Inflammatory bowel diseases (IBD) involve chronic systemic inflammation affecting multiple organs, including the lungs, leading to significant respiratory symptoms affecting patient's quality of life.1
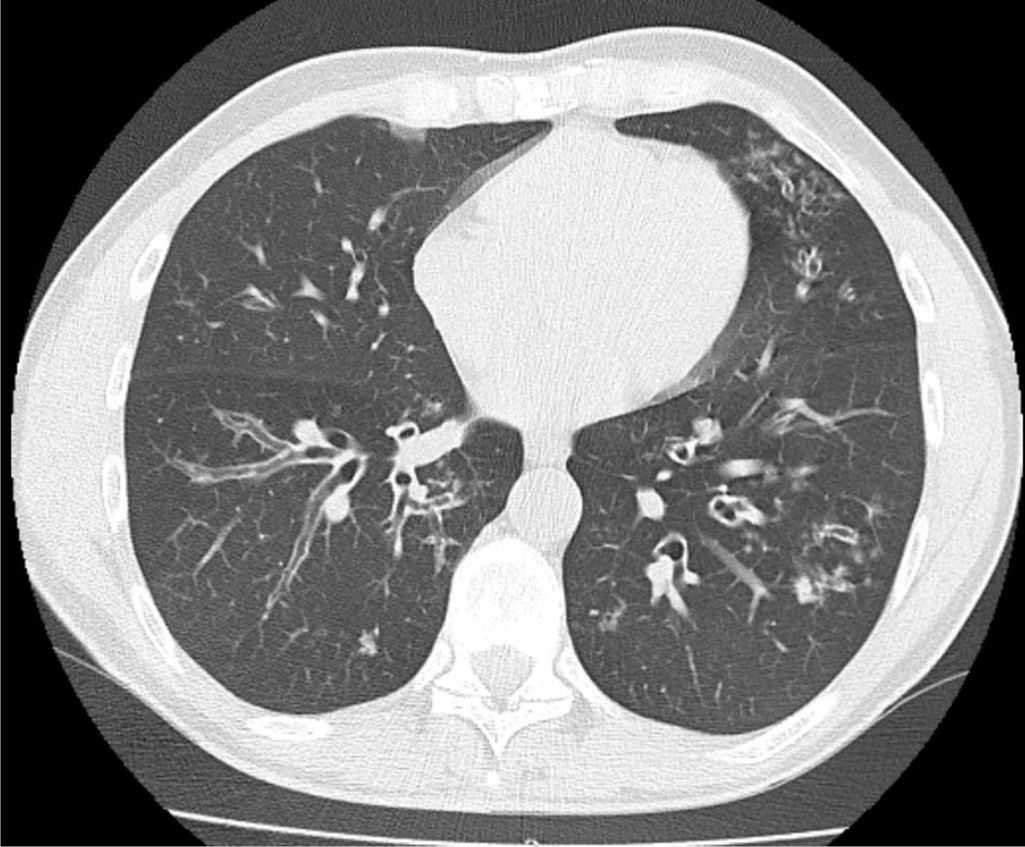
We present the case of a 42-year-old man non-smoking diagnosed with ulcerative colitis (UC) in 2004, primarily with rectal involvement, under IBD Unit follow-up. He experienced multiple outbreaks of the disease, requiring repeated corticosteroid therapy. In 2017, symptom control was achieved with vedolizumab, but the same year, he developed for the first time respiratory symptoms and chest computed tomography (CT) showed bilateral cylindrical bronchiectasis (Fig. 1).
The patient faced several episodes of bronchiectasis superinfection without identifiable microbiological causes. By late 2022, he transferred to our hospital for specialized follow-up. Initially, he reported shortness of breath, cough, and significant sputum production. Immunomodulatory treatment with daily azithromycin 250mg was attempted but was discontinued due to poor tolerance, as was inhaled gentamicin 80mg every 12h. He was on a long-acting β-adrenoceptor agonist (olodaterol) and long-acting muscarinic agonist (tiotropium bromide) bronchodilator therapy and inhaled corticosteroid (mometasone), performing respiratory physiotherapy, and nebulizing with 7% sodium chloride and hyaluronic acid after short-acting bronchodilator inhalation. He experienced in this year two exacerbations treated with oral antibiotics.
By February 2023, a multidisciplinary session indicated intestinal inflammation control. However, respiratory symptoms worsened, prompting a switch from vedolizumab to tofacitinib (5mg every 12h), based on a similar case in the literature.2 Subsequent follow-ups showed significant improvement in respiratory symptoms, from 2 to 0 in the mMRC (Modified Medical Research Council) Dyspnea Scale. His COPD Assessment Test (CAT) score decreased from 26 to 6 after nine months. Additionally, there was a reduction in oral antibiotic (just one exacerbation required it) and oral corticosteroid use and inhaled corticosteroid dose; improvement in respiratory function tests (FVC increased from 3289ml (63%) to 4550ml (90%) and FEV1 from 2240 (54%) ml to 3060ml (75%)) and digestive symptoms.
Extraintestinal manifestations of IBD can occur alongside disease flares or independently.2 IBD patients are more susceptible to lung issues, often underdiagnosed. UC presents extraintestinal manifestations in about 31% of cases, with respiratory symptoms being more common than Crohn's disease.3
Bronchiectasis is the most frequent pulmonary complication, typically manifesting as cough, sputum production and breathlessness. Diagnosis is confirmed via thoracic CT.1 Current treatments include inhaled corticosteroids, with oral corticosteroids for severe cases. Immunomodulators and biological therapy are third-line treatments.3
The worsening of respiratory symptoms following vedolizumab raises questions about a possible association between the drug and pulmonary complications. Literature reports cases of respiratory issues in patients on vedolizumab, with symptoms improving after discontinuation.4
León-Ramón et al. describe a UC patient who developed bronchorrhea and bronchiectasis after starting vedolizumab and showed improvement with the compassionate use of tofacitinib, an oral Janus kinase (JAK) inhibitor targeting four intracellular tyrosine kinases – JAK1, JAK2, JAK3 and the non-receptor tyrosine kinase 2 protein – that activate immune mediators implicated in IBD pathogenesis.2,5
This case highlights the need for studies on tofacitinib's role in extraintestinal respiratory manifestations of IBD, particularly bronchiectasis, as it significantly affects patients’ quality of life.
Artificial Intelligence InvolvementNo participation of artificial intelligence on this article.
FundingNo funding related to this article.
Conflicts of InterestNone declared.