Both lung growth and aging can be programmed in the early stages of life. The environment during embryonic development and the first years of life are essential for growth and the acquisition of maximum lung function, with a critical window for subsequent lung health.1,2 Accordingly, the debate on the importance of the evolution of pulmonary function at these moments and the impact on adult respiratory health has been ongoing for several decades now.3
Recently, Agusti et al.4 identified a group of individuals in the general population from three different cohorts with low lung function in early adulthood and the risk of early comorbidities and premature death. This work has a considerable value since it highlights the importance of the evolution of pulmonary function and its potential impact on adult life. Interestingly, the authors analyze the long-term impact of a low pulmonary function, defined as two measures of forced expiratory volume in the first second (FEV1) <80%. However, it is important to note that the FEV1/forced vital capacity (FVC) ratio was above 70%. Therefore, the authors are studying the importance of having a restrictive pattern on two occasions in young adulthood, as previously described.5
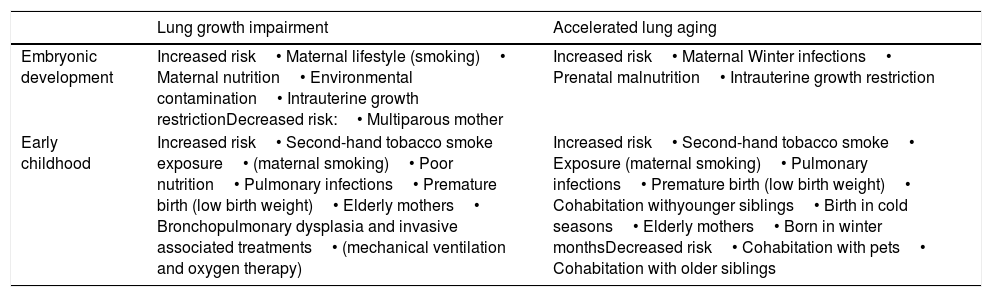
One key aspect of the study is that it does not reveal what happens during childhood or in the neonatal or prenatal period. It is very likely that the situation of decrease of the FVC is related to what happened before its evaluation time. Therefore, we would like to remind researchers two key ideas. First, that lung grow and aging are different but complementary concepts and future research should probably approach them separately. Second, there are a number of different factors that have shown to influence lung growth and aging summarized here in Table 1. From the lung growth perspective, exposures to a range of factors in early life, such as parental lifestyle, nutrition, environmental contamination or viral infections, can restrict growth, modulate lung function and induce changes in gene expression, modulating the pathophysiology of the respiratory tracts.1,6 These factors may interrupt lung development in the saccular phase, resulting in anatomical pulmonary immaturity, altered or delayed synthesis of surfactant, underdeveloped thoracic anatomy and ineffective clearance of respiratory secretions.7 From the lung aging perspective, the decrease in lung function is a normal aging process, but it can be potentiated by multiple risk factors during gestation and childhood including gestational smoking, cohabitation with younger siblings, birth in cold seasons, elderly mothers or premature birth1,2,7,8 (Table 1).
Summary of different early-life factors associated with lung growth and aging.
| Lung growth impairment | Accelerated lung aging | |
|---|---|---|
| Embryonic development | Increased risk• Maternal lifestyle (smoking)• Maternal nutrition• Environmental contamination• Intrauterine growth restrictionDecreased risk:• Multiparous mother | Increased risk• Maternal Winter infections• Prenatal malnutrition• Intrauterine growth restriction |
| Early childhood | Increased risk• Second-hand tobacco smoke exposure• (maternal smoking)• Poor nutrition• Pulmonary infections• Premature birth (low birth weight)• Elderly mothers• Bronchopulmonary dysplasia and invasive associated treatments• (mechanical ventilation and oxygen therapy) | Increased risk• Second-hand tobacco smoke• Exposure (maternal smoking)• Pulmonary infections• Premature birth (low birth weight)• Cohabitation withyounger siblings• Birth in cold seasons• Elderly mothers• Born in winter monthsDecreased risk• Cohabitation with pets• Cohabitation with older siblings |
Additionally, these factors, which act alone or in combination, can also compromise the development of other systems, such as cardiovascular and metabolic.9,10 In Agusti et al. paper, 4–13% of the general population has a low pulmonary function in early adulthood,4 also presenting a higher prevalence of respiratory, cardiovascular and metabolic abnormalities and a greater and earlier incidence of comorbidities. Interestingly, in the light of all potential confounders described early in life, the bivariate analysis presented in that study has a descriptive interest for hypothesis establishment without allowing to draw solid conclusions. Notably, some associations found in Agusti et al. paper may be a consequence of this simple analysis, e.g. associations found in one cohort and not the others, electrocardiogram abnormalities (which does not imply an arrhythmia) or valvular disease and without echocardiographic abnormalities, diabetes or the spurious association with different systemic inflammatory biomarkers. Therefore, it would be necessary to perform an integrated analysis of the variables related to lung growth and aging (Table 1) in order to weigh the relevance of the findings.
Finally, if we accept that airway diseases are influenced by lung development during prenatal and early childhood periods, it follows that this evaluation should be part of our clinical assessment. It is easy to understand that a chronic respiratory condition like chronic obstructive pulmonary disease (COPD) may have a worse lung function and prognosis due to these factors. However, a clinical question is posed as to how should we name a condition in which there is an incomplete lung development or an accelerated aging without previous relevant inhaled exposures.
In conclusion, the evidence of an association of prenatal and early childhood impact on lung growth and aging is increasing. It is therefore important that both pediatricians and pulmonologists collect the personal history of patients with lung diseases, emphasizing prematurity, adequate birth weight, gestational and parenteral smoking, causes of hospitalization at birth, experienced respiratory symptoms, need for mechanical ventilation and oxygen therapy and respiratory infections suffered in childhood. The multidisciplinary approach to these risk factors will improve lung health and reduce the prevalence and severity of a wide range of respiratory diseases.