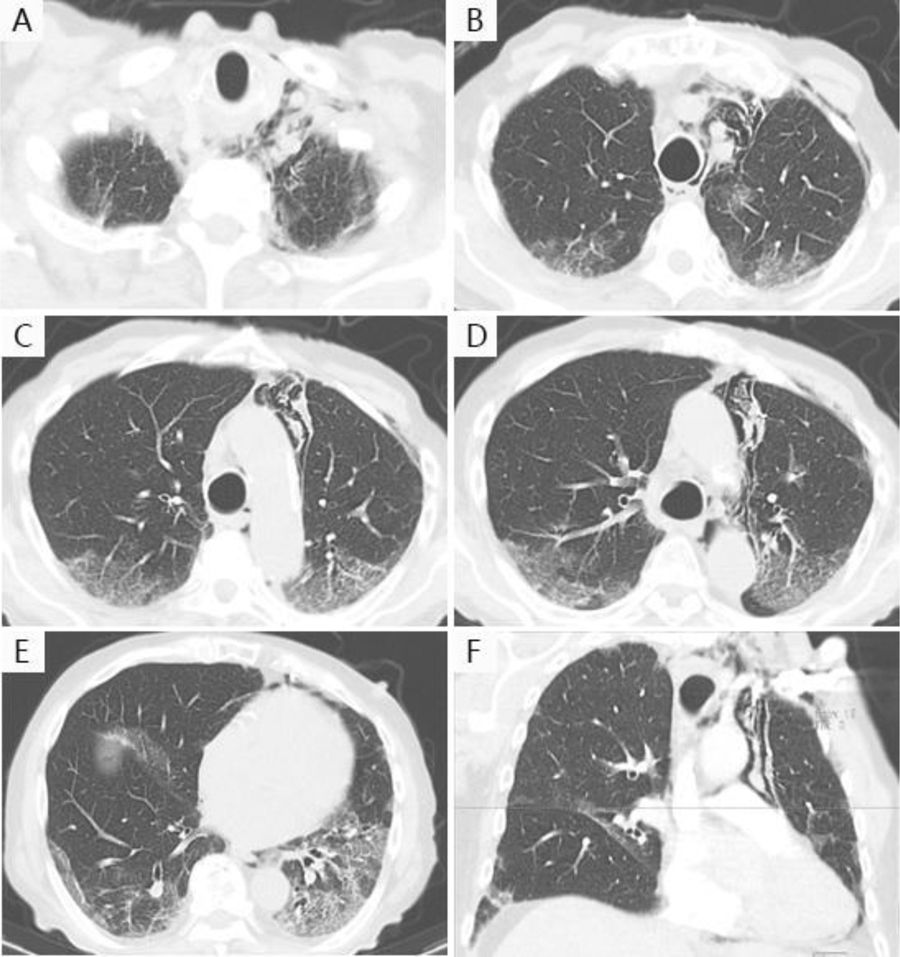
A 88-year-old male, non-smoker, without any underlying lung disease, was hospitalized due to COVID-19 pneumonia, with persistent fever and progressive fatigue. He started treatment with hydroxychloroquine, lopinavir/ritonavir, azithromycin and ceftriaxone, assuming bacterial co-infection. However, there was a radiological and analytical worsening. We switched antibiotherapy to ceftazidime and started corticosteroids, with further analytical and imaging improvement, but maintenance of hypoxemia. A chest CT angiography (Fig. 1) was performed, revealing a pneumomediastinum. After three days of rest and oxygen therapy, patient's hypoxemia improved, with overall good clinical and imaging outcome, showing spontaneous resolution. Because no precipitating factors were identified, as severe cough, signs of respiratory distress, high flow oxygen therapy or ventilatory support, we assumed a pneumomediastinum as a complication of COVID-19 pneumonia. This can be related to an alveolar membrane damage and rupture caused by the disease, followed by air dissection through the bronchovascular sheath into the mediastinum.1,2
Although a pneumomediastinum is a benign disease which only requires conservative treatment,1 it is important to monitor it closely when associated to COVID-19, due to the possibility of disease worsening.1,2
This is an interesting case because it seems to be an uncommon association,1,2 although the overall incidence is yet unknown.