This clinical case contributes to the limited literature available on plasmacytoma in people living with human immunodeficiency virus (PLHIV). PLHIV have a higher incidence of plasma cell (PC) disorders, which often appear at a younger age and in a more aggressive form compared to the non-HIV population [1]. This report also underscores the importance of lung cancer screening (LCS) with low-dose computed tomography (LDCT) amidst PLHIV, as the implementation of these screening programs has led to the detection of incidental thoracic findings like the one presented here.
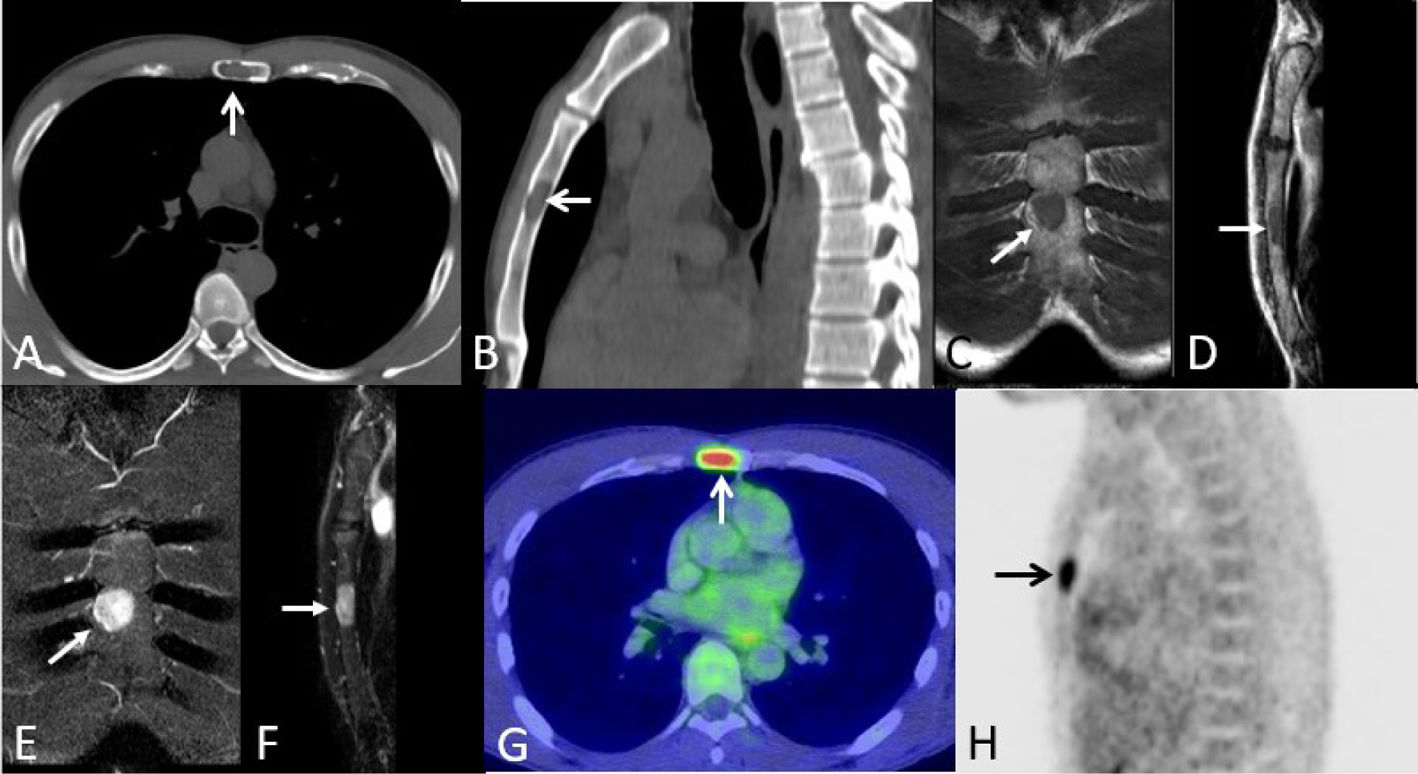
We report the case of an asymptomatic 47-year-old African American male, active smoker (30-pack-years), with a family history of lung cancer (father and paternal grandfather), and diagnosed with HIV infection 15 years earlier. Following our institution clinical guidelines for PLHIV, he underwent LCS with LDCT. The LDCT did not show any suspicious lung nodules but incidentally detected a lytic mid-sternal lesion with a geographic appearance (Fig. 1A and B). Magnetic resonance imaging (MRI) confirmed this finding, an isointense lesion on T1-weighted images and hyperintense on T2-weighted images (Fig. 1C–F), and a whole-body positron emission tomography-CT (PET-CT) demonstrated moderate fluorodeoxyglucose (FDG) uptake by this bone lesion and ruled out any other hypermetabolic lesions (Fig. 1G and H). Furthermore, a percutaneous CT-guided core needle biopsy was performed, followed by a surgical resection. It revealed 6% PCs with kappa light chain restriction among other features that were consistent with bone plasmacytoma. The patient was treated with radiotherapy (40Gy), achieving a successful clinical outcome.
(A and B) Axial (A) and sagittal (B) thoracic low-dose CT images (bone window) show an osteolytic lesion involving the sternal body (arrow). (C and D) Coronal (C) and sagittal (D) T1-weighted MR images show a low-intensity sternal lesion (arrow). (E and F) Coronal (E) and sagittal (F) T2-weighted MR images show a high-intensity sternal lesion (arrow). (G and H) Axial fused PET/CT (G) and sagittal PET-only (H) images demonstrate an increased focal FDG avidity by the sternal lesion (arrow).
Plasmacytoma is an uncommon clonal PC tumor. It should be noted that solitary bone plasmacytoma (SBP), is the most frequent form of plasmacytoma. It is considered an intermediate stage between monoclonal gammopathy of undetermined significance (MGUS) and multiple myeloma (MM), with higher incidence during the fifth and sixth decades of life, in African Americans, and in men (2:1). The etiology remains unclear and clinical manifestations vary, although bone pain (thoracic spine) predominates. Diagnosis requires peripheral blood smear, serum and urine protein electrophoresis and immunofixation, serum free light chain assay, and bone marrow (BM) aspiration/biopsy, together with skeletal survey (showing a “soap bubble” lesion in SBP), whole-body MRI, CT and/or PET-CT [2,3]. Either the evidence of less than 10% clonal PCs in the BM or the absence of BM infiltration, without multiple bone lesions and no end-organ damage constitute the diagnostic criteria for SBP. Differential diagnosis includes MM, MGUS and metastatic carcinoma. Radiotherapy (35–50Gy) is considered the treatment of choice, while the role of surgery and chemotherapy remains controversial. Approximately 50% of SBP cases evolve into MM, requiring lifelong follow-up, with short-interval follow-up examinations initially [2–4].
Recent data supports LCS programs with LDCT in PLHIV over 40 years old, smokers or ex-smokers (who have quit smoking within the previous 3 years) with ≥20 pack-years, and having neither recent pulmonary infections nor contraindications to thoracic surgery [4,5]. To our knowledge, this is the first report of a sternal SBP incidentally detected on LDCT performed for LCS.
CRediT authorship contribution statementAMAR: Data curation, writing – original draft preparation.
MJVG: Supervision, writing – reviewing and editing.
LGS: Supervision, validation, writing – reviewing and editing.
Declaration of generative AI and AI-assisted technologies in the writing processThe authors also declare not to have produced any of the material with the help of any artificial intelligence software or tool.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestThe authors declare not to have any conflicts of interest that may be considered to influence directly or indirectly the content of the manuscript.