Spirometry is the standard method for monitoring lung allograft function in lung transplantation (LT), with progressive declines in FEV11 and FVC used as indicators of allograft dysfunction [1,2]. However, in single-lung transplantation (SLT), the native and transplanted lungs exhibit distinct resistive and elastic properties, which may lead to an inaccurate assessment of transplanted lung (TL) function using conventional spirometry (SpiroC), potentially delaying the diagnosis of allograft dysfunction [3].
Electrical impedance tomography (EIT) has the potential to estimate expiratory flows separately for each lung, enabling the reconstruction of regional spirometry (SpiroEIT) and providing a more precise tool for evaluating allograft function [4].
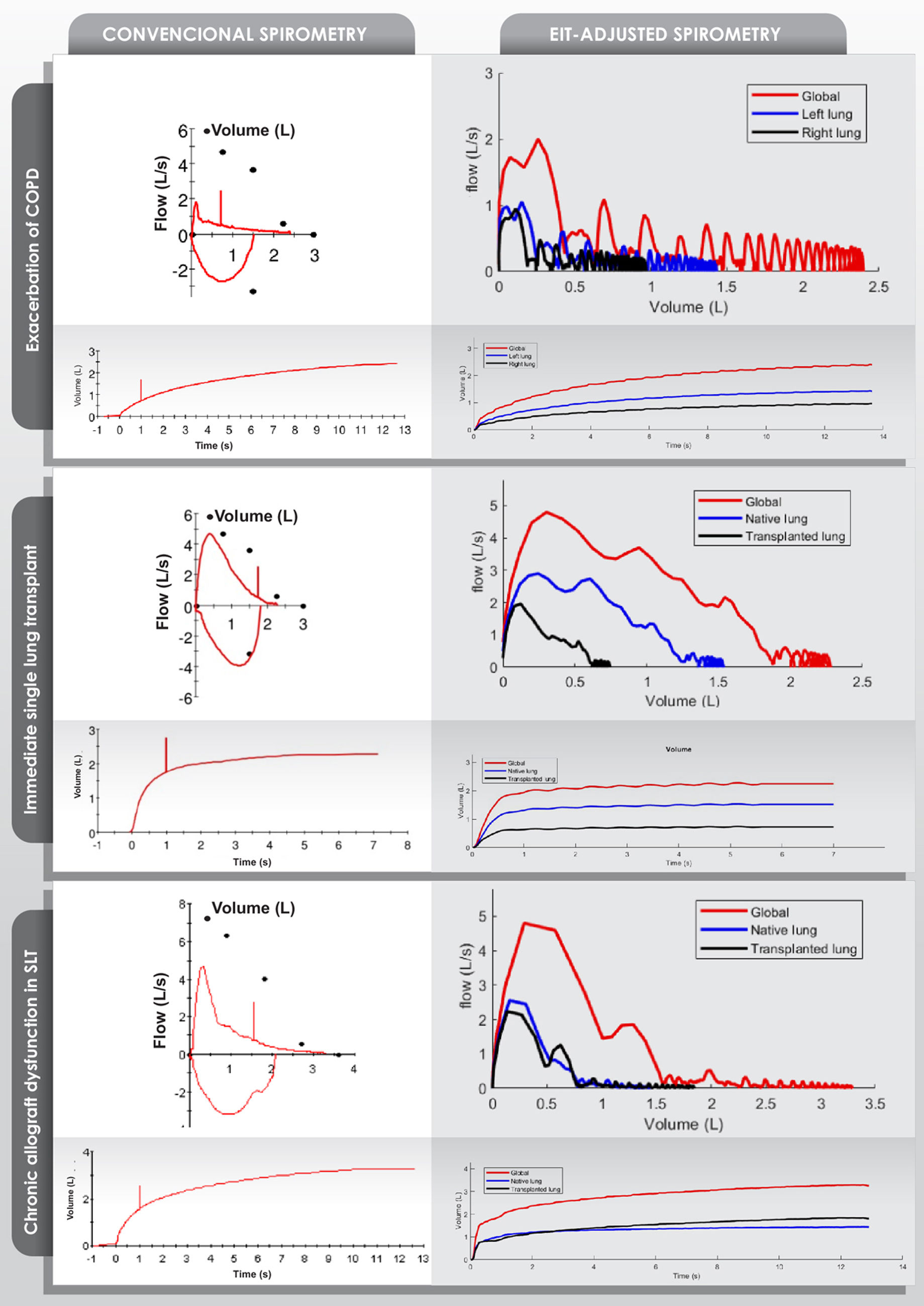
To assess the feasibility of EIT-adjusted spirometry, we applied this technique in three clinical scenarios:
Patient 1: A 58-year-old female with COPD, on the SLT waiting list for two years, hospitalized due to exacerbation. SpiroC showed an obstructive pattern suggestive of elevated airway resistance. SpiroEIT revealed that the left lung exhibited an FEV1 of 0.44L and an FVC of 1.43L, corresponding to 60.3% and 59.6%, respectively, of the values obtained with conventional spirometry (SpiroC), indicating an unequal contribution to total FEV1 and FVC.
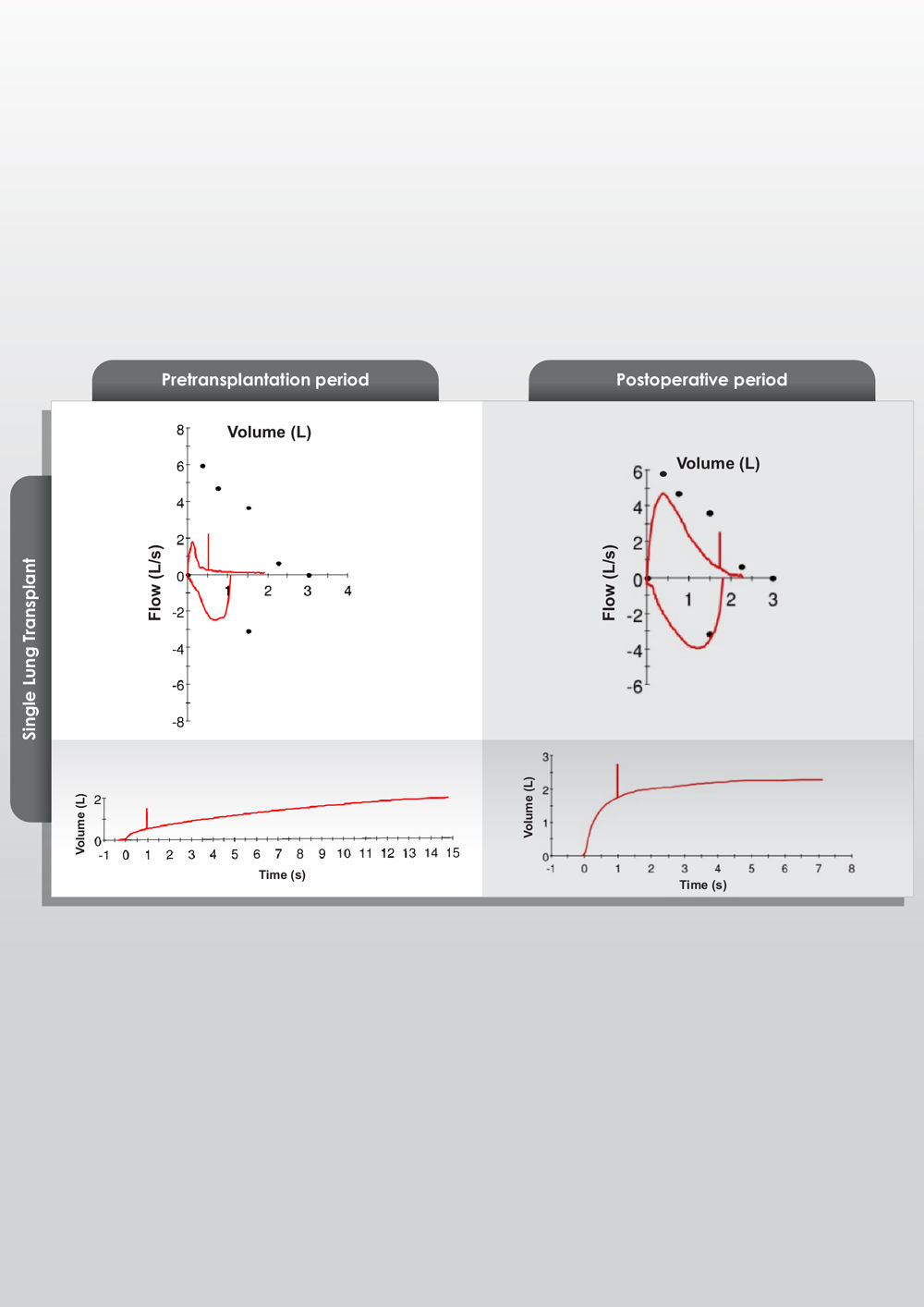
Patient 2: A 53-year-old female in the immediate postoperative period following SLT for COPD. SpiroC demonstrated normalization of global expiratory flow morphology compared to the preoperative period (see supplementary material). However, SpiroEIT revealed that the FEV11 of the transplanted lung (TL) was 0.57L, compared to 1.18L in the native lung (NL). The FVC in the TL was 0.74 vs 1.54 in the NL. This means that the FEV11 and FVC of the TL represented only 32.6% and 32.5% of the SpiroC values, showing an unequal contribution of both lungs in the expiratory flows and volume.
Patient 3: A 68-year-old male, three years post-SLT for COPD, hospitalized due to chronic lung allograft dysfunction (CLAD). SpiroC revealed a severe obstructive pattern, while SpiroEIT showed increased airway resistance in the transplanted lung, consistent with CLAD. The transplanted lung's FEV11/FVC ratio was 0.46, with FEV11 and FVC values of 0.84L and 1.84L, respectively, representing 53.4% and 55.9% of SpiroC values.
SpiroC and SpiroEIT tracings are shown in Fig. 1, and numerical results are available in the supplementary material. These findings show the limitations of SpiroC in SLT and the potential role of SpiroEIT in detecting early allograft dysfunction. Notably, in the postoperative case, a hypothetical 15% decline in transplanted lung FEV11 would translate into only a 5% reduction in global FEV11, potentially delaying the recognition of allograft dysfunction [5].
Illustrations of conventional spirometry and electrical impedance tomography (EIT)-adjusted spirometry in three patients are presented: exacerbation of COPD, immediate post-single lung transplant (SLT), and chronic allograft dysfunction in SLT. The black dots in the conventional spirometry represent normal reference values. EIT-adjusted spirometry revealed that in the patient with exacerbation of COPD, the contribution of FEV11 and FVC from each lung is unequal, with the left lung contributing more to FEV11 and overall FEV1. In the patient during the immediate post-SLT period, FEV11 and FVC of the transplanted lung are lower than those of the native lung. This disparity is attributed to the limitation in the expansion of the transplanted lung caused by hyperinflation of the native lung. In the patient with chronic allograft dysfunction, both lungs exhibit an obstructive pattern. The native lung shows this pattern due to COPD, while the transplanted lung's morphology is consistent with chronic allograft dysfunction.
In addition, SpiroEIT provided new insights into the behavior of the native lung. In the immediate post-transplant period, the FEV11/FVC ratio assessed by SpiroC typically shows improvement, a finding commonly attributed to the implantation of the transplanted lung. However, SpiroEIT revealed an additional relevant observation: an enhancement in the expiratory emptying of the native lung. This was demonstrated by a more physiological morphology of the expiratory flow curve and an increase in the regional FEV11/FVC ratio. Notably, the FEV11/FVC ratio of the native lung approximated that of the transplanted lung and the value measured by conventional spirometry. However, these ratios were derived from significantly different regional FEV1 and FVC values.
This technique offers a novel approach to lung function assessment, providing insights into the complex expiratory flow physiology in SLT. Clinically, SpiroEIT may also assist in preoperative decision-making by guiding the selection of the native lung to retain during SLT, potentially minimizing hyperinflation and optimizing postoperative outcomes.
In conclusion, these findings suggest that EIT-adjusted spirometry could provide a more comprehensive evaluation of allograft function in SLT, enhancing both early detection and clinical decision-making.
CRediT authorship contribution statementIgnacio Fernández Ceballos: Literature search, data collection, study design, manuscript preparation. Joaquin Ems: Study design, data analysis. Miriam Marcos: data collection.
Declaration of generative AI and AI-assisted technologies in the writing processThe authors disclose that part of the material in this manuscript has been produced with the assistance of artificial intelligence software, specifically ChatGPT (version February 2025), to enhance the clarity, readability, and overall quality of the text.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestThe authors declare not to have any conflicts of interest that may be considered to influence directly or indirectly the content of the manuscript.
To Juan Martín Nuñez Silveira, Julieta Gonzalez Anaya and Leyniker Alexander Navarro Rey for their collaboration in carrying out the spirometric measurements. To Indalecio Carboni Bisso and Marcos Las Heras for their help in writing the text.