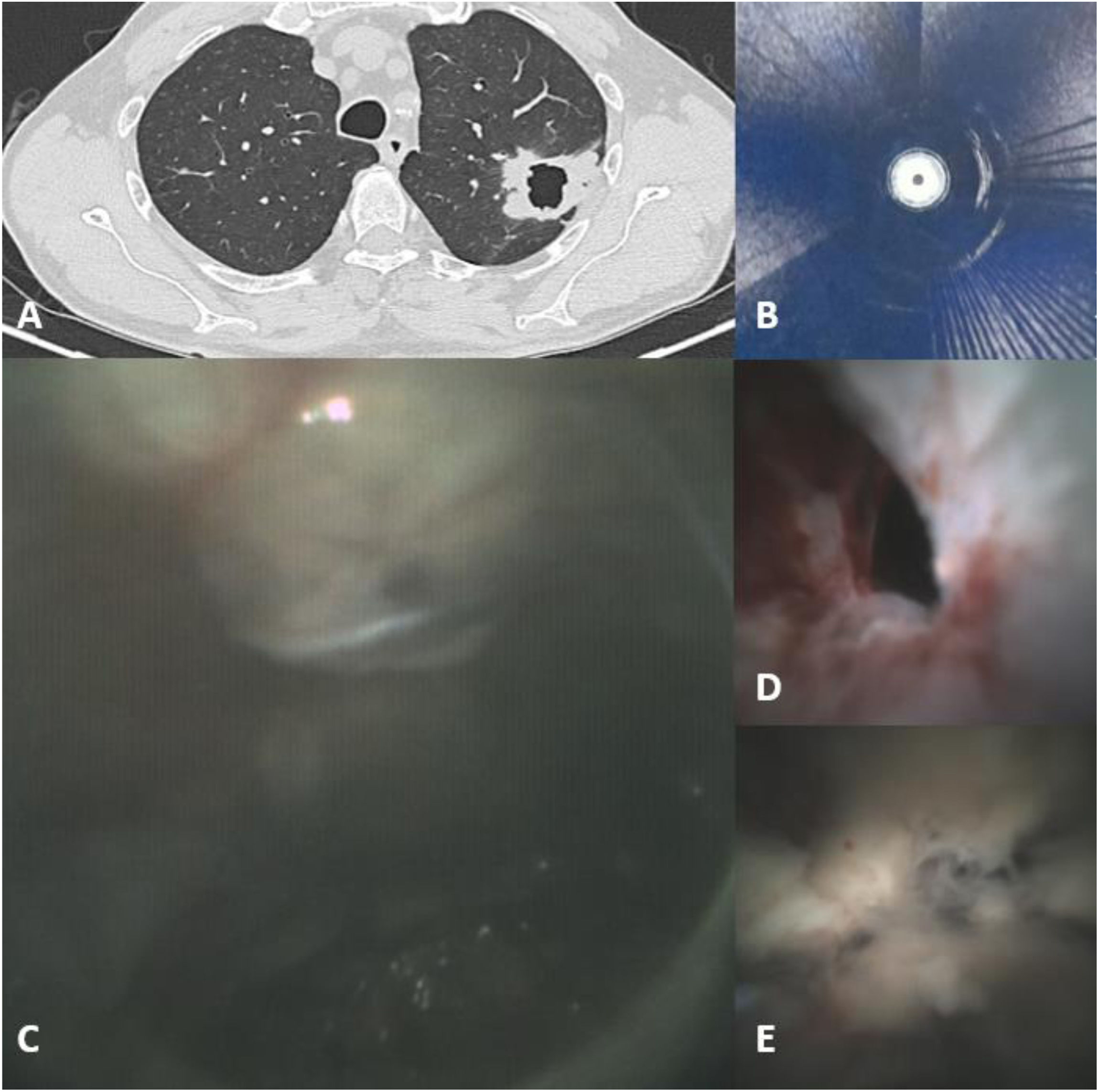
A 68-year-old male, former smoker, was referred to the pulmonology department for a solitary cavitary peripheral pulmonary lesion measuring 30mm in its largest diameter (Fig. 1A). Bronchoscopy (Ambu® aScope 5 Broncho 4.2/2.2mm) was performed under general anesthesia to obtain a histologic diagnosis. Initial lesion localization was attempted using a radial endobronchial ultrasound (R-EBUS) (FUJI PB2020-M2) introduced through a guide sheath (LYS Medical). R-EBUS imaging revealed only air, with no discernible tissue interfaces (Fig. 1B). The R-EBUS probe was subsequently replaced with Iriscope® (LYS Medical), which enabled direct endoscopic visualization within the cavity (Fig. 1C). Slight retraction of the scope allowed clear identification of the cavity entrance (Fig. 1D). This enabled precise positioning within the cavity, allowing targeted cryobiopsies (1.1mm, ERBE elektromedizin) of the most pathological areas (Fig. 1E). Finally, the histopathological analysis reveals a pulmonary squamous cell carcinoma. Catheterization of pulmonary cavities is not uncommon, but is typically performed with ultrathin bronchoscopes in proximal lesions [1,2]. Iriscope® is a novel device that enables direct endoscopic visualization of peripheral pulmonary lesions and is typically used in conjunction with R-EBUS via a guide sheath to optimize lesion localization [3–5]. This case illustrates the utility of Iriscope® for targeted biopsy guidance in cavitary peripheral pulmonary lesions when R-EBUS is insufficient.
MB: draft the article; MB and AK: made bronchoscopy; AK and FB: review the article.
Declaration of generative AI and AI-assisted technologies in the writing processThe authors declare that no artificial intelligence software was used in the preparation of this manuscript.
FundingThe authors declare that no funding was received for the publication of this case.
Conflicts of interestThe authors have no conflicts of interests to declare.