodule in the left upper lobe (LUL). Chest CT confirmed a 14mm spiculated nodule in the posterior region of the LUL, indicative of malignancy (Fig. 1), and a diagnosis of lung adenocarcinoma was confirmed by the pathology report. No pathological contrast uptake was found in any other sites on PET-CT.
The merits of extensive screening for occult malignancy after idiopathic thromboembolic events are still widely debated. The latest evidence suggests that this practice is only justified in high-risk patients (recurrent thrombotic events in spite of anticoagulation, and portal or hepatic vein thrombosis) due to high healthcare costs, but basic screening studies with laboratory testing, protocolized according to age and chest X-ray results, may be beneficial.1–4 Finally, it is important to note that while the most commonly affected territories are the veins of the lower limbs and the lungs, a small percentage of venous thrombosis in unusual sites may also indicate occult malignancy or other systemic diseases. Thus, each case should be evaluated on an individual basis, and minimal basic screening is a possible approach.
Please cite this article as: Jodra Sánchez S, Andrés Blanco AM, Abad Manteca L. Trombosis venosa inusual como primera manifestación de neoplasia pulmonar. Arch Bronconeumol. 2015;51:156–157.