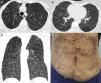
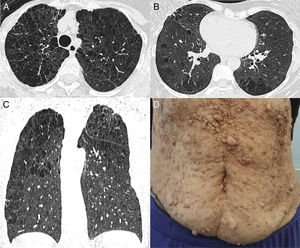
A 69-year-old woman with nonobstructive coronary artery disease and neurofibromatosis type I (NF1) visited a cardiologist, who noted worsening of the patient's functional class. She complained of dyspnea during physical stress, which had started years previously, and mild productive cough. She denied fever, night sweats, chills and any other symptom. She also denied a past history of pulmonary disease. She had a 20-year history of smoking 1 pack of cigarettes per week (3 pack years). A first-degree relative had also been diagnosed with NF1. Physical examination revealed multiple and widespread brownish dermatologic lesions compatible with “café au lait” spots, and multiple skin nodules compatible with neurofibromas (Fig. 1D). Chest CT showed centrilobular emphysema associated with bullae, predominating in the upper lobes of both lungs. Scattered pulmonary cysts of various sizes were also present (Fig. 1A–C). These findings are compatible with pulmonary involvement in NF1.
Axial chest CT images obtained with lung window settings at the levels of the upper lobes (A) and lower pulmonary veins (B), and coronal reconstruction (C) showing emphysema with upper lobe predominance and multiple scattered pulmonary cysts, predominantly in the right lung. Note also in (D) multiple cutaneous neurofibromas in the anterior thoracic wall.
NF1, also known as von Recklinghausen disease, is an autosomal-dominant disorder of neuroectodermal and mesenchymal origin. It can occur as inherited or sporadic disease, the latter corresponding to 30%–50% of cases. A mutation in the NF1 gene on chromosome 17q11.2 has been recognized as a disease prompter, and the spectrum of clinical phenotypes is wide because of the gene's complexity, size and diversity of exons. The disease is characterized by multiple tumors of ectodermal and mesodermal tissues,and its hallmarks are multiple neurofibromas, “café-au-lait” spots and pigmented hamartomas in the iris (Lisch nodules). Neurofibromas are benign nerve-sheath tumors of the peripheral nervous system. Plexiform neurofibromas occur along spinal roots and small branches and large trunks of nerves, and can undergo malignant progression, the major cause of cancer-related death in affected patients.1–3
Some authors have emphasized that interstitial disease associated with NF1 is a definable clinical entity, although the true prevalence and characteristics of this association remain unknown.1 In a literature review, Zamora et al.1 analyzed 61 cases of interstitial lung disease associated with NF1, and the main pulmonary abnormalities on HRCT were bullae (50%), reticular abnormalities (50%), ground-glass opacities (37%), cysts (25%) and emphysema (25%). Other thoracic abnormalities described in patients with NF1 include chest-wall cutaneous and subcutaneous neurofibromas, plexiform neurofibromas, meningoceles, kyphoscoliosis, ribbon deformity of the ribs due to bone dysplasia or erosion from adjacent neurofibromas, other thoracic tumors, posterior vertebral scalloping and enlarged neural foramina.1–5 In conclusion, patients with NF1 may present pulmonary involvement characterized by dyspnea and tomographic evidence of interstitial lung disease, such as emphysema, bullae, cysts and reticular abnormalities.