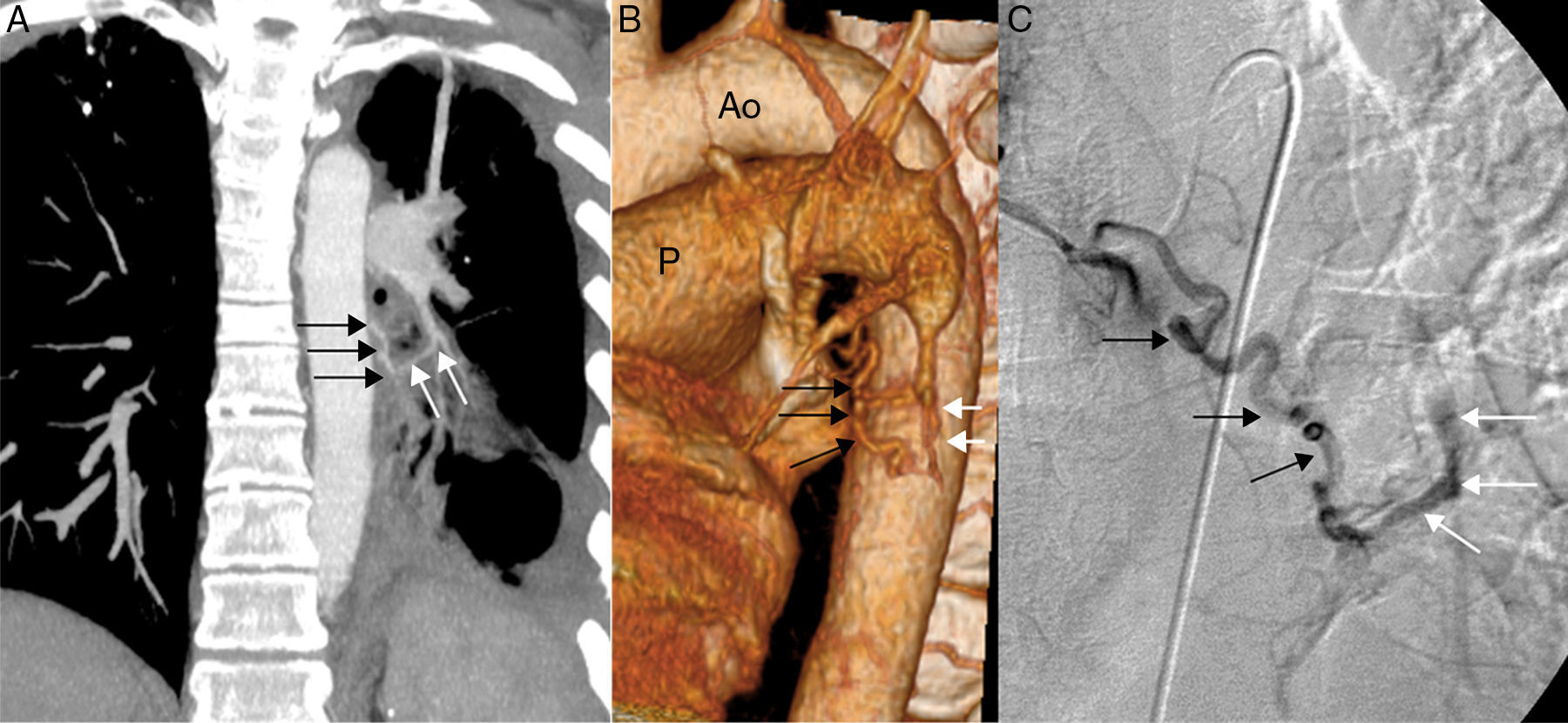
We report the case of a 31-year-old patient with a history of advanced HIV infection (stage C3) with poor therapeutic control, consulting due to hemoptysis. Chest radiograph revealed sequelae from a tuberculosis lung infection involving the left hemithorax in particular. Chest CT angiogram identified a fistula between tortuous, dilated branches of the left bronchial artery and a filiform segmental branch of the left lower lobe pulmonary artery (Fig. 1A and B). Angiogram confirmed the existence of this fistula (Fig. 1C), and embolization was subsequently performed.
(A) Coronal maximum intensity projection (MIP) reconstruction of CT showing a communication between the tortuous branches of the left bronchial artery (black arrows) and a filiform segmental branch (white arrows) of the left lower lobe artery. Note sequelae from tuberculosis in the left hemithorax. (B) 3D reconstruction (volume rendering) of chest CT (Ao: aorta; P: pulmonary artery) providing a better view of the fistula between the branches of the left bronchial artery (black arrows) and the pulmonary artery (white arrows). (C) Angiogram showing retrograde filling of pulmonary arteries (white arrows) from the tortuous branches of the left bronchial artery (black arrows).
Fistulas from bronchial arteries to pulmonary arteries are uncommon left-right shunts and may be congenital or acquired. The most common symptom on presentation is usually hemoptysis, and the treatment of choice is percutaneous embolization. We did not find any cases in the literature describing acquired bronchial artery-pulmonary artery fistula as a cause of hemoptysis in a patient with HIV infection.
Please cite this article as: Gorospe Sarasúa L, Farfán-Leal FE, García-Latorre R. Embolización de fístula adquirida de arteria bronquial a arteria pulmonar en paciente con infección por VIH. Arch Bronconeumol. 2016;52:527.