Once respiratory muscle impairment has become pronounced, patients with neuromuscular disorders (NMD) can use non-invasive ventilation (NIV) to reduce symptoms related to CO2 retention, improve functional status and quality of life (QoL) [1]. As respiratory conditions worsen, patients may require more extensive ventilatory support and transition from nighttime only to full time ventilator use, usually when experiencing daytime respiratory discomfort [2]. For some patients, nasal interface can be a comfortable option for daytime NIV, especially if they are able to tolerate it without skin breakdown. Other patients may use a nasal or oronasal interface for nighttime and switch to a mouthpiece for daytime use. In both cases, they experience limitations in their ability to perform daily activities, including communicating, eating or grooming. For this reason, finding a viable alternative to NIV to assist ventilation during daytime is a crucial point.
A 47-year-old female patient with severe Fukuyama congenital muscular dystrophy, a professor at our University, was evaluated at the outpatient clinic of the Respiratory Pathophysiology Division of the University of Padua. She had been using home NIV via a nasal mask for 15 years prior to our clinical evaluation and regularly underwent lung recruitment manoeuvres through a mechanical in-exsufflator. She reported a history of progressive respiratory discomfort, fatigue and increasing need for ventilator use which had become necessary not only at night, but also during the day to alleviate symptoms. However, daytime use of NIV prevented her from giving lectures to her students. At that time, the patient realized that pressing her upper abdomen against the edge of the desk and releasing it rapidly by the wheelchair back and forth motion enhanced speech volume and duration, making it possible to perform uninterrupted lessons without ventilatory support; likewise, this technique enabled her to eat and drink without any assistance from the ventilator. As a result, she decided to use “wheelchair-assisted ventilation” during daytime whenever it was necessary to interrupt NIV. Remarkably, the patient discovered the method spontaneously and it was not a medical recommendation.
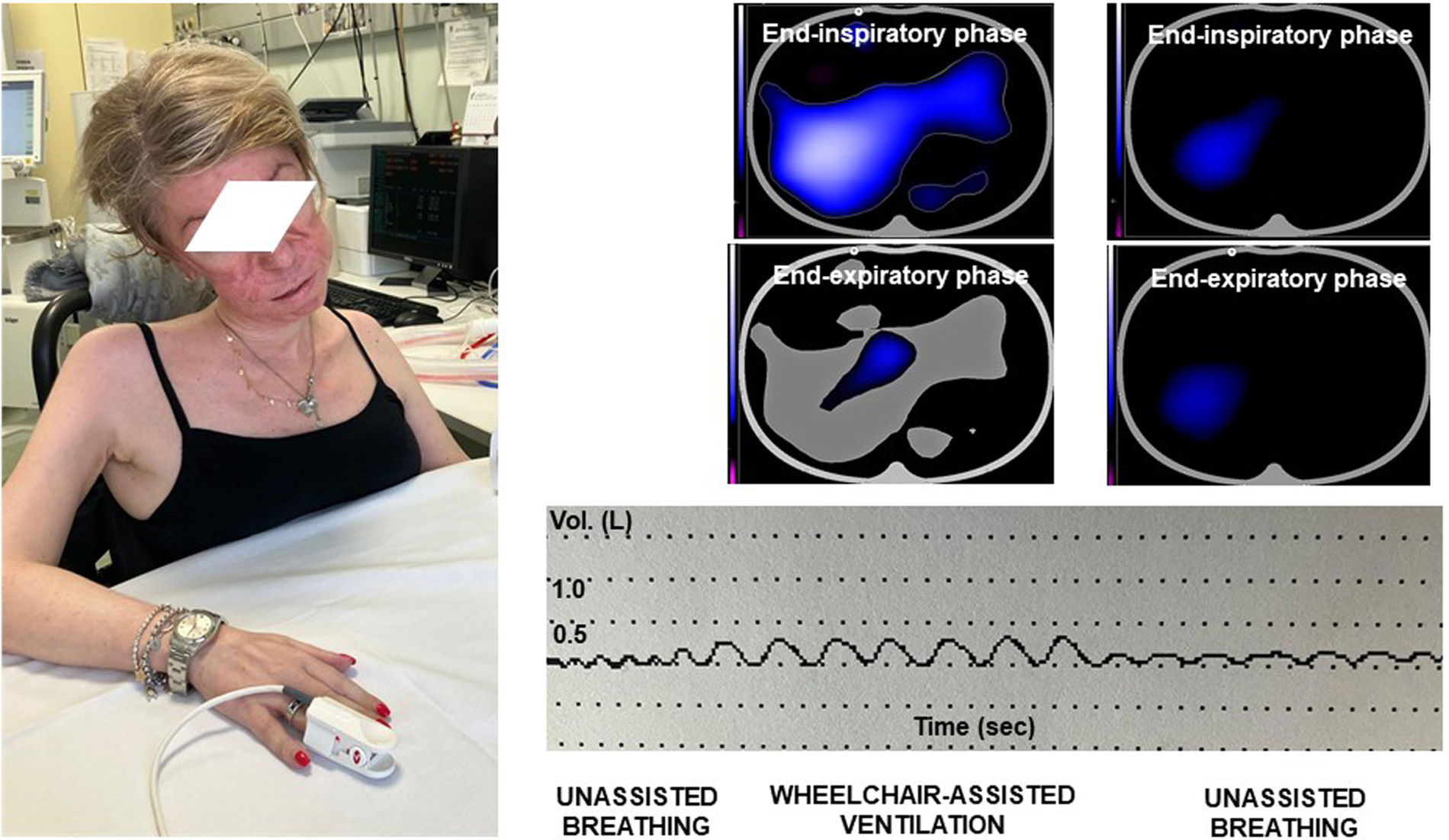
At our pulmonary function laboratory, the patient underwent pulmonary function test including recording of her pattern of breathing by a water-sealed bell spirometer (Baires 80, Biomedin, Padua, Italy) and electrical impedance tomography (EIT), a non-invasive monitoring tool providing continuous transverse images of the lungs, allowing a breath-to-breath evaluation of lung ventilation [3] (PulmoVista® 500, Dräger Medical GmbH, Lübeck, Germany). Her forced vital capacity (FVC) was found to be equal to 0.3L. Arterial blood gas analysis showed normal values (PaO2: 78mmHg; PaCO2: 44.5mmHg; pH: 7.40; SaO2: 96%). After discontinuing NIV through oronasal mask, the patient could sustain unassisted breathing for about 90s before the onset of respiratory discomfort. We found that tidal volume increased from 0.1L during unassisted ventilation to 0.35L during wheelchair-assisted ventilation at a respiratory rate of approximately 20cycles/min (Fig. 1). Moreover, EIT showed a partial re-expansion of both lower lobes during the procedure (Fig. 1). SpO2 value increased from 95% during unassisted breathing to 98% during assisted ventilation.
Similar to what happens during the application of the intermittent abdominal pressure ventilator [4], we hypothesized that compression of the upper abdomen against the edge of the desk could move the diaphragm upward to exhale air from the lungs by an increase in intra-abdominal pressure, whilst during release the diaphragm could return to its resting position due to gravity, thus fostering passive inspiration in combination with elastic return of the rib cage. As a result, we believe that wheelchair-assisted ventilation can effectively support breathing during daytime in NMD patients except for those cases with severe obesity, kyphoscoliosis, previous abdominal surgery, and/or gastroesophageal reflux. Required skills include ability to use commands for the electric wheelchair. Another limitation is that the user needs back extensors, and possibly some hip flexors to do the maneuver, both of which can be severely impaired due to underlying disease. Moreover, the technique cannot be effective in case of acute exacerbation, when patients need to use NIV 24/7 and mechanical in-exsufflation to treat oxygen desaturation. Since this is a single case and no systematic studies on long-term efficacy or safety are currently available, reproducibility and safety require further evaluation before the technique can be recommended. Despite limitations, wheelchair-assisted ventilation may represent a useful option to improve participation in daily activities and quality of life in selected NMD patients.
CRediT authorship contribution statementAndrea Vianello: Conceptualization; writing – review & editing
Gabriella Guarnieri: Investigation; original draft preparation, review & editing
Federico Lionello: Conceptualization, methodology, review & editing
Declaration of generative AI and AI-assisted technologies in the writing processNo content of the manuscript has been partially or totally produced with the help of any artificial intelligence software or tool.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestThe authors declare not to have any conflicts of interest that may be considered to influence directly or indirectly the content of the manuscript.