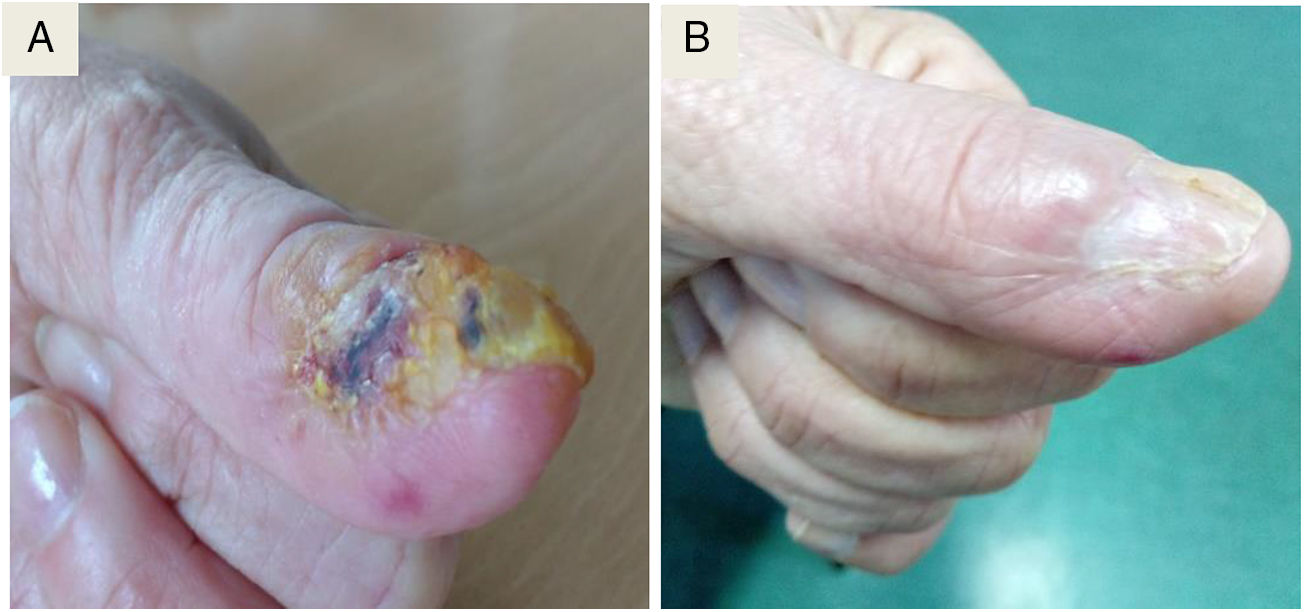
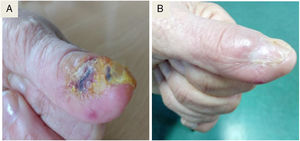
An 80-year-old Caucasian woman presented with a 1-year history of nail dystrophy on the left thumb. She had no history of diabetes, nail trauma, neoplastic disease or other dermatological disorders such as psoriasis. Diagnosis of onychomycosis was initially assumed, so she started topical and oral antifungal agents, but no improvement was noticed. The nail (Fig. 1A) was then biopsied and the histopathological examination revealed epithelioid granulomas with foci of necrosis and lymphocytic infiltrate. Cultural examination of the biopsy was positive for Mycobacterium tuberculosis. Pulmonary involvement was excluded since chest computed tomography was normal and there was no mycobacterial growth on respiratory secretions. Contiguous involvement of the nail by an underlying tuberculous focus in bones was also excluded, since the hand radiograph was normal. Treatment with isoniazid, rifampicin, pyrazinamide, and ethambutol was started. The antibiotic sensitivity test showed sensitivity to all first-line drugs. After 6 months of therapy, the patient presented significant clinical improvement (Fig. 1B).
Nail dystrophy may result of any traumatic or inflammatory process that involves the nail matrix, nail bed or surrounding tissues. Onychomycosis is the most common cause of nail dystrophy in adults, but there are other causes including trauma, congenital abnormalities, psoriasis or cancer. To our knowledge, this is the first case of nail dystrophy due to tuberculosis reported in literature. We excluded tuberculosis of the adjacent osteoarticular structures, as well as other possible causes of nail dystrophy.1,2 This clinical image demonstrates the relevance of a detailed history as well as proper diagnostic tests in determining the etiology of a suspicious and treatment-resistant lesion.1 The importance of systematically sending biopsy samples to mycobacteriological culture should not be overlooked, especially if the histopathological examination shows caseating granulomas.