Guidelines have been published to provide protocols standardizing clinical activity and procedures in direct puncture arterial blood collection for the determination of arterial blood gases (ABG).1,2 However, some earlier studies3 and clinical experience seem to indicate that the techniques used by professionals still vary and that guidelines for the performance of this procedure are not always followed, especially those aimed at reducing pain caused by the procedure.
In this article we aim to explore and compare attitudes and perceptions surrounding the arterial puncture technique for determining ABG in adults among nursing professionals in the pulmonology and emergency departments of several third-level hospitals in the Basque Country (Spain).
A cross-sectional analytical study was conducted using a voluntary, anonymous survey of active nursing professionals from 4 hospital emergency departments (ED) and 5 pulmonology inpatient departments (PID) from 5 third-level hospitals in the Basque Country, with a staff of 285 emergency nurses and 79 pulmonology nurses.
The survey was prepared ad hoc by the researchers, using other previous studies as a model.3,4 Content validation was performed sequentially by way of a review of the initial questionnaire by the researchers, a critical analysis by a group of experts, and a pilot survey completed by 10 nursing professionals to verify adequate understanding by the study subjects. The final questionnaire comprised a section of social and vocational variables and a series of questions centered on self-perception/self-evaluation of different attitudes toward the technique, using open- and closed-ended questions and descriptive rating scales.
The questionnaire was distributed between January and February 2020 by institutional email among the nursing staff who were working at the time in the units selected for study. A reminder was sent 15 days after the initial invitation.
Categorical variables are expressed as absolute frequencies and percentages. To test the hypothesis, the X2 test or Fisher test with a 2-tailed significance level of 95% (P<.05) was applied. The magnitude of the association with the effect variable “no local anesthesia used” according to different covariables was evaluated by crude calculation of the odds ratio (OR) and 95% confidence interval (95% CI). Data analysis was performed using SPSS 25 and OpenEpi 3.01.
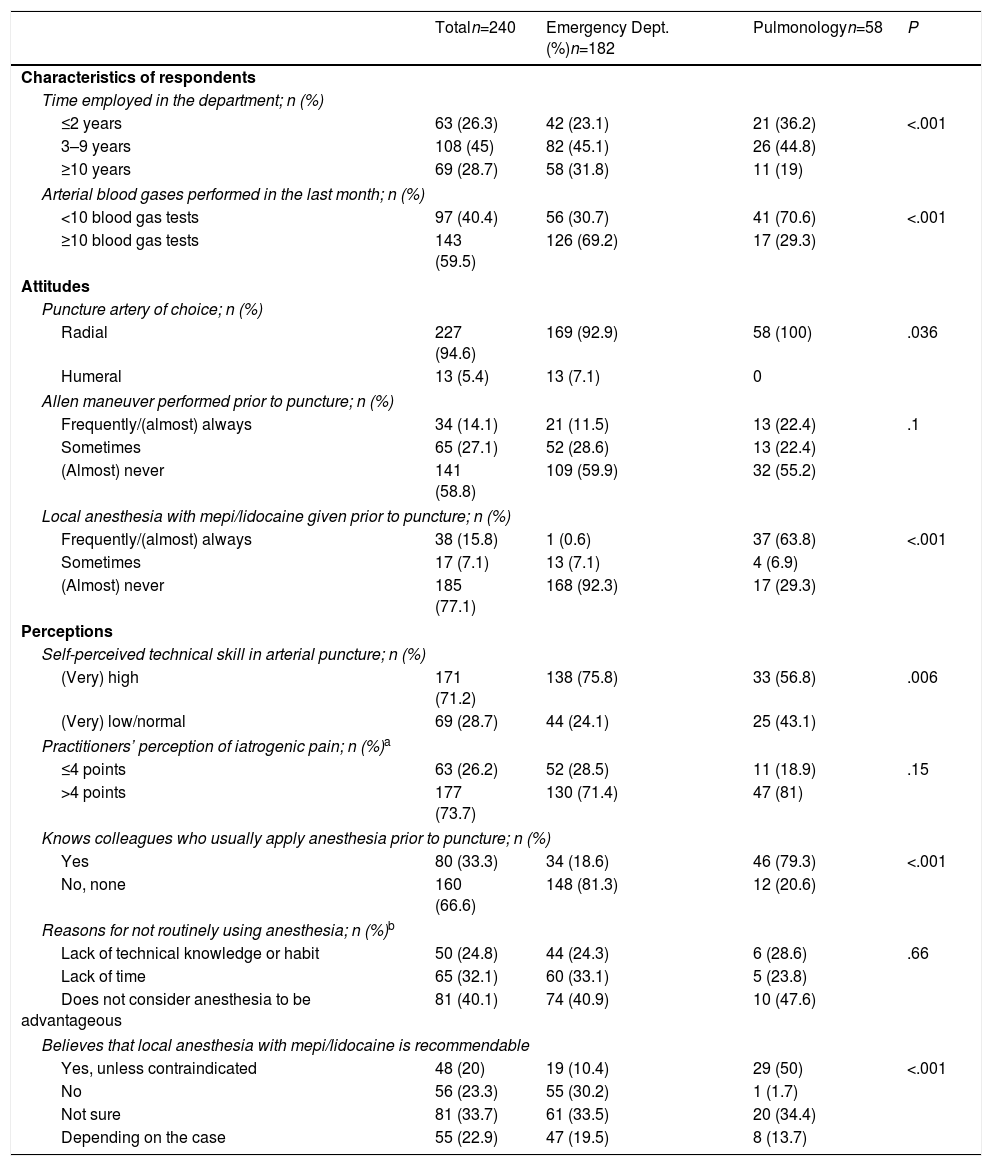
A total of 185 nurses from EDs and 58 from PIDs participated in the survey (65.9% participation rate). Table 1 describes the main characteristics of the respondents and their responses to questions on their attitudes and perceptions regarding the ABG technique.
Perceptions and Attitudes Toward Arterial Puncture for Arterial Blood Gases Determination Among Nurses in the Emergency Departments and Pulmonology Inpatient Departments.
| Totaln=240 | Emergency Dept. (%)n=182 | Pulmonologyn=58 | P | |
|---|---|---|---|---|
| Characteristics of respondents | ||||
| Time employed in the department; n (%) | ||||
| ≤2 years | 63 (26.3) | 42 (23.1) | 21 (36.2) | <.001 |
| 3–9 years | 108 (45) | 82 (45.1) | 26 (44.8) | |
| ≥10 years | 69 (28.7) | 58 (31.8) | 11 (19) | |
| Arterial blood gases performed in the last month; n (%) | ||||
| <10 blood gas tests | 97 (40.4) | 56 (30.7) | 41 (70.6) | <.001 |
| ≥10 blood gas tests | 143 (59.5) | 126 (69.2) | 17 (29.3) | |
| Attitudes | ||||
| Puncture artery of choice; n (%) | ||||
| Radial | 227 (94.6) | 169 (92.9) | 58 (100) | .036 |
| Humeral | 13 (5.4) | 13 (7.1) | 0 | |
| Allen maneuver performed prior to puncture; n (%) | ||||
| Frequently/(almost) always | 34 (14.1) | 21 (11.5) | 13 (22.4) | .1 |
| Sometimes | 65 (27.1) | 52 (28.6) | 13 (22.4) | |
| (Almost) never | 141 (58.8) | 109 (59.9) | 32 (55.2) | |
| Local anesthesia with mepi/lidocaine given prior to puncture; n (%) | ||||
| Frequently/(almost) always | 38 (15.8) | 1 (0.6) | 37 (63.8) | <.001 |
| Sometimes | 17 (7.1) | 13 (7.1) | 4 (6.9) | |
| (Almost) never | 185 (77.1) | 168 (92.3) | 17 (29.3) | |
| Perceptions | ||||
| Self-perceived technical skill in arterial puncture; n (%) | ||||
| (Very) high | 171 (71.2) | 138 (75.8) | 33 (56.8) | .006 |
| (Very) low/normal | 69 (28.7) | 44 (24.1) | 25 (43.1) | |
| Practitioners’ perception of iatrogenic pain; n (%)a | ||||
| ≤4 points | 63 (26.2) | 52 (28.5) | 11 (18.9) | .15 |
| >4 points | 177 (73.7) | 130 (71.4) | 47 (81) | |
| Knows colleagues who usually apply anesthesia prior to puncture; n (%) | ||||
| Yes | 80 (33.3) | 34 (18.6) | 46 (79.3) | <.001 |
| No, none | 160 (66.6) | 148 (81.3) | 12 (20.6) | |
| Reasons for not routinely using anesthesia; n (%)b | ||||
| Lack of technical knowledge or habit | 50 (24.8) | 44 (24.3) | 6 (28.6) | .66 |
| Lack of time | 65 (32.1) | 60 (33.1) | 5 (23.8) | |
| Does not consider anesthesia to be advantageous | 81 (40.1) | 74 (40.9) | 10 (47.6) | |
| Believes that local anesthesia with mepi/lidocaine is recommendable | ||||
| Yes, unless contraindicated | 48 (20) | 19 (10.4) | 29 (50) | <.001 |
| No | 56 (23.3) | 55 (30.2) | 1 (1.7) | |
| Not sure | 81 (33.7) | 61 (33.5) | 20 (34.4) | |
| Depending on the case | 55 (22.9) | 47 (19.5) | 8 (13.7) | |
Note: The final numbers may not account for 100% of the sample due to missing values.
While the Allen maneuver is rare in both departments, the use of strategies to control iatrogenic pain was significantly higher in PIDs, where the proportion of nurses who believe that the systematic use of local anesthesia is recommendable is also higher. However, there were no differences between departments in nurses’ perception of pain caused by the procedure: 73.7% of respondents estimated that the puncture generated more than 4 points on the 0–10-point NRS-11 numeric pain scale.
The factors most strongly associated with the non-routine use of anesthesia were not knowing other colleagues in their department who used it (OR 66.7; 95% CI 22.2–273.8); performing ABG in the ED (OR 28.2; 95% CI 13.1–63.8); perception of iatrogenic puncture pain less than or equal to 4 points on the NRS11 scale (OR 3.6; 95% CI 1.5–9.7), and high or very high self-perceived arterial puncture skill by the professionals themselves (OR 2.3; 95% CI 1.2–4.5).
The use of the Allen test as a screening method for deficits in palmar collateral circulation is described in most of the reference guides,1,2 but this maneuver is highly controversial, and some authors have advised against it.5
There is some scientific consensus that any pain scoring more than 3 points on the NRS11 scale should be treated.6 In the case of ABG, the pain generated by the technique is evaluated by the patients at between 2 and 5 points and, while differences emerge depending on the difficulty of the procedure,7–9 it is widely agreed that the use of measures to mitigate iatrogenic pain should be evaluated. Local injection of mepi/lidocaine is the most common practice used to mitigate this type of pain,10,11 but it is rarely applied in EDs.
The reason for poor adherence to anesthesia most often given is the perception that the routine injection of mepi/lidocaine at the site of arterial puncture offers no therapeutic advantage. Indeed, although clinical guidelines advocate its systematic administration, the scientific evidence in this regard is inconclusive12 and some authors currently propose as an alternative the use of selective anesthesia based on criteria of patient preference, professional expertise, and technical difficulty of the puncture.13 In our study, we observed that nurses who considered themselves expert or who felt that the pain caused by their punctures was less than 4 points on the NRS11 scale were more reluctant to use anesthesia on a regular basis.
The lack of time available to apply anesthesia (attributed to high demand for care or emergency situations) has also been highlighted as an argument for omitting anesthetic treatment. The emergency situation is the main contraindication for anesthesia use during ABG procedures, but patients who attend EDs and who are classified with triage levels higher than II on the Manchester scale should not be deprived of this resource, since the use of anesthesia does not involve a clinically relevant investment of time.
Finally, lack of training in local anesthesia administration and poor organizational culture (measured by whether the practitioner knows other colleagues who use anesthesia) are other causes of low adherence to iatrogenic pain management that are easily addressed through education and awareness programs.
In conclusion, it is clear that the arterial puncture technique for ABG is significantly different if it is performed in the ED or the PID. In general, some technical heterogeneity exists in the collection of arterial blood, and pain management is, in particular, an area that must be improved if we are to reduce suffering in the practice of a nursing procedure as common as ABG.
Conflict of InterestsThe authors declare that they have no conflicts of interest in relation to this article.
Please cite this article as: Ballesteros-Peña S, Vallejo de la Hoz G, Fernández-Aedo I. Actitudes y percepciones frente a la técnica de punción arterial para gasometría: diferencias entre enfermeras de los servicios de urgencias y de neumología. Arch Bronconeumol. 2020;56:528–530.