Malignant airway obstruction (MAO) often complicates the course of oncological diseases, specially lung cancer. Bronchoscopic evaluation and intervention is of utmost importance in MAO management.1 In selected cases, airway stenting is needed to maintain airway patency either in a purely palliative setting or as a bridge until adequate response to systemic treatment is achieved. Silicone stents can only be placed by rigid bronchoscopy under general anaesthesia, but are easy to remove.2 However, stent-related complications are not negligible and seem to be time-dependent.3 Although yearly switch is recommended by the manufacturer, the real durability of Dumon® stent is unknown. We report a case of a 58 year old female with MAO due to an atypical carcinoid of the lung managed with silicone stent for 16 years.
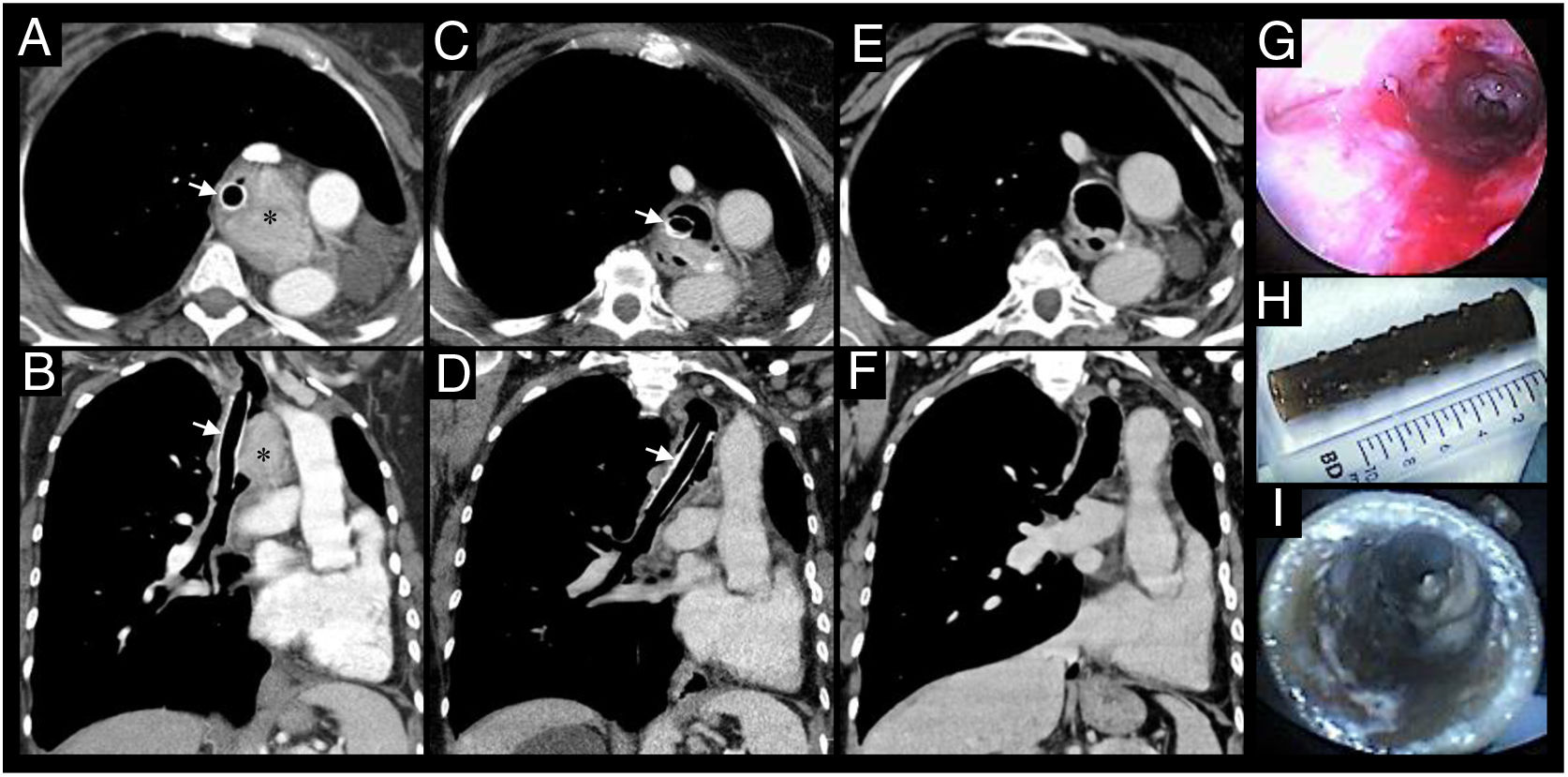
The patient was diagnosed with an atypical carcinoid of the lung at age of 21 and underwent left pneumonectomy. After 18 years, disease recurrence was detected. A thoracic CT scan showed a mass involving the lower third of the trachea and the right main bronchus, causing significant endoluminal airway obstruction (90%). Rigid bronchoscopy was performed and after mechanical debulking, airway patency was still not satisfactory, therefore, a Dumon® stent was placed in the trachea and right main bronchus with clinical improvement. Two years later, she presented in the emergency department with severe stridor. An emergent rigid bronchoscopy showed proximal obstruction of the right main bronchus with tumoral tissue and, after laser therapy and mechanical debulking, a distal stent migration to the right main bronchus was observed. The procedure was complicated by severe haemorrhage leading to respiratory failure requiring mechanical ventilation and subsequent intensive care unit admission. After fourteen days of invasive ventilation and stabilization, the stent was replaced and positioned in distal trachea and proximal right main bronchus. After nine days, she was extubated and discharged to Pulmonology ward. Despite clinical improvement, the patient was diagnosed with critical illness myopathy and polyneuropathy requiring intensive physical rehabilitation. Additionally, distant multifocal metastatic disease including skin and bone was found. Since the tumor revealed positivity for somatostatin receptors in octreotide scan, systemic treatment with somatostatin analogues was initiated. Regular bronchoscopic evaluations were performed showing appropriate stent positioning. Progressive shrinkage of the mass was observed and adequate airway patency was achieved being possible to safely remove the stent after 16 years (Fig. 1). Despite the clinical stability, during this time, the patient experienced severe halitosis with negative impact in her social life and, in the last 2 years of stenting, frequent respiratory infections were observed. Currently, the patient is asymptomatic.
Thoracic CT scan shows an extraluminal mass (*) in previously left pneumoectomized patient causing significant mass effect in the trachea and endoluminal involvement, after mechanical debulking and placement of a Dumon® silicone stent (arrows), axial (A) and coronal (B) views. After systemic treatment, progressive shrinkage of the mass was observed and adequate airway patency was achieved (as seen in C and D) permitting the stent removal. The re-establishment of airway patency after stent removal is showed in CT scan axial (E) and coronal (F) views as well as in bronchoscopy (G). The Dumon® silicone stent removed after several years is showed in H and I.
Airway stenting is indicated in a variety of malignant and benign diseases and has as main function supporting and maintain the airway lumen patency. In malignancy, the indications of its use include airway obstruction either due extrinsic compression or persistence of residual endobronchial lesions after mechanical debulking and/or thermal therapies, cartilage destruction by tumor and tracheoesophageal fistulas.4 Stenting also avoids the tumor re-growth and obstruction recurrence at some extent. Although any type of malignancy may cause airway obstruction, either as primary or metastatic, the most common cause is primary lung cancer.2 The present case reports a malignant airway obstruction caused by an atypical carcinoid, a subtype of neuroendocrine lung tumor. This type of tumors are uncommon and express several pathologic and clinical features that require different treatment strategies.5 Although initially treated radically with pneumonectomy, the local recurrence of the disease demanded combined strategies with bronchoscopic intervention including airway stenting and systemic treatment.
Endoluminal silicone stents were firstly placed by Dumon with the same technique currently used.6 Silicone is a synthetic material that is firm but easily moldable, is stable at high temperatures and well tolerated since it provokes only minimal mucosal reactivity. In general, silicone stent placement is technically complex and requires rigid bronchoscopy under general anaesthesia. However, they have an optimal safety profile, are easy to remove and reposition can be done after endobronchial deployment. Additionally, its customization is easy by cutting the edges before placement.4 The decision of stent placement requires experience and must be individualized and deliberated, since they have potential for complications. One must be aware that the intention of stent placement is only palliative, either entirely or in a transitory manner while waiting systemic therapies response as seen in this case. Indeed, after disease control, silicone stent was successfully removed. Complications of silicone stents are well described and comprise migration, obstruction from accumulated secretions or granulation tissue growth at the proximal or distal ends, halitosis and, less commonly, respiratory infections, ulcerations and perforations.7 Although the overall adopted treatment strategy was effective and despite frequent clinical and bronchoscopic surveillance, the patient presented significant stent-related complications namely migration, severe halitosis and recurrent respiratory infections, probably associated to long-standing stenting, at least in some degree.3 After stent removal, a significant improvement in patient's quality of life was noticed.
Despite evident and potentially life-threatening complications, adequate airway patency was achieved and the silicone stent was tolerated for 16 years under periodic clinical and bronchoscopic surveillance. This case reflects the clinical challenge behind a successful management of MAO, which led to an exceptionally long-lasting silicone stent. Still, the Dumon® silicone stent was safely removed after several years which suggests that it may be more durable than expected as previously reported.8
Statement of EthicsThis report was approved by Ethics Committee of Centro Hospitalar e Universitário de São João and conducted in accordance with a declaration of Helsinki.
FundingNone.
Conflict of InterestThe authors declare no conflict of interests.