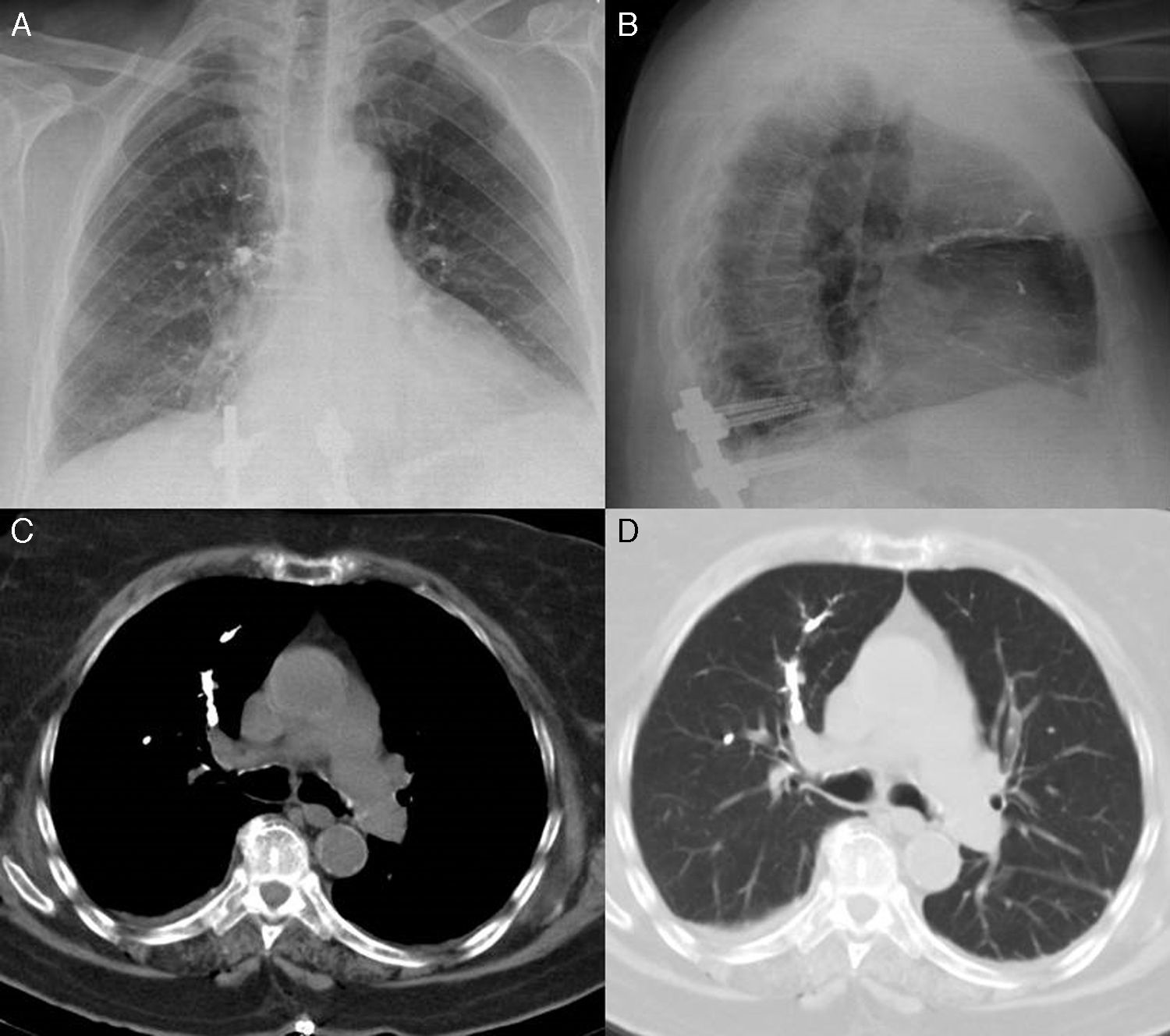
We report the case of a 76-year-old woman, operated 2 years previously for stenosis of the lumbar canal, with sequelae of sagittal imbalance and lumbar pseudoarthrosis. She was hospitalized to undergo T10-S1 arthrodesis with L3 percutaneous vertebroplasty. Six hours after surgery she developed dyspnea, tachypnea, and hypoxemia. On chest radiograph (Fig. 1A and B), dense ramified material was observed in the right upper, middle and lower lung fields and in the left middle field. On chest computed tomography (CT) (Fig. 1C and D), this material occupied the segmental arteries of the right upper, middle and lower lobes and the left upper lobe, and was diagnosed as pulmonary cement embolism (polymethylmethacrylate). She needed high-flow oxygen therapy for the first 24h, after which the oxygen component was gradually reduced until withdrawal a few days later. Pulmonary cement embolism is a potential complication after percutaneous vertebroplasty, due to extravasation of the cement injected into the vertebra to the paravertebral venous system, from where it can migrate to the pulmonary arteries.1,2 In cases of asymptomatic or peripheral embolism, the recommended approach is observation. Anticoagulant therapy, or even embolectomy, should be reserved for symptomatic cases or central embolism.2
Posteroanterior (A) and lateral (B) chest radiographs with dense ramified material, associated with cement emboli, in the right upper, middle and lower lung fields and the left middle field. On the chest CT cross-sectional slice (C and D), the same material occupies right upper lobe segmental arteries.
Please cite this article as: Trasancos-Escura C, Pinos-Blanco A. Una causa infrecuente de embolismo pulmonar. Arch Bronconeumol. 2016;52:528–529.