Postoperative hospital length of stay (LOS) is one of major sources of health care expenditures associated to surgical procedures1–3 making LOS reduction an attractive target for ensuring access to limited inpatient beds and cost reduction per treatment event. Thus, in the recent decades, surgeons and providers have tried to improve cost-effectiveness by decreasing LOS while ensuring high-quality care for patients through different care pathways4 in an era of rising healthcare costs.
Additionally, the value of LOS within a specific diagnostic category may be used as a quality-of-care indicator given that it is correlated with postoperative complications and morbidity5 turning it into a surrogate indicator of case complexity and hospital performance.5,6
Although many studies5,7–10 have reported LOS for pulmonary resection, scanty information is available on time-trending.11 The goal of this study was to evaluate trends in LOS in patients who underwent anatomical lung resection at a high-volume tertiary academic centre over the period between 2011 and 2021 and identifying variables strongly associated to LOS.
A retrospective observation study was conducted. All data were obtained from an institutional prospective, computerized database. Patients older than 18 years who underwent elective anatomical lung resection (segmentectomy, lobectomy, bilobectomy or pneumonectomy) for NSCLC from 2011 to 2021 were identified. The population was divided into three time periods according to the implementation date of new surgical approaches (a fully standardized video-assisted thoracic surgery (VATS) programme was implemented in 2015 while a fully standardized robotic programme was implemented in 2019): 2011–2014, 2015–2018, and 2019–2021.
Postoperative management was uniform for all patients through-out the study period. Nursing care was homogeneous in all cases and included incentive spirometry, early mobilization and standardized intensive physiotherapy as indicated.12 Criteria for discharge remained stable along the study period. At discharge all patients were able to self-assistance, chest pain was well controlled with non-opiates, had no fever and no pneumothorax or large pleural effusion (except in pneumonectomy cases) were seen at chest X-ray. In cases fulfilling previous criteria, prolonged air leak or PO2 under 60mmHg were not considered a contra-indication for discharge and ambulatory chest tube or home oxygen were temporarily indicated.
The dependent variable was postoperative LOS which was defined by the number of calendar days from surgical procedure to hospital discharge. Mean, median, standard deviation, and interquartile range for LOS were calculated in the three periods. As independent variables we considered demographic and clinical characteristics of patients.
The main purpose of the study was describing the LOS trending in all anatomical lung cancer resection over the 2011–2021 period. The secondary endpoint was determining variables associated with LOS and describing trendings in those variables strongly associated to prolonged LOS in the complete series.
First, LOS and postoperative morbidity rates in the three periods were calculated and compared by Kruskal–Wallis and χ2 test, respectively.
LOS was log-transformed to obtain a normal distribution according to Kolmogorov–Smirnov's test and multiple linear regression analysis was used to estimate determinants of its value. The prevalence or mean of factors with the strongest association with prolonged LOS in the complete series were compared in each period by using χ2 test for categorical variables or the one-way ANOVA for continuous variables with gaussian distribution or the Kruskal–Wallis tests for continuous variables with non-normal distribution.
Statistical analyses were performed using the statistical software SPSS 26 (IBM Corp, Chicago, Illinois, 2019).
The series consisted of 1544 cases. Thirteen patients (0.84%) who died before discharge were excluded. A total of 1531 cases were analyzed: 391 cases (2011–2014), 650 cases (2015–2018) and 490 cases (2019–2021).
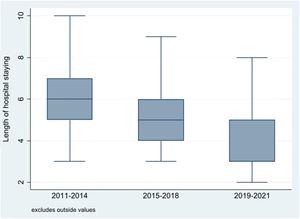
Overall, median LOS was 5 days with interquartile range (IQR) 4–6. Overall mean LOS was 5.53 days with standard deviation (SD) 3.82. Median LOS significantly decreased from 6 days (IQR: 2 days) in the first period to 5 days (IQR: 2 days) in the second period and 3 days (IQR: 2 days) in the third one (p<0.001) (Fig. 1). Overall, 506 patients (33.1%) experienced any postoperative complication. There was a trend towards a decrease in morbidity rates during the last period (34.5%, 35.2% and 29%, respectively, p=0.065).
In the multiple linear regression analysis, LOS significantly correlated with surgical approach (0=thoracotomy, 1=VATS, 2=robotics; β: −0.422; p<0.001), predicted postoperative forced expiratory volume in the first second percentage (ppoFEV1%) (β: −0.111; p<0.001), age (β: 0.111; p<0.001), extended resection (0=no, 1=yes; β: 0.091; p<0.001), predicted postoperative carbon monoxide lung diffusion capacity percentage (ppoDLCO%) (β: −0.090; p<0.001) and sex (0=female, 1=male; β: 0.049; p=0.045).
Time trends of variables strongly associated to LOS showed that minimally invasive approaches (VATS or robotics) significantly increased during the study period (5.9%, 60.8% and 76.9%, respectively, p<0.001) while the rate of extended resections decreased progressively along the three periods (p<0.001). Regarding patients’ characteristics, the rate of female patients increased until reaching 33.5% in the last period and ppoFEV1% significantly improved. No changes were identified in time trend of ppoDLCO% and patients’ age (Table 1).
Time trends of variables significantly associated to LOS.
| Variable | 2011–2014 | 2015–2018 | 2019–2021 | p-Value |
|---|---|---|---|---|
| (n=391) | (n=650) | (n=490) | ||
| Surgical approach, n (%) | <0.001* | |||
| Thoracotomy | 368 (94.1) | 255 (39.2) | 113 (23.1) | |
| VATS | 23 (5.9) | 384 (59.1) | 263 (53.7) | |
| RATS | 0 (0) | 11 (1.7) | 114 (23.3) | |
| ppoFEV1%, mean±SD | 71.79±18.66 | 73.96±19.83 | 75.96±19.29 | 0.008** |
| Age, mean±SD, years | 65.46±8.92 | 66.89±8.88 | 66.12±9.16 | 0.043** |
| Extended resection, n (%) | 45 (11.5) | 31 (4.8) | 19 (3.9) | <0.001* |
| ppoDLCO%, mean±SD | 63.65±15.97 | 65.69±11.44 | 64.69±17.74 | 0.171** |
| Male gender, n (%) | 324 (83.9) | 469 (72.2) | 326 (66.5) | <0.001* |
VATS: video-assisted thoracoscopic surgery; RATS: robotic-assisted thoracic surgery; ppoFEV1: predicted postoperative forced expiratory volume in one second; ppoDLCO: predicted postoperative carbon monoxide lung diffusion capacity.
Our results show that there has been a significant decrease in LOS following anatomical lung resection for NSCLC in the last 11 years, although overall postoperative morbidity remain stable. These findings corroborate the results previously reported by von Meyenfeldt et al.,11 who found a decrease in LOS after lung cancer surgery by more than one day from 2010 to 2015 after analysing data from the Netherlands National Cancer Registry.
During the last period of the study (2019–2021), median LOS was 3 days, pointing out the fact that an early discharge after anatomical lung resection is feasible and safe as it has been proven in previous studies.9,10
With regard to determinants of LOS, twenty years ago, Gagarine et al.3 analysed 360 patients who underwent pulmonary lobectomy between 1998 and 2001 and identified surgeon, age, FEV1% and DLCO as of the variables predicting LOS after pulmonary resection. Our analysis has the advantage of providing a contemporary and generalizable assessment for LOS among a large number of NSCLC patients. Our results identify surgical approach, ppoFEV1%, age, gender, extended resection, and ppoDLCO% as the main determinants of LOS. Minimally invasive surgical approach noticeably increased during the study period from 5.9% in the first period to 76.9% in the last one making surgical approach the strongest variable influencing LOS and the one which experienced a more significant variation along the entire period.
Our findings must be interpreted within the context of the study design. First, the study is retrospective in nature and data were obtained from a single public institution with standardized clinical care pathways. Second, there could be some circumstances not included in the analyses that may influence LOS such as technological surgical or anaesthetic improvements (development of suture or energy devices) or the impact of coronavirus disease (COVID) pandemic.
In conclusion, LOS after anatomical lung resection has progressively decreased over the last 11 years. Surgical approach is the strongest factor influencing LOS and minimally invasive approaches have markedly increased during the last decade.
Funding statementThe authors declare that no financial support was received regarding the content of this manuscript.
Conflict of interestThe authors declare that there is no conflict of interest regarding the content of this manuscript.