As of 4 June 2020, the number of confirmed cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in Spain is 240,326, many of whom have developed the coronavirus disease 2019 (COVID-19).1 Despite the high number of deaths (around 27,000), more than 120,000 patients have been cured.1 Once the outbreak is over, the new situation we face is dealing with non-related COVID pathologies in patients diagnosed with COVID-19 or who have recently overcome the disease.
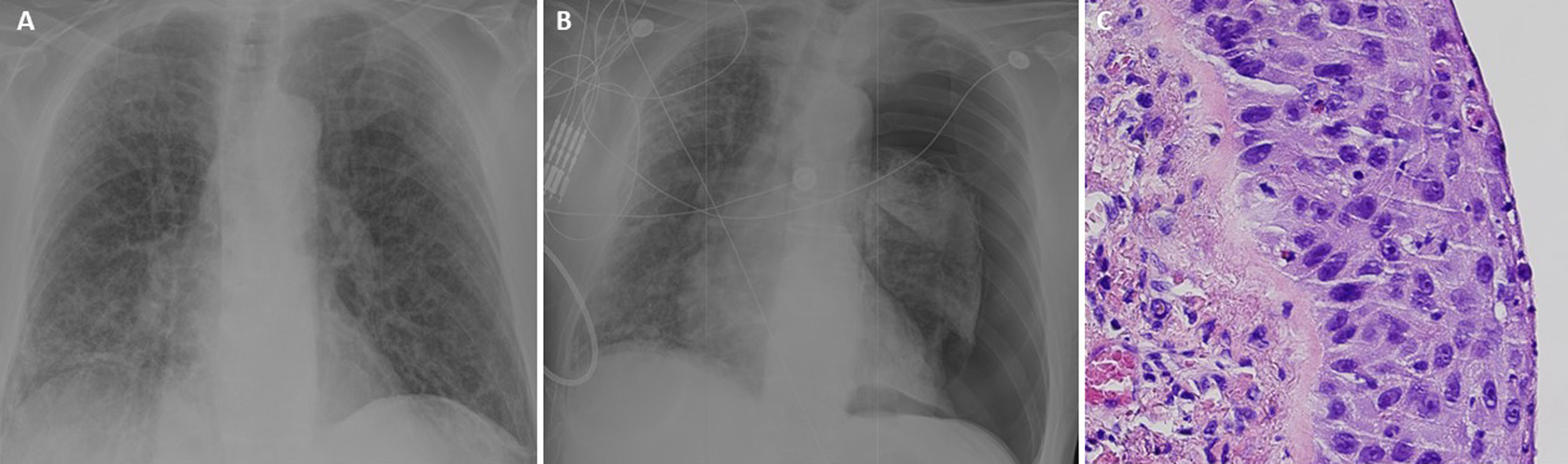
A 78-year old former smoker (cumulative cigarette smoking more than 30 pack-year) patient with medical history of chronic obstructive pulmonary disease (COPD) type emphysema (forced expiratory volume in the first second (FEV1)/forced vital capacity (FVC): 46%, FEV1: 70% and carbon monoxide diffusing capacity (DLCO): 49%) under bronchodilator treatment and periodical follow-up by a pulmonologist was admitted in a non-tertiary care hospital due to dyspnea, cough, myalgia and fever. The patient presented an acute respiratory failure with hypoxemia and hypocapnia. The polymerase chain reaction (PCR) microbiological test in nasopharyngeal exudate revealed SARS-CoV-2 nucleic acid and the chest radiography showed right basal opacities and a diffuse interstitial bilateral pattern (Fig. 1A). The patient was diagnosed with COVID-19 pneumonia and he was treated with hydroxychloroquine, lopinavir/ritonavir, interferon beta, corticoids and non-invasive ventilation. After 10 days of hospitalization, the patient was discharged with home oxygen and the recommendation of solitary confinement for 14 days. During the 4th day of individual isolation, he developed acute dyspnea and chest pain and he was transferred to the hospital again. A left complete pneumothorax was seen in the chest radiography (Fig. 1B). A 20F chest tube was inserted and a continuous 3/5 air leak was observed in the analogic drain. The patient was kept in isolation in a COVID-19 restricted area. After 6 days of prolonged air leak and incomplete pulmonary expansion, his general surgeon contacted us to transfer the patient to our third-level university hospital for surgical treatment.
(A) Chest radiography showing right basal opacities and a diffuse interstitial bilateral pattern compatible with COVID-19. (B) Chest radiography showing q left complete pneumothorax and persistence of the radiological changes due to the COVID-19. (C) Microscopical detailed view of atypical cellularity with a high mitotic index (squamous cell carcinoma).
To avoid virus spread, the procedure to transfer a patient from one to another hospital must follow all security protocols. So that, before transferring the patient we performed a new PCR test with a negative result. Once here, since the patient had not complied the 14 days of individual isolation after discharge, a serologic test was ordered to verify if the infection was active or passed; the result was positive, but unfortunately there was no possibility to know about which kind of immunoglobulins was elevated (Ig G or Ig M) due to the lack of reactants. So that, a new PCR test was performed to confirm the previous one with a delay less than 48h. The result was negative. Regarding the two last negative tests and the time interval since the first positive test (more than three weeks), the patient was considered as a SARS-CoV-2 negative patient and treated with comprehensive protective measures but without strict isolation in the ward.
The patient underwent video-thoracoscopic surgery. A 2mm perforation was found in the left segment six in an emphysematous area and a wedge resection and chemical pleurodesis were performed. The patient was discharged the day after the operation with no complications. The anatomopathological report revealed a keratinizing squamous cell carcinoma in situ in an emphysematous bulla with free surgical margins (Fig. 1C). Non-tumoral parenchyma characterized by the subpleural cyst wall thickness.
After complete recovery of the patient, a thoraco-abdominal computerized tomography (CT) and a positron emission tomography-CT (PET-CT) were performed. No distant metastases or nodal disease were detected. Final staging was pTisN0M0 (stage 0).
As thoracic surgeons the new scenario we face is treating COVID-19 patients or patients who recently overcome the disease who present with non-related COVID-19 pathology which require urgent or preferential thoracic surgical intervention. A recent study has demonstrated that postoperative pulmonary complications occur in half of patients with perioperative SARS-CoV-2 infection and are associated with high mortality.2 Moreover, Li et al.3 concluded that COVID-19 is associated with poor prognosis for patients undergoing thoracic operation, especially for those with COPD. So that, unnecessary thoracic surgeries should be avoided. Besides, since it is imperative to ensure the safety of health-care workers not only to safeguard continuous patient care but also to ensure they do not transmit the virus, high-sensibility diagnostic tests should be routinely performed to identify current and past infection (serologic tests) and to ensure that patients who have overcome the disease are no longer contagious (nucleic acid tests).
Until a few days ago, only urgent procedures and high priority oncological elective surgery in non-COVID-19 patients were performed and always balancing the risk of delaying therapy against the availability of hospital resources and potential exposure of COVID-19 on a case-by-case basis. In addition, whenever possible, the elective surgical activity has been transferred to COVID-free areas to avoid potential contracting intra-hospital infections. Since previous reports have revealed that there are asymptomatic patients infected with SARS-CoV-2,4,5 all patients needing a surgical intervention should be tested.
We report the case of a patient presented with left spontaneous pneumothorax after discharge for COVID-19 pneumonia that was managed surgically. We consider this therapy was non-delayable and, after microbiological verification of SARS-CoV-2 negativity, excision of a perforated bulla was performed. Pathological examination of the specimen revealed a lung carcinoma in situ whose prognosis is excellent.
Funding sourceNone.
Conflict of interestThe authors declare that they have no conflict of interest related directly or indirectly to the contents of the manuscript.