The aims of this study were to design a best fit linear regression model to estimate VO2max (estimated VO2) and to compare the ability of VO2 values (measured and estimated) predicting cardiorespiratory complications in a series of patients undergoing lung resection for lung cancer.
MethodThis was a prospective, observational study performed in 83 patients. Variables analyzed were: demographic characteristics, comorbidity, body mass index (BMI), FEV1%, FVC%, diffusion capacity (DLCO%), mean daily distance walked in kilometers, VO2max measured by cardio-pulmonary exercise test (CPET) and postoperative complications. Descriptive and comparative statistical analysis of the variables was performed using the Mann–Whitney test for categorical variables and the Student's t-test for continuous variables. A new linear regression model was designed, where the dependent variable (measured VO2max) was estimated by the distance, DLCO% and age, resulting in the estimated VO2. The predictive power of the measured and estimated consumption was analyzed using the Student's t-test, grouping by the occurrence or absence of cardiorespiratory complications.
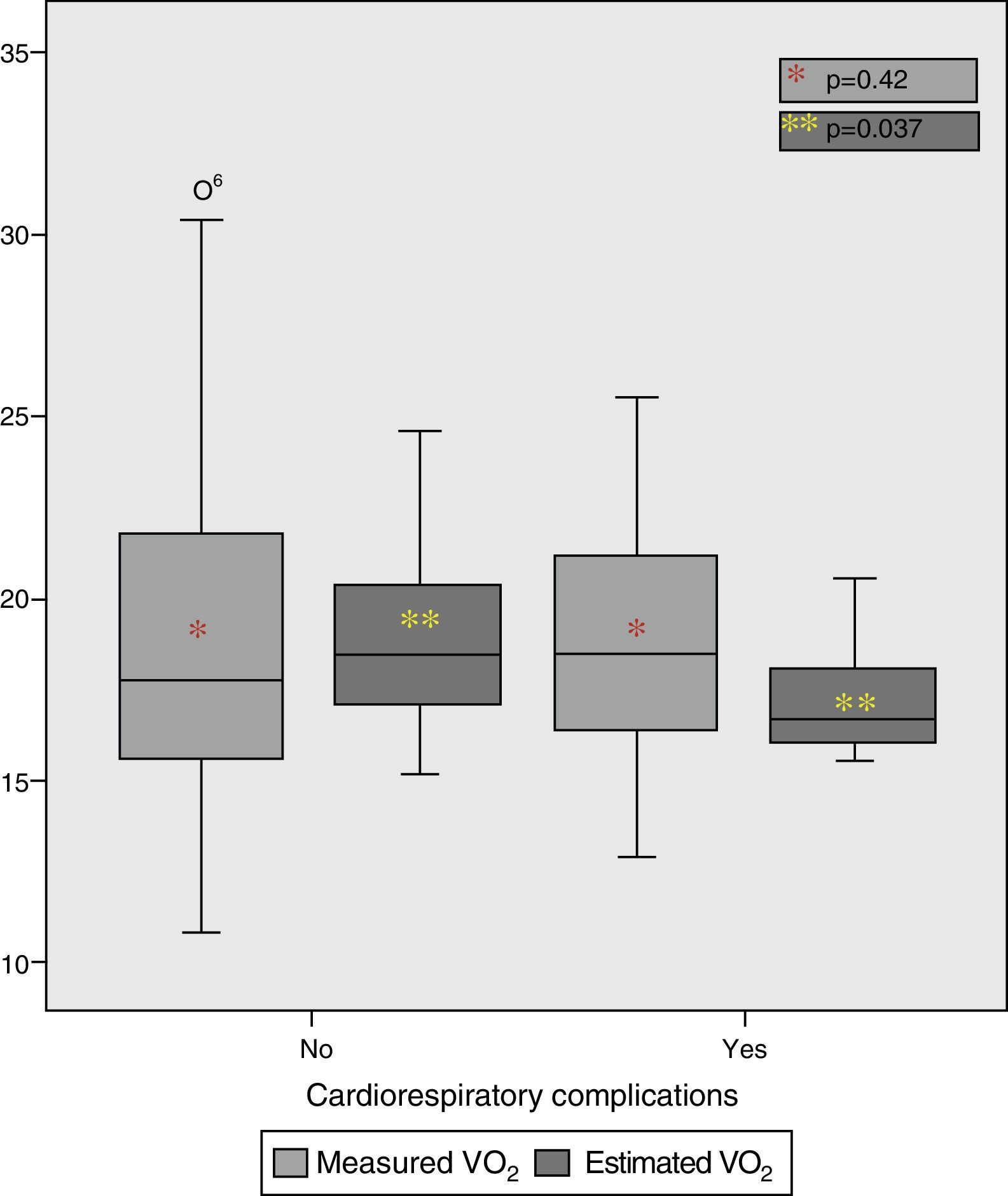
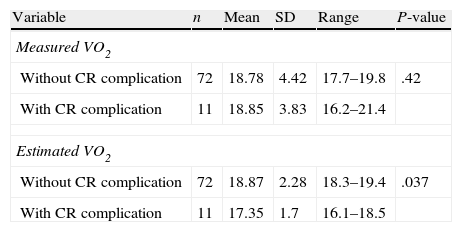
ResultsBoth groups were homogeneous for age, sex, BMI, FEV1%, DLCO%, comorbidity, type of resection performed and mean distance walked per day. Estimated VO2 and measured VO2 were normally distributed (K–Smirnov test, P>.32). VO2 means estimated by the model (age, DLCO% and mean distance walked per day) were significantly different between patients with and without complications (Student's t-test, P=.037) compared with measured VO2 values, which did not differentiate groups (Student's t-test, P=.42).
ConclusionThe VO2max estimated by the model is more predictive in this case series than the VO2max measured during a standard exercise test.
Los objetivos de este trabajo son rediseñar un modelo de regresión lineal para estimar el valor de VO2max (VO2 estimado) ya publicado y comparar la capacidad predictiva de los valores VO2 medido y VO2 estimado en la aparición de complicaciones cardiorrespiratorias en una serie de pacientes sometidos a resección pulmonar por cáncer de pulmón.
MétodoEstudio prospectivo y observacional en 83 pacientes. Variables analizadas: demográficas, comorbilidad, IMC, FEV1%, FVC%, DLCO%, distancia recorrida media diaria (km), VO2max medido en el test de ejercicio cardiopulmonar (CPET) y complicación postoperatoria. Estadística descriptiva y comparativa de variables usando Mann-Whitney test para categóricas y t de Student para continuas normales. Se diseña un modelo de regresión lineal donde VO2max, la variable dependiente, se estima desde la distancia recorrida, DLCO% y edad del paciente y su resultado es la VO2 estimada. Se compara la capacidad predictiva de los VO2max medido y estimado mediante t de Student, agrupando por ocurrencia o no de complicaciones cardiorrespiratorias.
ResultadosLos 2 grupos son homogéneos en edad, distribución de sexos, IMC, FEV1%, DLCO%, comorbilidad, cirugía realizada y distancia media recorrida/día. VO2 medida y VO2 estimada tienen distribución normal (K-Smirnov p>0,32). En la predicción de complicaciones, las medias del VO2 estimado a partir del modelo son significativamente diferentes entre los pacientes con/sin complicación (t de Student p=0,037); frente a los valores de VO2 medido que no distinguen grupos (t de Student p=0,42).
ConclusionesEl VO2max estimado por el modelo es más predictivo en esta serie de casos que el VO2max medido en una CPET.
Despite the refinement and adaptation of published algorithms and mathematical decision models,1 prediction of surgical risk is difficult due to selection bias inherent to these models.2 Comprehensive assessment of the cardiorespiratory system using standardized exercise tests provides a lot of information about the physiological status of the patient who is to undergo pulmonary resection.3 Calculation of peak exercise oxygen consumption (VO2max)4 is considered the most reliable test to quantify individual risk for postoperative complications. However, this technique is not available in all centers performing lung surgery, and it cannot be applied in all patients.5 The reasons are physical or medical contraindications, or structural problems in hospitals where it is implemented.
Among other options, performance at symptom-limited stair-climbing test has shown the best correlation with surgical morbidity,6 although its poor standardization and the difficulty for performing the test in a safe environment for the patient prevent routine use.
A previous study seeking possible alternatives7 found a correlation between VO2max values measured by standard cardiopulmonary exercise test (CPET) and VO2max values estimated with a regression model that included measurement of average distance (km) the patient walked each day, collected with a pedometer during the preoperative waiting period, and carbon monoxide diffusing capacity (%DLCO) adjusted for the patient's hemoglobin levels.
The objectives of the present study were to improve the previously designed linear regression model, in order to find the best correlation between oxygen consumption values (measured VO2 and estimated VO2), and to compare the ability of these two variables to predict the occurrence of cardiac complications in a series of patients undergoing anatomic pulmonary resection for lung cancer.
MethodsWe conducted a prospective, observational study of repeated measures for each subject before and after lung resection.
Study PopulationNinety-five patients were initially included in the study, of which 12 were excluded due to inability to perform exercise testing because of joint problems that prevented smooth pedaling (n=7), vascular comorbidity (presence of aorta aneurysm and recent treatment for deep venous thrombosis; n=2), a vasovagal episode prior to the exercise test (n=1) or because of technical issues with the pedometer that prevented correct measurement of ambulatory activity (n=2).
The final sample included 83 consecutive patients with non-small-cell lung cancer scheduled for major anatomic lung resection (typical segmentectomy, lobectomy, bilobectomy or pneumonectomy) from May 2009 to December 2011, who agreed to be included in the study and signed informed consent. All patients who, due to limitation or contraindication, were not able to properly perform the CPET were excluded. Inclusion of patients with ischemic heart disease was conditional on the existence of a previous coronary revascularization or evidence of good functional capacity, demonstrated by exercise testing or equivalent examination.
The criteria for operability in this study have been previously published8: absence of a comorbidity of worse prognosis than cancer, Karnofski index >50%, estimated postoperative forced expiratory volume in one second (FEV1) greater than 30%, and estimated postoperative DLCO greater than 40%.
All patients were treated by the same multidisciplinary team and operated via axillary thoracotomy without muscle section, in which a 2-cm auxiliary incision was also performed.
Measurement of Maximum Oxygen ConsumptionCardiopulmonary exercise testing was carried out in the Respiratory Functional Test laboratory using the cardiopulmonary exercise test module (ergospirometry) MasterScreen CPX Jaeger-Vyasis-Healthcare, which enables the measurement of ventilatory parameters, VO2, carbon dioxide production (VCO2), anaerobic threshold, respiratory exchange ratio (RER), heart rate (HR), ventilatory equivalent for oxygen (EQO2), and ventilatory equivalent for CO2 (EQCO2) in an open “breath-by-breath” type system.
The CPET modality used in our center is the symptom-limited incremental exercise test. In this modality, the patient performs exercise on a bicycle ergometer with continuous load increases over a period of about 10min (according to Wasserman protocol).9
Measurement of Daily Physical Activity by PedometerAn OmronWalking Style Pro HJ-720IT-E2 pedometer was used with the Bi-Link downloadable software specific to this supplier.
In the first visit, the pedometer the patient would use until the day of surgery was programmed with the date, time and footstep length. Participating in this study did not involve lengthening the preoperative waiting time.
For analysis, the activity recorded by pedometers was reviewed on a case-by-case and day-to-day basis, excluding from the calculation of parameter means those days without any registered activity because the patient did not use the pedometer.
Postoperative ComplicationsData on the type of surgery, occurrence of postoperative complications and type of complications were collected during hospital stay. Complications were grouped into those of cardiac, respiratory or technical nature.
Study VariablesAll variables were prospectively collected in a computerized database:
- -
Patient variables: age, gender, body mass index (BMI), forced vital capacity (FVC), %FEV1 and %DLCO (with optimized bronchodilator treatment, if necessary); comorbidities: systemic hypertension (HT), ischemic cardiovascular disease, diabetes mellitus (DM), chronic renal failure (creatinine >2mg/dl), cardiac valve disease, and/or chronic arterial disease.
- -
CPET variables: patient–weight adjusted VO2peak (ml/kg/min) in absolute values and percentage.
- -
Pedometer variables:
- •
Total number of steps per day or “total steps”.
- •
Number of aerobic steps per day or “aerobic steps”. This count activates when the wearer has walked over 10min at a minimum rate of 60 steps per minute and inactivates if the wearer rests for more than 1min.
- •
Ambulatory activity time in minutes per the day or “time”, divided into total activity and aerobic activity.
- •
Distance traveled during daily activity in kilometers or “distance”.
- •
- -
Postoperative complications:
- •
Respiratory: lobar/pulmonary atelectasis, pneumonia according to Center for Disease Control/National Healthcare Safety network criteria,10 persistence of respiratory failure at discharge (PO2<60mmHg or PCO2>45mmHg), need for mechanical ventilation at any time after extubation in the operating room, and occurrence of pulmonary thromboembolism.
- •
Cardiovascular: occurrence of stroke, arrhythmia (auricular fibrillation, AF), myocardial ischemia or acute myocardial infarction, and heart failure.
- •
Technical: need for reoperation for massive hemothorax, occurrence of prolonged air leak or bronchial fistula within the first week after resection.
- •
Descriptive and comparative statistical analysis of the study variables was performed.
After a correlation analysis between variables, a linear regression model was designed, where VO2max was the dependent variable, and the variables distance traveled, %DLCO and patient age were set as independent variables. The outcome variable in this model was estimated VO2. Bootstrap technique with 1000 replications was performed to study collinearity and perform resampling, in order to obtain a more robust standard error of the coefficients values. Finally, occurrence of postoperative morbidity and mortality and their relationship with VO2max values, both the measured values and the values estimated with the predictive model developed, were analyzed using paired Student's t-test. These analyses were performed using the statistical software Stata 10.0.
ResultsFinal Study PopulationThe final study population was 83 patients, of whom 15 were women (18.1%). Population age was 64.59±9.5 (38–80 years). Twenty patients (24.1%) were being treated for hypertension, 18 (21.7%) met criteria for COPD and were receiving bronchodilators, nine (10.8%) had DM, six (7.2%) significant peripheral artery disease, five (6%) stable ischemic heart disease, and one patient (1.2%) had renal failure not needing dialysis but strict medication adjustments. None of the patients had associated valvular pathology.
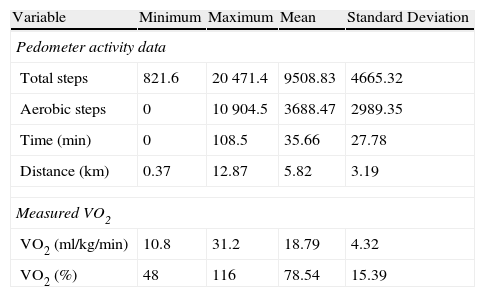
Patients wore the pedometer for an average of 25 days (range 5–41 days) (Table 1), showing a routine in the schedules and time periods they usually walked. All patients performed the CPET according to protocol.
Characteristics of Pedometer-recorded Activity and CPET-measured Oxygen Consumption by Study Population.
| Variable | Minimum | Maximum | Mean | Standard Deviation |
| Pedometer activity data | ||||
| Total steps | 821.6 | 20471.4 | 9508.83 | 4665.32 |
| Aerobic steps | 0 | 10904.5 | 3688.47 | 2989.35 |
| Time (min) | 0 | 108.5 | 35.66 | 27.78 |
| Distance (km) | 0.37 | 12.87 | 5.82 | 3.19 |
| Measured VO2 | ||||
| VO2 (ml/kg/min) | 10.8 | 31.2 | 18.79 | 4.32 |
| VO2 (%) | 48 | 116 | 78.54 | 15.39 |
Seventeen typical segmentectomies, 61 lobectomies, three pneumonectomies and two bilobectomies (one right and one left) were performed.
There was no mortality in this series. In terms of morbidity, 26 patients (31.3%) experienced a complication: eight (9.6%) were respiratory, one (1.2%) was a cardiac complication (arrhythmia), two patients had concomitant cardiac and respiratory complications, and 15 patients experienced technical complications (18.1%), mainly prolonged air leak.
Preliminary Design Correlations and Linear Regression ModelWe analyzed the possible correlations between the recorded lung function variables and aerobic activity with VO2max and VO2peak data.
In this series, VO2max was significantly associated with age (r=−0.451, P=.000), BMI (r=−0.357, P=.001), DLCO (r=0.238, P=.030), number of total steps/day (r=0.278, P=.011), and distance traveled/day (r=0.315, P=.004), but not with %FEV1 (r=0.182, P=.1), presence of COPD (r=0.088, P=.431), aerobic steps/day (r=0.151, P=.173) or the total time of aerobic activity (r=0.117, P=.294).
%VO2 was significantly correlated only with %FEV1 (r=0.303, P=.006), DLCO (r=0.390, P=.000), and the number of total steps/day (r=0.244 steps, P=.027).
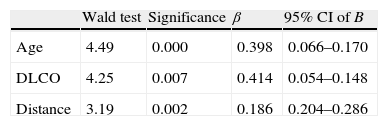
After analyzing the correlations between variables, the final linear regression model with VO2max and %VO2 as dependent variables included those variables with the highest correlation with the dependent variable and showing no collinearity between them.
Of the models developed for %VO2 and for VO2max, the best fitting was related to the estimated VO2max values (dependent variable) and included as independent variables age, DLCO and distance traveled (Table 2). Discriminant analysis for collinearity was performed and none of the variables were related to the others (collinearity index <15 in all variables).
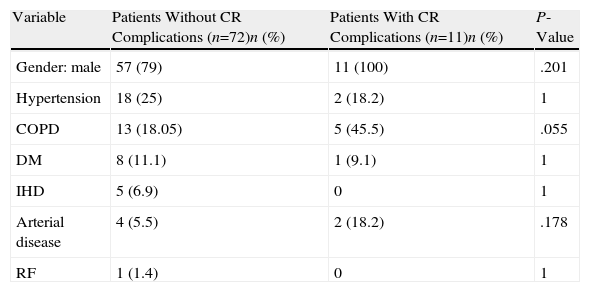
Population Analysis According to Occurrence of Postoperative Cardiac ComplicationsThe two groups into which the population was divided were homogeneous (Table 3).
Comparison of Occurrence of Postoperative Cardiac Complications (CR) in the Two Study Subpopulations.
| Variable | Patients Without CR Complications (n=72)n (%) | Patients With CR Complications (n=11)n (%) | P-Value |
| Gender: male | 57 (79) | 11 (100) | .201 |
| Hypertension | 18 (25) | 2 (18.2) | 1 |
| COPD | 13 (18.05) | 5 (45.5) | .055 |
| DM | 8 (11.1) | 1 (9.1) | 1 |
| IHD | 5 (6.9) | 0 | 1 |
| Arterial disease | 4 (5.5) | 2 (18.2) | .178 |
| RF | 1 (1.4) | 0 | 1 |
| Mean (DE) | Mean (DE) | P-Value | |
| Age | 63.8 (9.3) | 69.2 (8.8) | .08 |
| IMC | 26.7 (4.7) | 23.9 (4.3) | .78 |
| %FEV1 | 85.1 (20.3) | 77.5 (24.5) | .26 |
| %FVC | 96.4 (19.1) | 100.2 (19.1) | .53 |
| %DLCO | 78.2 (20.1) | 66.78 (20.5) | .08 |
| Total footsteps | 9511.2 (4701.3) | 9493.2 (4641.5) | .99 |
| Aerobic footsteps | 3750.6 (2921.1) | 3281.5 (3533.5) | .63 |
| Time | 36.1 (26.9) | 32.6 (34.2) | .69 |
| Distance | 5.9 (3.2) | 4.9 (3.03) | .349 |
Both variables (measured and estimated VO2) were normally distributed (K–Smirnov P>.32).
As for prediction of complications, mean estimated VO2 according to the model was significantly different between patients with/without complication (P=.037), compared to measured VO2 values, which did not distinguish these groups (P=.42) (Table 4 and Fig. 1).
Numerical Values of Mean Oxygen Consumption by Groups According to Occurrence of Cardiopulmonary Complications (CR).
| Variable | n | Mean | SD | Range | P-value |
| Measured VO2 | |||||
| Without CR complication | 72 | 18.78 | 4.42 | 17.7–19.8 | .42 |
| With CR complication | 11 | 18.85 | 3.83 | 16.2–21.4 | |
| Estimated VO2 | |||||
| Without CR complication | 72 | 18.87 | 2.28 | 18.3–19.4 | .037 |
| With CR complication | 11 | 17.35 | 1.7 | 16.1–18.5 | |
The main objective of this study was to design a method for predicting the patient's VO2 from variables easily obtained in all patients, and to analyze its predictive capacity for the occurrence of cardiac complications after lung resection.
The model developed had R2=0.94, meaning a very good fit. The three variables included are age, %DLCO and average distance traveled per day. The inverse relationship between age and VO2 is well known,11 and inclusion of this variable into the analysis improves the result. Both %DLCO adjusted for the patient's hemoglobin and the average distance traveled per day in kilometers were already part of the previously published model.7 Inclusion of these two variables represented an innovation in the variables that had been used to estimate the VO2 in other studies.12–14 In this analysis, as in the previous one,7 we chose to use the variable “distance” instead of “total steps” because its correlation index with VO2 was better (r=0.315 vs r=0.278). There are two reasons for including %DLCO: first, this parameter proved to be correlated with age (r=0.245) and VO2max (r=0.238) and, second, because %DLCO is an accepted independent predictor of postoperative complications.15
The second objective was to analyze the predictive ability of these two variables of oxygen consumption: the measured one and the estimated one. In our analysis, predictive ability is significantly better in the estimated model. Analyzing the performance of average values in the different groups, two aspects draw attention (Table 4 and Fig. 1): first, the difference between groups with/without complication is very small in both measurements; second, measured VO2 has very similar values, and non-discriminating between the two groups because the ranges of measurements are very wide, unlike estimated VO2 values whose ranges are much narrower and probably confer a predictive advantage. A recent meta-analysis of Benzo et al.16 including 14 studies with 955 subjects found that patients with postoperative complications had significantly lower oxygen consumption than those who did not. However, average difference was only 3ml/kg/min or 8.95% between the two groups. The authors concluded from this analysis that patients with consumption over 20ml/kg/min had a very low complication rate. This did not mean that complications would not occur, only that in case of occurrence, they had a better chance of survival. Interestingly, the range of values of measured VO2 in patients who experienced complications in our study was higher than in those who did not (17.7–19.8 vs 16.2–21.4) and mean values were similar (18.75 vs 18.85; P=.42). However, the ranges of estimated consumption values are less wide (18.3–19.4 vs 16.1–18.5) and means were significantly different (18.87–17.35; P=.037). In the meta-analysis,16 the lower threshold associated with a high complication rate is 16ml/kg/min, and this is 17.35ml/kg/min in our patients, slightly higher but within the range of values published in studies analyzed.
Although the comparison of the characteristics of these two subpopulations of patients—those who experience complications and those who do not—yields two statistically similar groups, patients who experience more complications have older mean age (63.8–69.2 years) and lower %DLCO (78.2–66.7). These data are consistent with published results regarding the characteristics of patients who experience complications in other series.16
Current clinical guidelines1 for the evaluation of patients eligible for lung resection recommend a final decision based on the CPET results, i.e., according to the VO2max reached expressed as absolute values or percentage (%VO2).
The values on which VO2max depends include age,11 gender,17 previous respiratory disease,18 genetic characteristics,19 and the training degree of the patient,17 among other factors. The training degree is in turn is strongly linked to daily physical activity,20 his/her health status, and mortality,21,22 and may be useful for predicting postoperative adverse events. In this regard, our group has sought an alternative to estimate VO2max value by studying performance at an easy exercise.
Recent studies5 confirm the existence of numerous shortcomings in the implementation of the European functional assessment algorithm published in 2009.1 The major difficulty is conducting high-technology stress testing, since only 84% of operated patients underwent this for various reasons. The same guidelines recognize that the standardized symptom-limited stair climbing test can be an alternative to performing the CPET, helping reduce the number of patients who would require the latter. However, this test has been criticized for its poor standardization and difficulty for performance in a safe place for the patient. In addition, many patients have joint and insecurity problems when climbing stairs, so results can sometimes be suboptimal, as occurs with the CPET, in which some unsatisfactory results may be attributable to the harsh conditions required for its performance.
Patient limitations are one of the root causes for not being able to perform the CPET.7 Cardiovascular contraindications and joint limitations are especially relevant in an increasingly older population, with more associated comorbidity. Overcoming this limitation is difficult, but possibly the solution lies in the development of new simple and safe strategies to measure the exercise capacity of a given patient. This is the case of measurements based on walked distance or the quality of daily exercise that the patient performs in everyday life.
It is not the intention of this study to question the predictive value of the CPET in surgical risk evaluation. At present, the measurement of daily physical activity is not considered a substitute for the formal CPET, but further studies with larger series and patients more functionally compromised might allow may support this as a valid, cost-saving and effective screening test for those patients in which a formal CPET cannot be conducted due to contraindication or limitation, or also as an alternative when CPET is not available in the center.
Our study has some important limitations. On the one hand, the limitation derived from its sample size, which limits the possibilities for statistical study. This reason prevented a division of the sample into two groups: one to create the mathematical model and a second group to assess validity. Analysis of larger series in the future will enable testing of the reliability of the conclusions drawn in this study. This aspect also influences the number of cardiac complications included in the study, experienced by only 11 patients, which also limits the ability to extrapolate the results. Another important limitation of this study is a possible observation bias. The data collected were generated by the patient during everyday life outside the hospital. Therefore, it is not possible to be absolutely certain that this person was wearing the pedometer. However, in order to reduce this bias, special emphasis was made to each patient during consultation on the importance of not letting anyone else from his/her environment use the pedometer. Lastly, the findings may be affected by case-selection bias, since it was not possible to obtain data from patients who were not considered candidates for surgery, thereby not eligible for this study, due to the selection criteria of the physicians who refer patients to our unit.
In conclusion, the VO2 value of a given patient can be reliably estimated from age, %DLCO and average walking distance per day, measured with a pedometer. In this series, estimated VO2max was more predictive of the occurrence of cardiac complications than VO2max measured in a standard exercise test. Our next objective will be the validation of this model in a larger series and with a broader patient profile.
Conflicts of InterestThe authors declare no conflict of interest that might cause a bias in this study.
Please cite this article as: Vargas Fajardo MdC, Novoa Valentín NM, Jiménez López MF, Ramos Gonzalez J, Varela Simó G. Un método alternativo para la predicción del riesgo de complicaciones postoperatorias en la resección pulmonar. 2014;50:87–92.