Since there are active drugs against tuberculosis (TB), the most effective control measures are to assure treatment adherence and to perform contact tracing. Given the long treatment duration and characteristics of some TB patients, threats that put at risk treatment adherence may appear. Identify and address them is essential to achieve the objectives of disease control.
ObjectivesTo identify the epidemiological characteristics of TB patients and the incidents and threats occurring during treatment, to describe the interventions performed to enhance treatment adherence and to determine if there are differences among native and foreign-born patients in the TB clinical unit of a referral hospital in the inner city of Barcelona.
MethodsA descriptive, observational, cross-sectional study was performed. We recorded information on sociodemographic and clinical characteristics, incidents and interventions during treatment in all patients with TB diagnosed between September 2013 and August 2016.
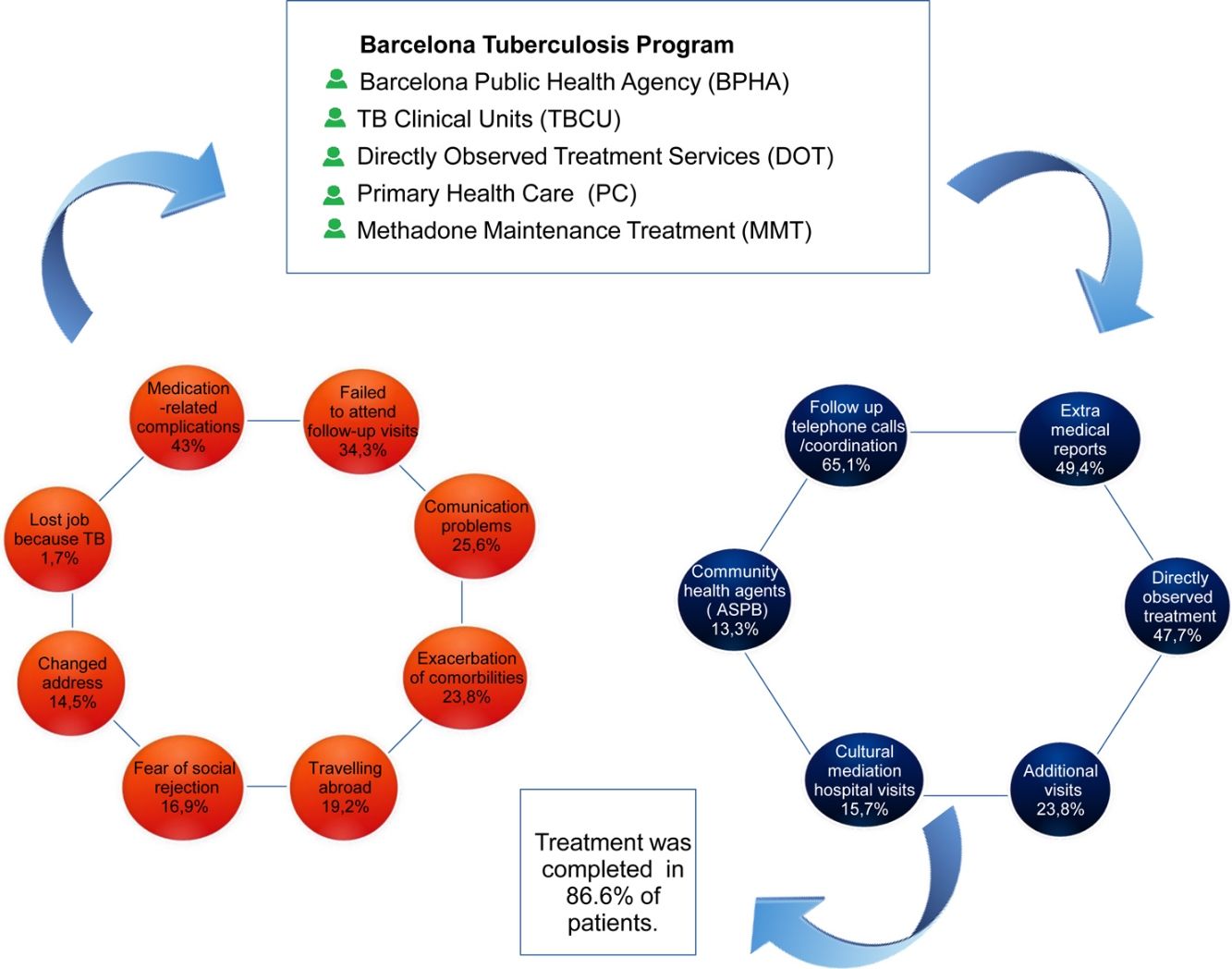
Results172 patients were included, 62.2% were foreign-born. The most common incidents and threats were medication-related complications (43.0%), missed follow-up visits (34.3%), communication problems (25.6%), comorbidities complications (23.8%), trips (19.2%), fear of social rejection (16.9%) and change of address (14.5%). The adherence-promoting interventions were: follow-up calls, directly observed treatment, medical and humanitarian reports, extra visits and cultural mediation. Incidents and interventions were more frequent in foreign-born patients, however there were no differences in treatment success among Spanish and foreign-born.
ConclusionIn this inner city several incidents occurred during TB treatment that can threaten adherence and are more common among foreign-born patients. Coordination among professionals from different healthcare settings was able to overcome obstacles in most cases and achieve TB treatment completion.
Dado que existen medicamentos activos contra la tuberculosis (TB), las medidas de control más efectivas son asegurar la adherencia al tratamiento y realizar un seguimiento cercano. Debido a la larga duración del tratamiento y las características de algunos pacientes con TB, pueden entrar en juego ciertos factores que hacen peligrar la adherencia al tratamiento. Identificar estos factores y abordarlos es esencial para lograr los objetivos de control de la enfermedad.
ObjetivosIdentificar las características epidemiológicas de los pacientes con TB y los incidentes y factores que tienen lugar durante el tratamiento, describir las intervenciones realizadas para mejorar la adherencia al tratamiento y determinar si existen diferencias entre los pacientes nativos y extranjeros en la Unidad Clínica de TB de un hospital de referencia en el centro de la ciudad de Barcelona.
MétodosSe realizó un estudio descriptivo, observacional y transversal. Registramos las características sociodemográficas y clínicas de todos los pacientes con TB diagnosticados entre septiembre de 2013 y agosto de 2016, así como los incidentes y las intervenciones realizadas durante el tratamiento.
ResultadosSe incluyeron 172 pacientes, el 62,2% eran nacidos en el extranjero. Los incidentes y los factores de riesgo más comunes fueron: complicaciones relacionadas con la medicación (43,0%), visitas de seguimiento perdidas (34,3%), problemas de comunicación (25,6%), complicaciones de las comorbilidades (23,8%), viajes (19,2%), miedo al rechazo social (16,9%) y cambio de domicilio (14,5%). Las intervenciones para el fomento de la adherencia fueron: llamadas de seguimiento, tratamiento directamente observado, informes médicos y humanitarios, visitas adicionales y mediación cultural. Los incidentes e intervenciones fueron más frecuentes en pacientes nacidos en el extranjero; sin embargo, no hubo diferencias en el éxito del tratamiento entre españoles y nacidos en el extranjero.
ConclusiónEn este barrio marginal ocurrieron varios incidentes durante el tratamiento de TB que pueden poner en peligro la adherencia y que son más frecuentes entre los pacientes nacidos en el extranjero. La coordinación entre profesionales de los diferentes entornos de atención médica fue capaz de superar los obstáculos en la mayoría de los casos y lograr la finalización del tratamiento de la TB.
Tuberculosis (TB) continues to be a global public health problem worldwide. According to the World Health Organization (WHO) report of 2017, 10.4 million cases were diagnosed worldwide in 2016. A total of 65% of cases occurred in men, 10% in persons living with HIV (PLHIV), and 56% were concentrated in 5 countries: India, Indonesia, China, the Philippines and Pakistan. In all, 3% of cases (290,000 cases) occurred in Europe, with an incidence of 32 cases/100,000 inhabitants.1 In the same period, the incidence of notified cases was 10.7 and 13.3 cases/100,000 inhabitants in Spain as a whole and in Catalonia, respectively and was 16.6 cases/100,000 inhabitants in the city of Barcelona.2,3
Since active drugs against Mycobacterium tuberculosis became available, the most effective measures for TB control and treatment success are early diagnoses and adherence to anti-TB therapy. Given that treatments are long, even those shortened to 6 months, treatment adherence is essential to achieve TB control targets. Indeed, as observed with other chronic transmissible infections such as PLHIV, non-adherence to treatment has a human, economic and very important social cost. Treatment discontinuation reduces its effectiveness, increases transmission, and causes drug resistance, thus increasing morbidity, mortality and more widespread infection. These diseases mainly affect economically and socially disadvantaged groups and may require complex treatment regimens. They are thus a public health priority.4
According to the WHO report on long-term treatment adherence, adherence can be defined as the extent to which a person's behavior corresponds to the recommendations agreed with the health provider. The patient's context is determined by factors related to his or her socioeconomic status, the healthcare team or health system, the disease, treatment, and individual characteristics. Consequently, these factors need to be targeted in interventions to prevent treatment discontinuation.5
The Barcelona TB prevention and control program (TBPCP) was created in 1987, and public health nurses (PHN) played an essential role in following-up TB cases and conducting contact tracing. In its early beginnings, the program encouraged directly observed treatment (DOT) for homeless persons with TB in the inner city (Ciutat Vella) and progressively guaranteed community- or hospital-based DOT for patients showing poor adherence.6 Community health workers (CHW) were incorporated in 2003 because of the increase in immigration from countries with a high TB burden, and their role was to support public health nurses and act as cultural mediators and translators.7 Later, five TB clinical units (TBCU) were created, located at the four large hospitals in Barcelona and in a specialist TB outpatient unit. A key figure in these units is the nurse case manager, who follows up TB patients, performs contact tracing, and supervises treatments always in coordination with public health nurses from TBPCP as well as with other professionals.8 Therefore, this has made it possible to increase TB treatment adherence until 88.5%.3
The aim of this study was to identify the sociodemographic and epidemiological characteristics of TB cases, the incidents occurring during treatment that could influence treatment adherence and contact tracing, the interventions performed to promote adherence comparing foreign-born and Spanish-born patients in a hospital from the inner city of Barcelona with a TBCU, the Mar Hospital, with a population reference of 336,900 inhabitants living in the districts of Sant Martí and Ciutat Vella in Barcelona.
Materials and methodsDesignA population based observational descriptive cross-sectional study in a multidisciplinary specialist TBCU in Mar Hospital in Barcelona from September 1, 2013 to August 31, 2016 was performed. Follow-up of cases was closed in April 2018.
SettingThe TBCU has three medical specialties (pneumology, infectious diseases and pediatrics), a nurse case manager and an administrative assistant. The unit is part of a university referral hospital for the districts of Ciutat Vella and Sant Martí where there is very important immigration from countries with a high TB burden (the percentage of the foreign-born population registered in the districts being 45% and 16.5%, respectively, during the study period). The day to day work is coordinated by the TBPCP of Barcelona. These programs are composed of PHN, CHW, DOT teams and a specialized center for long-term inpatient care of TB patients.
Study participantsThis study included all patients with TB diagnosed and under follow-up by the TBCU of the hospital and notified to the Epidemiology Service of the Barcelona Public Health Agency (ASPB) through the circuits established for reporting notifiable diseases. TB cases were defined as patients with a clinical and/or microbiological diagnosis of TB starting treatment within the study period.9
Data collectionA data collection form was designed for the registration of the various threats that could jeopardize treatment adherence and patient and contact follow-up, as well as the strategies applied to maintain adherence. This form was complemented by an epidemiological survey of the Barcelona TBPCP, collected by PHN from the Epidemiology Service of ASPB for each TB patient, obtaining sociodemographic, clinical–epidemiological, microbiological treatment variables and data on contact tracing. To complete all the information, the patients’ clinical records, the follow-up forms of the public health nurses and those of the CHW were also consulted.
DefinitionsHomeless: persons living on the street or in municipal facilities, centers or shelters (with no fixed abode) and who could be at risk of rooflessness at any moment.
Disposable household income (DHI) index: variable constructed by the Statistics Department of the Barcelona City Council to determine the socioeconomic position of TB patients based on the postal address gathered in the survey, bearing in mind various indicators.10
TB risk factors: the following risk factors were collected in the epidemiological survey of the Barcelona TB program: diabetes, silicosis, renal insufficiency, pregnancy, immunosuppressive therapy, gastrectomy, injecting drug use, HIV/AIDS infection, alcohol abuse, tobacco use, homelessness, and problems with the law or prison.
Threat: event occurring during the treatment of TB that could jeopardize their treatment adherence, follow-up or contact tracing.
Perception and fear of social rejection: includes the perception reported by patients themselves and the variables “does not want to tell co-habitants of his/her diagnosis”, “does not want people at work to know of his/her diagnosis” and “refuses DOT”.
Extra visit: a nurse or physician visit scheduled before the routine follow-up visit (30 days in our TBCU).
Extra report: a medical and/or social report containing an up-to-date summary of the patient's clinical and/or social situation and which is not a discharge report. These reports include humanitarian reports, which are medical reports specifying the patient's disease and stating that treatment cannot be ensured in his or her country of origin.
Successful treatment: according to WHO definition, a cured patient was a patient whose sputum smear or culture was positive at the beginning of the treatment but who was smear- or culture-negative in the last month of treatment and on at least one previous occasion. Patients who completed treatment but who did not have a negative sputum smear or culture result in the last month of treatment and on at least one previous occasion were classified as having “completed treatment”. These two categories were considered as treatment success in this study.11 Therefore successful treatment are cured TB patients plus patients that completed TB treatment.
Ethical considerationsIn agreement with the ethical principles of the Declaration of Helsinki12 on the autonomy and voluntary participation of human research subjects, an informed consent form was signed by all patients and the anonymity and confidentiality of the data were maintained, in accordance with the Spanish Data Protection Law 3/201813 and the General Data Protection Regulation (EU) 2016/679.14 The project was approved by the Clinical Research Ethics Committee of Parc de Salut Mar (number 2014/5840/I).
Data analysisA descriptive analysis of the data was performed. The median and interquartile range (IQR) were calculated for quantitative variables, as they did not follow a normal distribution, while proportions were calculated for categorical variables. To compare foreign with native-born patients, in the bivariate analysis, categorical variables were compared with the chi-square test or the corresponding non-parametric tests. We calculated 95% confidence intervals (CI) and statistical significance was set at 5% (p-value<0.05).
The percentage of patients attended in Mar Hospital from the catchment areas of Ciutat Vella and Sant Martí was calculated and the number of cases treated in the hospital was compared with the total number of cases in the two districts and the number of new TB cases in the city of Barcelona during the study period. The statistical analysis was conducted using the SPSS 20.0 statistical package.
Validity and reliabilityBased on the patients’ clinical records, a data collection form was designed specifically for the study, which helped to ensure the rigor of the registry and coherence of the information. In addition, the information from the TB program was also used as a data source. This program has more than 30 years of experience in TB control and surveillance. From the initiation of the program, information reaching it is validated and contrasted throughout treatment by experienced epidemiologists.
ResultsDuring the study period, 172 TB cases were treated in the TBCU of Mar Hospital. A total of 40% and 55% occurred among residents of Ciutat Vella and Sant Martí districts, respectively. The distribution of cases and incidence of TB according to district are presented in Table 1. The table shows a higher incidence of tuberculosis in Ciutat Vella in relation to Sant Marti and Barcelona.
Distribution of cases and incidence of tuberculosis per 100,000 inhabitants in the districts of Ciutat Vella, Sant Martí and Barcelona per year. Mar Hospital, Barcelona, 2013–2016.
| Year | Ciutat Vella | Sant Martí | Barcelona | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Cases Mar Hospital | Total cases | Incidence† | Cases Mar Hospital | Total cases | Incidence† | Cases Mar Hospital | Total cases | Incidence† | |
| 2013 | 8‡ | 78 | 67.0 | 8‡ | 48 | 21.6 | 17‡ | 329 | 20.4 |
| 2014 | 33 | 62 | 60.5 | 20 | 43 | 17.2 | 59 | 300 | 18.6 |
| 2015 | 27 | 58 | 58.7 | 18 | 44 | 19.6 | 54 | 280 | 17.4 |
| 2016 | 20‡ | 42 | 43.8 | 8‡ | 25 | 10.5 | 30‡ | 260 | 16.2 |
Ref: Programa de Prevenció i Control de la Tuberculosi de Barcelona. La Tuberculosi a Barcelona. Informe. Barcelona: Agència de Salut Pública de Barcelona (2013–2016).
Of the 172 patients included, 106 (61.6%) were men. The median age was 43 years (IQR: 32.2–56). A total of 107 (62.2%) were foreign-born, of which 54 (31.3%) were born in the Indian subcontinent, 12 (6.9%) in Latin America, and 12 (6.9%) in Eastern Europe, while 9 patients were born in Morocco and 9 in the Philippines. Table 2 compares socio-demographic characteristics and clinical variables among Spanish and foreign-born patients.
Comparison of socio demographic and clinical variables between Spanish-born and foreign-born patients with tuberculosis. Mar Hospital, Barcelona, 2013–2016.
| Variables | Categories | Spanish-born (N=65)N (%) | Foreign-born (N=107)N (%) | Total(N=172)N (%) | p-Value |
|---|---|---|---|---|---|
| Sex | Male | 38 (58.5) | 68 (63.6) | 106 (61.6) | |
| Female | 27 (41.5) | 39 (36.4) | 66 (38.4) | 0.506 | |
| Age | Median (IQR) | 54 (42.5–72.5) | 38 (29–49) | 43 (32.25–56) | <0.001† |
| Age groups** | 0–14 | 5 (7.7) | 2 (1.9) | 7 (4.1) | 0.106* |
| 15–24 | 1 (1.5) | 12 (11.2) | 13 (7.6) | 0.019* | |
| 25–39 | 5 (7.7) | 45 (42.1) | 50 (29.1) | <0.001 | |
| 40–64 | 33 (50.8) | 44 (41.1) | 77 (44.8) | 0.217 | |
| >64 | 21 (32.3) | 4 (3.7) | 25 (14.5) | <0.001* | |
| Income according to DHI** | Low | 26 (43.3) | 68 (70.8) | 94 (54.7) | 0.003 |
| Low-medium | 21 (35.0) | 19 (19.8) | 40 (23.3) | 0.029 | |
| Medium-high | 10 (16.7) | 7 (7.3) | 17 (9.9) | 0.060 | |
| High-very high | 3 (5.0) | 2 (2.1) | 5 (2.9) | 0.367 | |
| Employment groups** | Unemployed | 10 (16.7) | 42 (39.6) | 52 (30.2) | 0.001 |
| Student | 2 (3.3) | 7 (6.6) | 9 (5.2) | 0.486 | |
| Retired | 16 (26.7) | 2 (1.9) | 18 (10.5) | <0.001 | |
| Employed | 29 (48.3) | 52 (49.1) | 81 (47.1) | 0.612 | |
| Not known | 3 (5.0) | 3 (2.8) | 6 (3.5) | 0.674 | |
| Tobacco use | Yes | 30 (46.2) | 36 (33.6) | 66 (38.4) | |
| No | 35 (53.8) | 71 (66.4) | 106 (61.6) | 0.102 | |
| Alcohol abuse | Yes | 8 (12.3) | 10 (9.3) | 18 (10.5) | |
| No | 57 (87.7) | 97 (90.7) | 154 (89.5) | 0.538 | |
| IDU | Yes | 2 (3.1) | 5 (4.7) | 7 (4.1) | |
| No | 63 (96.9) | 102 (95.3) | 165 (95.9) | 0.711* | |
| Homelessness | Yes | 4 (6.2) | 14 (13.1) | 18 (10.5) | |
| No | 61 (93.8) | 93 (86.9) | 154 (89.5) | 0.15 | |
| HIV | Yes | 5 (7.7) | 6 (5.6) | 11 (6.4) | |
| No | 60 (92.3) | 101 (94.4) | 161 (93.6) | 0.749* | |
| Immunosuppressive therapy | Yes | 8 (12.3) | 5 (4.7) | 13 (7.6) | |
| No | 57 (87.7) | 102 (95.3) | 159 (92.4) | 0.079* | |
| Diabetes | Yes | 9 (13.8) | 10 (9.3) | 19 (11.0) | |
| No | 56 (86.2) | 97 (90.7) | 153 (89.0) | 0.361 | |
| TB localization | Pulmonary | 46 (70.8) | 54 (50.5) | 100 (58.1) | |
| Extra pulmonary | 19 (29.2) | 53 (49.5) | 72 (41.9) | 0.009 | |
| 1st line drug resistance$ | Yes | 5 (7.7) | 7 (6.5) | 12 (7.0) | |
| No | 40 (61.5) | 61 (57.0) | 101 (58.7) | ||
| Unknown | 20 (30.8) | 39 (36.4) | 59 (34.3) | 0.741* | |
| Prison or problems with the law | Yes | 1 (1.5) | 4 (3.7) | 5 (2.9) | |
| No | 64 (98.5) | 103 (96.3) | 167 (97.1) | 0.651* | |
| Treatment outcome** | Treatment success | 56 (86.2) | 93 (86.9) | 149 (86.6) | 0.887 |
| TB death | 2 (3.1) | 0 (0.0) | 2 (1.2) | 0.141 | |
| Other causes death | 7 (10.8) | 4 (3.7) | 11 (6.4) | 0.105 | |
| Prolonged treatment | 0 (0.0) | 1 (0.9) | 1 (0.6) | 1.000 | |
| Transfer | 0 (0.0) | 5 (4.7) | 5 (2.9) | 0.158 | |
| Lost to follow-up | 0 (0.0) | 4 (3.7) | 4 (2.3) | 0.299 | |
| Risk factors‡ | Yes | 44 (67.7) | 59 (55.1) | 103 (59.9) | |
| No | 21 (32.3) | 48 (44.9) | 69 (40.1) | 0.103 | |
IQR: interquartile range; DHI: disposable household income index; IDU: intravenous drug use; HIV: human immunodeficiency virus; TB: tuberculosis.
In all, 134 patients (78.0%) lived in low- or low-medium income neighborhoods and 81 (47.1%) were employed. At least one risk factor for TB was present in 103 patients (59.9%). Disease localization was pulmonary or mixed in 100 patients (58.1%) and resistance to anti-TB drugs was detected in 12 patients (7%), one of whom showed multiresistance. Treatment success was achieved in 150 patients (86.6%), 5 (2.9%) moved to other autonomous communities of Spain or abroad, 4 (2.3%) were lost to follow-up, and 13 (7.5%) died (2 due to TB) (see Table 2).
Comparison of data from foreign and native-born patients revealed statistically significant differences: foreign-born patients contracted TB at younger ages, lived in neighborhoods with lower incomes, and a higher percentage were unemployed. A larger proportion of native-born patients were pensioners. Pulmonary localization was more common among native-born patients. There were no differences in treatment conclusion between the two groups. A comparison of sociodemographic, clinical and epidemiological factors between foreign and native-born patients is shown in Table 2.
Incidents occurred during follow-up in 151 patients (87.8%) with a median of 2 incidents per patient (IQR: 0–7). Medication-related complications occurred in 74 patients (43%), and exacerbation of comorbidities in 41 (23.8%).59 patients (34.3%) failed to attend follow-up visits in at least one occasion, and 33 patients (19.2%) reported traveling abroad during treatment (see Table 3).
Comparison of threats-related variables between Spanish and foreign-born patients with tuberculosis. Mar Hospital, Barcelona, 2013–2016.
| Variables | Categories | Spanish-born(N=65)N (%) | Foreign-born(N=107)N (%) | Total(N=172)N (%) | p-Value |
|---|---|---|---|---|---|
| Number of threats | Median (IQR) | 1 (0–2) | 3 (2–4) | 2 (1–4) | <0.001† |
| Threats | None | 19 (29.2) | 2 (1.9) | 21 (12.2) | |
| One or more | 46 (70.8) | 105 (98.1) | 151 (87.8) | <0.001 | |
| Medication-related complications | Yes | 30 (46.2) | 44 (41.1) | 74 (43.0) | |
| No | 35 (53.8) | 63 (58.9) | 98 (57.0) | 0.518 | |
| Type of medication-related complications (N=74) | Side effects or intolerance | 16 (53.3) | 23 (52.3) | 39 (52.7) | |
| Treatment prolongation | 14 (46.7) | 21 (47.7) | 35 (47.3) | 0.929 | |
| Complication of comorbidities | Yes | 20 (30.8) | 21 (19.6) | 41 (23.8) | |
| No | 45 (69.2) | 86 (80.4) | 131 (76.2) | 0.096 | |
| Missing in some follow-up visit | Yes | 11 (16.9) | 48 (44.9) | 59 (34.3) | |
| No | 54 (83.1) | 59 (55.1) | 113 (65.7) | <0.001 | |
| Travel | Yes | 2 (3.1) | 31 (29.0) | 33 (19.2) | |
| No | 63 (96.9) | 76 (71.0) | 139 (80.8) | <0.001 | |
| Communication problems | Yes | 1 (1.5) | 43 (40.2) | 44 (25.60) | |
| No | 64 (98.5) | 64 (59.8) | 128 (74.4) | <0.001 | |
| Change of address | Yes | 6 (9.2) | 19 (17.8) | 25 (14.5) | |
| No | 59 (90.8) | 88 (82.2) | 147 (85.5) | 0.124 | |
| Job loss | Yes | 1 (1.5) | 2 (1.9) | 3 (1.7) | |
| No | 64 (98.5) | 105 (98.1) | 169 (98.3) | 1* | |
| Perception and fear of social rejection | Yes | 15 (23.1) | 14 (13.1) | 29 (16.9) | |
| No | 50 (76.9) | 93 (86.9) | 143 (83.1) | 0.090 | |
| Problems of unstable housing | Yes | 1 (1.5) | 14 (13.1) | 15 (8.70) | |
| No | 64 (98.5) | 93 (86.9) | 157 (91.3) | 0.009 | |
| Health card | Yes | 65 (100) | 95 (88.8) | 160 (93.00) | |
| No | 0 (0.0) | 12 (11.2) | 12 (7.0) | 0.004* | |
IQR: interquartile range.
Communication problems were detected in 44 patients (25.6%) and 25 patients (14.5%) changed address; of these, 19 (76%) had pulmonary TB. Another effect of TB diagnosis was stigmatization: 3 patients (1.7%) lost their jobs, 29 (16.9%) showed attitudes influenced by fear of social rejection (not mentioning their diagnosis to cohabitants or at work, not accepting DOT due to fear of rejection by neighbors and/or discrimination in their environment). Compared with Spanish-born, foreign-born patients showed a higher number of threats during treatment, traveled more often, missed more follow-up visits, and had more problems of unstable housing (p<0.05). A comparison of incidents during treatment between native and foreign-born patients is shown in Table 3.
Various strategies were used to maintain adherence. DOT was conducted in a specialized intermediate care center in 82 patients (47.7%), either as long term inpatients or community based DOT outpatients. Extra reports were issued for 85 patients (49.4%), and additional visits were scheduled for 41 (23.8%). Cultural mediation during hospital visits was provided for 27 patients (15.7%), while CHW from the ASPB intervened in 40 patients (13.3%). The PHN and the hospital-based nurse case manager made follow-up telephone calls and coordinated with different healthcare levels in 112 patients (65.1%). Contact tracing was conducted in 79 patients with pulmonary TB (79%) and in 36 with non-pulmonary TB (50%). Eight patients lived alone (4.7%) and 13 refused contact tracing (7.6%) (see Table 4).
Comparison of variables related to adherence strategies used for Spanish-born and foreign-born tuberculosis patients. Mar Hospital, Barcelona, 2013–2016.
| Variables | Categories | Spanish-born(N=65)N (%) | Foreign-born(N=107)N (%) | Total(N=172)N (%) | p-Value |
|---|---|---|---|---|---|
| Contact tracing* | Conducted | 40 (61.5) | 75 (70.1) | 115 (66.9) | 0.248 |
| Refused | 2 (3.1) | 11 (10.3) | 13 (7.6) | 0.135 | |
| Live alone | 5 (7.7) | 3 (2.8) | 8 (4.7) | 0.156 | |
| Not come | 18 (27.7) | 18 (16.8) | 36 (20.9) | 0.089 | |
| DOT | Yes | 25 (38.5) | 57 (53.3) | 82 (47.7) | 0.059 |
| No | 40 (61.5) | 50 (46.7) | 90 (52.3) | ||
| Extra visits | Yes | 18 (27.7) | 23 (21.5) | 41 (23.8) | 0.355 |
| No | 47 (72.3) | 84 (78.5) | 131 (76.2) | ||
| Extra reports | Yes | 17 (26.2) | 68 (63.6) | 85 (49.4) | <0.001 |
| No | 48 (73.8) | 39 (36.4) | 87 (50.6) | ||
| Cultural mediation | Yes | 0 (0.0) | 27 (25.2) | 27 (15.7) | <0.001 |
| No | 65 (100.0) | 80 (74.8) | 145 (84.3) | ||
| CHW intervention | Yes | 3 (4.6) | 37 (34.6) | 40 (23.3) | <0.001 |
| No | 62 (95.4) | 70 (65.4) | 132 (76.7) | ||
| Follow-up calls | Yes | 33 (50.8) | 79 (73.8) | 112 (65.1) | 0.002 |
| No | 32 (49.2) | 28 (26.2) | 60 (34.9) | ||
DOT: directly observed treatment; CHW: Community health workers; TB: tuberculosis.
Foreign-born required more reports, additional visits and telephone calls and were also more frequently referred to DOT centers. There was no statistical differences between Spanish-born and foreign-born patients regarding to contact tracing coverage. The strategies used to maintain adherence by country of origin (native or foreign-born) are shown in Table 4.
DiscussionThe profile of persons diagnosed in this study corresponded to young adults (median age, 43 years), from countries with a high TB burden, especially the Indian subcontinent, of working age and living in low-income neighborhoods. As in other countries in the European Union, these patients had other risk factors in addition to being immigrants, such as immunosuppression, alcohol abuse, tobacco use, psychoactive substance use and, sometimes, problems with the law.15 Other risk factors were social vulnerability, low socioeconomic position, precarious employment not covering basic needs, unhealthy lifestyles and low individual perception of risk, with little appreciation of the personal and community effects of the disease.16 This at-risk population is most numerous in Ciutat Vella,17 an inner city district of Barcelona that, as in London18 or Rotterdam,19 is characterized by being situated in the city center, with a large socially deprived population and an incidence of TB three times higher than that of the city as a whole. Moreover, in Ciutat Vella, there is a higher percentage of those foreign-born compared to the city of Barcelona, as well as a higher incidence of TB due to the high burden of disease in the foreign-born population.2,3,7,17
In this study, we found that a lot and different social, economic and treatment-related threats usually happen during the long treatment period required in TB patients. In agreement with the findings of studies conducted in other countries with a high TB burden such as Colombia and Peru, medication-related complications (side effects) and the presence of comorbidities concurrent with TB were highly common incidents that could provoke treatment withdrawal.20,21 Adverse reactions were also associated with having stopped treatment in a low incidence setting.22 Another common threat was missing follow-up visits. Factors related to this finding in other European cities were a lower perception of risk and suboptimal working conditions.15
Communication problems frequently occurred, due both to patients’ language barriers and to the complexity of healthcare-related information, which, as shown by the literature poses a major threat to adherence in different settings.23–25 Therefore, understanding health information is a requisite for correctly following treatment. Effective communication is essential for patients to take informed decisions and participate in health-promoting processes. As was already described among foreign-born TB patients in Barcelona,7 CHW strategy contributed to minimize this problem also for TB patients for this hospital. Another obstacle identified during TB treatment follow-up was traveling. Foreign-born move aboard more often than the Spanish-born population. Patients usually travel to their country of origin, which can lead to losses to follow-up and TB treatment discontinuation.26–28
Nevertheless, the most important data in our study were those related to the social discrimination affecting TB patients. These findings prompt reflection on the fact that, despite all the knowledge accumulated over the years, TB patients continue to experience perception of social rejection.16 Factors detected in this study were patients not mentioning their diagnosis to cohabitants or in the workplace, not accepting supervised treatment for fear of rejection in their environment, losing their Jobs or being at risk of having to change address because of their diagnosis. These factors directly impacted the therapeutic process and contact tracing. A study conducted in India, the country of origin of many of the patients in this study, supports this reflection and stresses that a substantial proportion of opinion leaders and social representatives show discriminatory behavior toward people who have had TB.29 Another study from Colombia revealed that health professionals, despite having sufficient knowledge of the disease, hold mistaken beliefs leading to discrimination against specific social groups.30 Among countries with a low TB burden, studies have been performed in the USA, Canada, the United Kingdom, Europe and Australia that mention the association between TB, stigma and immigrant communities and demonstrate the interaction between social and cultural determinants and stigma.31 Therefore, a negative social response to TB is universal. While global investigation is focused on treatment and diagnostic tools simplification, the available literature shows insufficient data on research, interventions and recommendations on this topic.32,33
Numerous strategies have been reported in the literature to enhance treatment adherence and contact tracing, including reminders and food vouchers, adherence agreements, intensive patient supervision and social support, the use of new technologies such as an ingestible sensor-based system, video-calls, video DOT etc., which seem to have some potential.34,35 However, broad consensus in the literature is reserved for multi-pronged approaches known as “intervention packages”. This approach is based on patients’ needs and is effective in enhancing adherence.5,36–41 The combined use of all the strategies employed in this study—follow-up calls and liaison between healthcare levels, medical and humanitarian reports, DOT, extra visits, cultural mediation and CHW—allowed completion of most anti-TB treatments and contact tracing. The work performed in a network consisting of healthcare and non-healthcare professionals was essential to carry out these activities. Among other elements, key factors configuring the strategy implemented by the Barcelona TB Program are TB units with nurse case managers, public health teams, DOT teams, CHW, primary care and methadone maintenance programs.7,42,43 As in other countries such as the United Kingdom, the cornerstones of this strategy are flexible healthcare, multidisciplinary teams, and the assignment of a health professional as a key worker to each patient with TB.44
This study found that, compared with Spanish-born, foreign-born patients showed a higher number of threats and incidents during treatment. However, foreign-born required more interventions and finally had similar treatment evolution than Spanish-born patients. Therefore, we can assume that the greater number of interventions in the group with more incidents would be the cause of the similar final evolution.
One of the strengths of this study is that it provides an overall view of the context of patients treated in a referral hospital in Barcelona. The Spanish health system provides universal and for-free coverage. Moreover, the Barcelona TB Program has broad experience and there is clear coordination between the various stakeholders involved in the management and control of TB. The study designed a specific data collection form, favoring rigor in registering data and coherence of the information. In addition, various data sources were used, ensuring the veracity of the data. On the other hand, this study has the limitations characteristic of observational designs such us little control of confounding factors. Moreover, under-registering of the activities reported by the professionals involved in patient follow-up was possible. Another limitation was the small number of cases, which did not allow for more complex statistical analyzes.
ConclusionIdentifying the context and incidents occurring during TB treatment allows the implementation of measures to enhance patients’ adherence. Moreover, coordinated interventions between professionals from different health fields allow to complete treatment: interventions aiming to reduce stigma, improve the administrative situation of the patients, and ensure adequate treatment during trips. The most effective strategy is combining a package of multidisciplinary interventions responding to the particular needs of each patient.
Authors’ contributionsAll authors were involved in the conception or design of the work; the acquisition, analysis and interpretation of data; the drafting of the work and revising it critically; the final approval; and agree to be accountable for all aspects of the work.
Competing interestsThe authors declare that they have no competing interests.
FundingNo additional funding was required.
Ethics approval and consent to participateThe project was approved by the Clinical Research Ethics Committee of Parc de Salut Mar (number 2014/5840/I).
The authors would like to thank all the public health nurses, CHW and committed team of the Barcelona Public Health Agency, the TB Clinic (Serveis Clínics) staff, the social workers and the Mar Hospital team for their support and contributions to this study.