During the last decades the overall and relative number of patients with community-acquired pneumonia (CAP) requiring intensive care management has increased globally, especially among elderly people.1 The percentage of intensive care unit (ICU) admissions attributable to elderly patients ranges between 9 and 19% in European studies2,3 and 20–30% in American studies.4 Severe CAP is the most common cause of acute respiratory distress syndrome (ARDS), which occurs in approximately 7–10% ICU patients with CAP,5 although a recent study found 13% of ARDS among ICU patients with CAP, reaching 29% in those requiring mechanical ventilation.6 Interestingly, the number of quadrants on chest imaging seems to be associated with an increased risk of death in patients with acute hypoxaemic respiratory failure requiring mechanical ventilation.7 However, there is limited information on ARDS in very old patients (VOP ≥80 years old) with CAP. We aimed to assess the prevalence, clinical characteristics, outcomes and risk factors of ARDS in VOP with CAP.
Prospective observational cohort study of consecutive adult patients with CAP admitted to the ICU within 24h from hospital admission, between November 1996 and December 2019. Inclusion criteria were: (1) hospitalized patients ≥80 years old with diagnosis of CAP; (2) severe CAP (according to ATS/IDSA criteria)8; (3) ICU admission; and (4) either invasive (IMV) or non-invasive mechanical ventilation (NIMV) within 24h from admission. Patients were excluded if they had severe immunosuppression or active tuberculosis. ARDS diagnosis was based on Berlin definition.9 Chest-X-ray involvement was analyzed as follows: involvement of one quadrant was considered unilateral, while two quadrants could be unilateral or bilateral; involvement of three or four quadrants was considered bilateral.7
Descriptive statistics were used for basic features of study data and appropriate statistical tests were performed to compare groups. A propensity score for VOP with ARDS was developed by means of a logistic regression model. The score was entered as a continuous variable into four logistic regression analyses to assess association between ARDS and outcomes (i.e., in-hospital, ICU, 30-day, and 1-year mortality). A similar analysis was performed to assess association between lung imaging quadrants and outcomes.
For publication purposes, the study was approved by the Comité Ètic d’Investigació Clínica, register: 2009/5451. The need for written informed consent was waived due to the non-interventional study design.
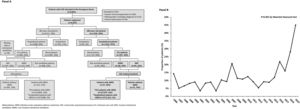
Among 6547 CAP patients admitted during the study period, 4571 patients (69.8%) were<80 years old, 904 (24%) of them were admitted to the ICU; 448 (52%) were not ventilated, 123 (14%) received NIMV, and 297 (34%) received IMV; and 1976 (30%) were VOP, 197 (10%) of them were admitted to the ICU; 95 (48%) were not ventilated, 38 (19%) received NIMV, and 64 (32%) received IMV (Fig. 1, Panel A). Overtime, the proportion of VOP admitted to the ICU changed significantly between 14% and 45% (p<0.001) (Fig. 1, Panel B).
One hundred and fifteen (27%) patients<80 years old met the Berlin ARDS criteria, and 305 (73%) did not. Twenty-seven VOP (26%) met the Berlin ARDS criteria, and 75 cases (74%) did not.
In patients younger than 80 years, those with ARDS presented higher rates of comorbidities (79% vs. 65%, p=0.004) and higher median PSI score (120 vs. 108, p=0.012), than patients without ARDS, while there were not significant differences regarding in-hospital (23% vs.27%, p=0.443), 30-day (21% vs. 21%, p=0.974) and 1-year mortality (29% vs. 30%, p=0.809) between groups. Interestingly, when we compared ARDS patients <80 years old with ARDS VOP, we found that VOP with ARDS had a higher PSI score (108 vs. 140, p<0.001), higher in-hospital (27% vs. 52%, p=0.012), 30 days (21% vs. 56%, p<0.001) and 1-year mortality (30% vs. 68%, p<0.001) than patients<80 years old with ARDS.
Our study population therefore comprised 102 VOP patients (Fig. 1, Panel A). Amongst the 27 VOP with ARDS, 9 (35%), 13 (50%), and 5 (15%) patients had mild, moderate, and severe ARDS, respectively. Seventy-two (84%) non-ARDS VOP presented unilateral infiltrates (1 quadrant 84%; 2 quadrants 12%).
Compared to VOP without ARDS, VOP with ARDS had more frequently received previous antibiotic therapy, and had higher median C-reactive protein values (Table 1). An etiologic diagnosis was obtained in 52 VOP (51%). The most frequent pathogen in both groups was S. pneumoniae (22 out of 40 patients in the non-ARDS VOP group [55%] vs. 8 out 12 VOP in the ARDS group [67%], p=0.473). The most frequent antibiotic regimens were β-lactam plus either a respiratory fluoroquinolone (46%) or a macrolide (25%). There were not differences in the empiric treatment between ARDS and non-ARDS VOP.
Patients characteristic and outcomes according to the presence of ARDS.
| Variable | ARDS | ||
|---|---|---|---|
| No(n=75) | Yes(n=27) | p-Valuea | |
| Age, median (Q1; Q3), years | 83 (81; 85) | 83 (81; 86) | 0.361 |
| Male sex, n (%) | 52 (69) | 15 (56) | 0.196 |
| Previous antibiotic, n (%) | 10 (15) | 9 (38) | 0.022 |
| Previous episode of pneumonia, n (%) | 11 (16) | 1 (4) | 0.130 |
| Comorbidities, n (%)b | 61 (81) | 20 (74) | 0.424 |
| Chronic respiratory disease | 33 (45) | 12 (48) | 0.317 |
| Chronic cardiovascular disease | 14 (19) | 5 (19) | 0.995 |
| Diabetes mellitus | 29 (39) | 8 (30) | 0.402 |
| Neurological disease | 14 (20) | 4 (16) | 0.661 |
| Chronic renal disease | 12 (16) | 4 (15) | 0.864 |
| Chronic liver disease | 2 (3) | 2 (7) | 0.276 |
| Nursing-home, n (%) | 7 (10) | 1 (4) | 0.356 |
| C-reactive protein, median (Q1; Q3), mg/dL | 15.0 (6.3; 22.4) | 25.1 (13.2; 28.9) | 0.015 |
| PSI score, median (Q1; Q3) | 140 (121; 160) | 141 (121; 179) | 0.620 |
| Severe CAP, n (%) | 61 (82) | 23 (88) | 0.552 |
| SOFA score, median (Q1; Q3) | 5.5 (3; 7) | 4.5 (3; 6) | 0.525 |
| CXR quadrants involved, n (%) | <0.001 | ||
| 1 quadrant | 63 (84) | 0 (0) | <0.001 |
| 2 quadrants | 11 (15) | 16 (59) | <0.001 |
| >2 quadrants | 1 (1) | 11 (41) | <0.001 |
| Unilateral/bilateral, n (%) | <0.001 | ||
| Unilateral – 1 quadrant | 63 (84) | 0 (0) | <0.001 |
| Unilateral – 2 quadrants | 9 (12) | 0 (0) | <0.001 |
| Bilateral | 3 (4) | 27 (100) | <0.001 |
| Appropriate empiric treatment, n (%) | 49 (82) | 23 (96) | 0.165 |
| Mechanical ventilation, n (%)c | 0.368 | ||
| Non-invasive | 26 (35) | 12 (44) | |
| Invasive | 49 (65) | 15 (56) | |
| Length of hospital stay, median (Q1; Q3), days | 16 (11; 26) | 17 (9; 23) | 0.663 |
| In-hospital mortality, n (%) | 24 (32) | 14 (52) | 0.067 |
| ICU mortality, n (%) | 12 (16) | 11 (41) | 0.008 |
| 30-day mortality, n (%) | 24 (32) | 15 (56) | 0.031 |
| 1-year mortality, n (%) | 31 (42) | 17 (68) | 0.024 |
Abbreviations: ARDS indicates acute respiratory distress syndrome; CAP, community acquired pneumonia; CXR, chest X-ray; ICU, intensive care unit; PSI, pneumonia severity index; Q1, first quartile; Q3, third quartile; SOFA, sequential organ failure assessment. We excluded patients with severe immunosuppression, active tuberculosis, CAP with sepsis that development septic shock, and unavailable data. Percentages calculated on non-missing data.
ICU, 30-day and 1-year mortality were significantly higher in the ARDS VOP group (p=0.008, 0.031 and p=0.024, respectively). Main causes of death were respiratory failure (non-ARDS VOP: 56% vs. ARDS VOP: 55%) and refractory shock with multi-organ failure (non-ARDS VOP: 39% vs. ARDS VOP 36%). The propensity-adjusted analyses showed that ARDS patients had higher risk of in-hospital, ICU, 30-day and 1-year mortality compared to non-ARDS VOP (odds ratio [OR] 3.13 [95% confidence interval (CI) 1.02–9.61], OR 4.12 [95%CI 1.22–13.91], OR 3.32 [95%CI 1.09–10.13], and OR 4.80 [95%CI 1.40–16.43], respectively), and confirmed by internal validation using bootstrapping with 1000 bootstrap samples and bias-corrected.
VOP with bilateral infiltrates presented significantly higher ICU mortality rates than patients with unilateral/1-quadrant infiltrates (p<0.05). Propensity-adjusted analyses showed that VOP with bilateral infiltrates showed an increased risk of 1-year mortality compared to VOP with unilateral/1-quadrant infiltrates (OR 4.01 [95%CI 1.27–12.62]), confirmed by internal validation using bootstrapping with 1000 bootstrap samples and bias-corrected.
The main findings of our study are as follows. First, 10% of patients with CAP admitted to the ICU were VOP and there was an increase in the proportion of VOP admitted to the ICU overtime, which is in accordance with reports showing a progressive increase of critically ill VOP worldwide.1,2,10,11 Second, 52% of VOP admitted to ICU received MV, which is also consistent with prior studies. For instance, Storms et al.12 found that 42% of patients admitted to the ICU due to CAP received MV, whereas in a study including 930 with CAP admitted to the ICU, we observed that 46.5% received MV.6 Third, ARDS developed in 26% of very old CAP patients treated in ICU with either IMV or NIMV, which is similar to the overall percentage of ARDS found in studies also including non-VOP adults.6,13 Yet, some of these studies showed an age-dependent gradient in the incidence of ARDS in the general population, with a trend towards higher percentages of ARDS amongst older patients.13,14 Fourth, ARDS was associated with significantly higher risk of both short-term and long-term mortality, which provides insight for clinical decision-making, i.e., early implementation of measures to prevent ARDS development. Interestingly, in patients under 80 years old we did not observe differences in outcomes between ARDS and non-ARDS, which is consistent with prior findings of our group.6 Finally, patients with unilateral infiltrates had lower severity than patients with bilateral infiltrates while patients with bilateral infiltrates had higher ICU mortality than patients with unilateral infiltrates. Our results contrast with those of Pham et al.,7 who found that patients with unilateral-infiltrate had mortality rates comparable to that of patients with ARDS of similar severity.
Our study is limited by its small sample size, which precluded further relevant sub-analysis such as the impact of ARDS severity on mortality. However, to our knowledge ours is the first study providing information on ARDS due to CAP in VOP admitted to ICU.
In conclusion, ARDS in VOP with CAP admitted to ICU and ventilated is associated with higher risk of morbidity and mortality. Further research is required in order to enhance clinical decision-making in VOP with severe CAP.
Conflicts of interestThe authors declare that they have no conflicts of interest.