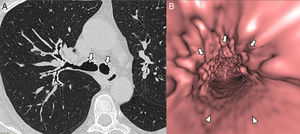
A 60-year-old woman came to the emergency room with symptoms of a respiratory tract infection. The anamnesis included a 50-year history of asthma in treatment with beclomethasone and salbutamol. Obstructive pattern was present in spirometry while Antitrypsin alpha and Prick test were negative. Chest computed tomography (CT) revealed bronchiectasis and multiple calcified nodules on the trachea and main bronchi (Fig. 1A, arrows) which appeared in the virtual bronchoscopy as multiple polypoid images (Fig. 1B, arrows), with sparing of the posterior wall (Fig. 1B, arrowheads), suggestive of tracheobronchopathia osteochondroplastica (TO).
Multidetector computed tomography (MDCT) of the thorax. (A) Axial high resolution MDCT image demonstrates multiple nodular calcifications (white arrows) at the anterior wall of the main bronchi. (B) Virtual bronchoscopy shows nodules (white arrows) involving the anterior and lateral portions of the trachea, with sparing of the posterior wall (arrowheads).
TO is an uncommon idiopathic benign condition affecting the tracheobronchial tree with abnormal chondrification and ossification of cartilages.1 Multiple sessile sub-mucosal nodules, with or without calcifications, with sparing membranous posterior wall and deformed tracheal cartilage rings, without external compressions, are highly suggestive CT findings.1
Most patients are asymptomatic, but the common presenting symptoms are chronic cough, dyspnea, wheezing, and recurrent respiratory tract infections, which often lead to the misdiagnosis of asthma.2 There's no specific treatment for TO, however non steroidal anti-inflammatory drugs and dapsone have been reported to be successful in medical treatment, while invasive procedures such as surgical resection or laser ablation may be used in severe cases.2