Necrotizing mediastinitis (NM) is defined as the progression of a distant acute infection towards the mediastinum1, involving its structure2,3 and causing necrosis of the tissues involved. This is a rare but potentially lethal complication with a mortality ranging from 10% to 40%, depending on the series4. This high morbidity is derived from the severity of the process4 and the need for prolonged admission in most cases2.
The most frequently associated foci are otolaryngological infections1, usually from a dental or oropharyngeal abscess5, and less frequently from cervical spine infections4,6. The infection spreads via deep retropharyngeal6, pretracheal, or vascular7 fascia, facilitated by intrathoracic negative pressure, severity, and breathing1,4,7. For this reason, it is normally called descending NM. Dissemination from a source other than the head and neck is exceptional, although other foci, such as abdominal, chest wall, lung, lymph nodes, and even hematogenic spread, have been described1.
We report the case of an 83-year-old patient with a history of hypertension and type 2 diabetes mellitus, permanent atrial fibrillation treated with anticoagulation, complete atrioventricular block with pacemaker implantation, and obstructive sleep apnea syndrome. The patient had undergone endoscopic retrograde cholangiopancreatography to perform a sphincterotomy with plastic stent placement to treat repeated biliary colic complicated with acute pancreatitis of biliary origin and cholangitis. As endoscopic revisions were required due to large calculi obstructing the stent, we decided to perform a cholecystectomy.
He was scheduled to be admitted from home but reported vomiting and diarrhea in the days prior to admission. On the morning of the intervention, he presented hypotension 50/30 mmHg with generalized deterioration of his condition and metabolic acidosis with hyperlactacidemia (19 mmol/l) and pH 7.22, so the procedure was suspended and the patient was admitted to the intensive care unit. During admission, his hemodynamic status was highly unstable and he developed acute renal failure (creatinine 2.42 mg/dl), elevated acute phase reactants (mild leukocytosis of 13.43 × 109/l, C-reactive protein 150 mg/l, and procalcitonin 48.59 ng/dl), elevated liver enzymes, and hyperbilirubinemia.
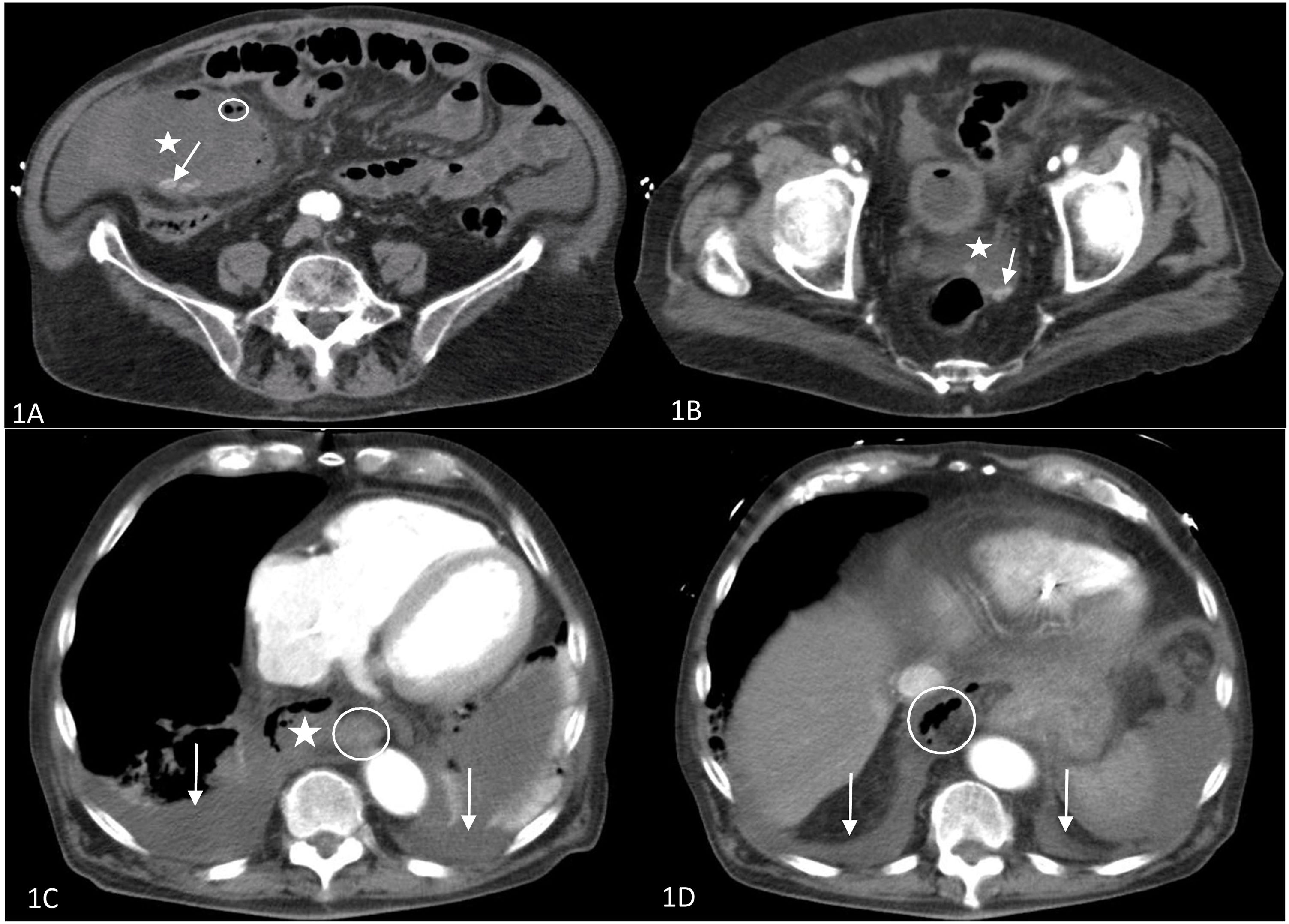
An urgent chest-abdomen computed tomography scan was performed, showing acute emphysematous cholecystitis (Fig. 1A) complicated with probable bilioperitoneum (Fig. 1B). An incidental finding was bilateral pleural effusion and collections in the mediastinum containing air, indicative of NM (Fig. 1C), and air in the retroperitoneum extending to the mediastinum (Fig. 1D). No esophageal ruptures were identified, which, together with the absence of subcutaneous emphysema, allowed us to reasonably rule out esophageal perforation.
A and B: Abdominal CT 1A: Enlarged gallbladder (asterisk) containing lithiasis (arrow) and free gas in the wall of the gallbladder (circled), indicative of emphysematous cholecystitis. 1B: Pouch of Douglas containing free fluid (asterisk) and lithiasis (arrow), showing bilioperitoneum. C and D: Chest CT. 1C: Upper chest slices; mediastinal collection containing air (asterisk); esophagus (circled); bilateral pleural effusion (arrows). 1D: Thoracoabdominal sections; diaphragmatic domes (arrow); retroperitoneal air (circled) progressing to the chest.
Given the progression of the sepsis, support measures were intensified with high-dose amine supplementation, broad-spectrum antibiotic therapy, and orotracheal intubation. However, the patient developed multiorgan dysfunction. The combination of the fulminant nature of the symptoms, the rapid progression, hemodynamic instability, age and associated comorbidities led us to rule out aggressive surgical debridement of the infectious focus as being too risky, even though the symptoms were unlikely to improve with conservative management. The patient died a few hours later.
NM is a polymicrobial infection of the mediastinum caused by aerobic and anaerobic microorganisms4,5 which, despite combined treatment, still has high mortality rates. Early multidisciplinary management7 in specialized centers6 using broad-spectrum antibiotic therapy subsequently adjusted according to the results of sensitivity testing5,7 and aggressive surgical drainage of the primary focus and mediastinum are key to patient survival4,5. A delay in diagnosis and surgery of more than 24 h has been associated with an unfavorable prognosis3.
The main risk factors and predictors of mortality include the presence of previous comorbidities, acute renal failure1, and severe sepsis or septic shock2,5. Patients with signs of sepsis and/or septic shock should be admitted to the intensive care unit2–4. The length of stay in the unit and severity at admission have a direct impact on mortality3.
Early diagnosis is therefore fundamental4,7, though complex6, and a high level of suspicion is necessary2 since the clinical picture is nonspecific, marked by the primary focus (such as trismus, dysphagia, or even abdominal pain)5, and by chest pain, dyspnea, and signs of sepsis4. Computed axial tomography remains the diagnostic technique of choice for establishing the origin of infection, assessing its extension, and planning surgery4,7. The diagnosis can be defined by the presence of a remote focus with radiological findings indicative of mediastinitis3.
Spread of an abdominal infection to the mediastinum, though rare, has previously been described in the literature. Chang and Chen8 describe the first published case of mediastinitis marked by extensive necrosis and abscess formation in the mediastinum caused by a pancreatic pseudocyst. Chong et al.9 later reported a patient with acute pancreatitis complicated by the formation of a paraesophageal pancreatic pseudocyst associated with NM. Finally, Dajer-Fadel et al.10 described a patient with emphysematous pyelonephritis and mediastinal progression of infection with NM. They suggest that the route of dissemination is retroperitoneal spread of air and infection to the mediastinum. These cases illustrate the possibility of propagation to the mediastinum with the development of secondary ascending NM.
This is therefore the first case reported in the literature of ascending NM associated with emphysematous cholecystitis, and the fourth case of ascending NM from an abdominal focus. Given the rarity of this form of presentation, this complication should be considered in patients with a history of abdominal infection and generalized decline. Combined treatment with antibiotic therapy and surgical debridement has been shown to reduce mortality. A high level of suspicion is necessary to allow early diagnosis and the rapid introduction of therapeutic measures.
We thank the Intensive Care Unit for their time and dedication.
Please cite this article as: Sánchez-Matás C, Aldabó-Pallas T, Palacios-García I, Jiménez-Sánchez M. Mediastinitis ascendente necrosante. Un caso excepcional. Arch Bronconeumol. 2021;57:780–782.