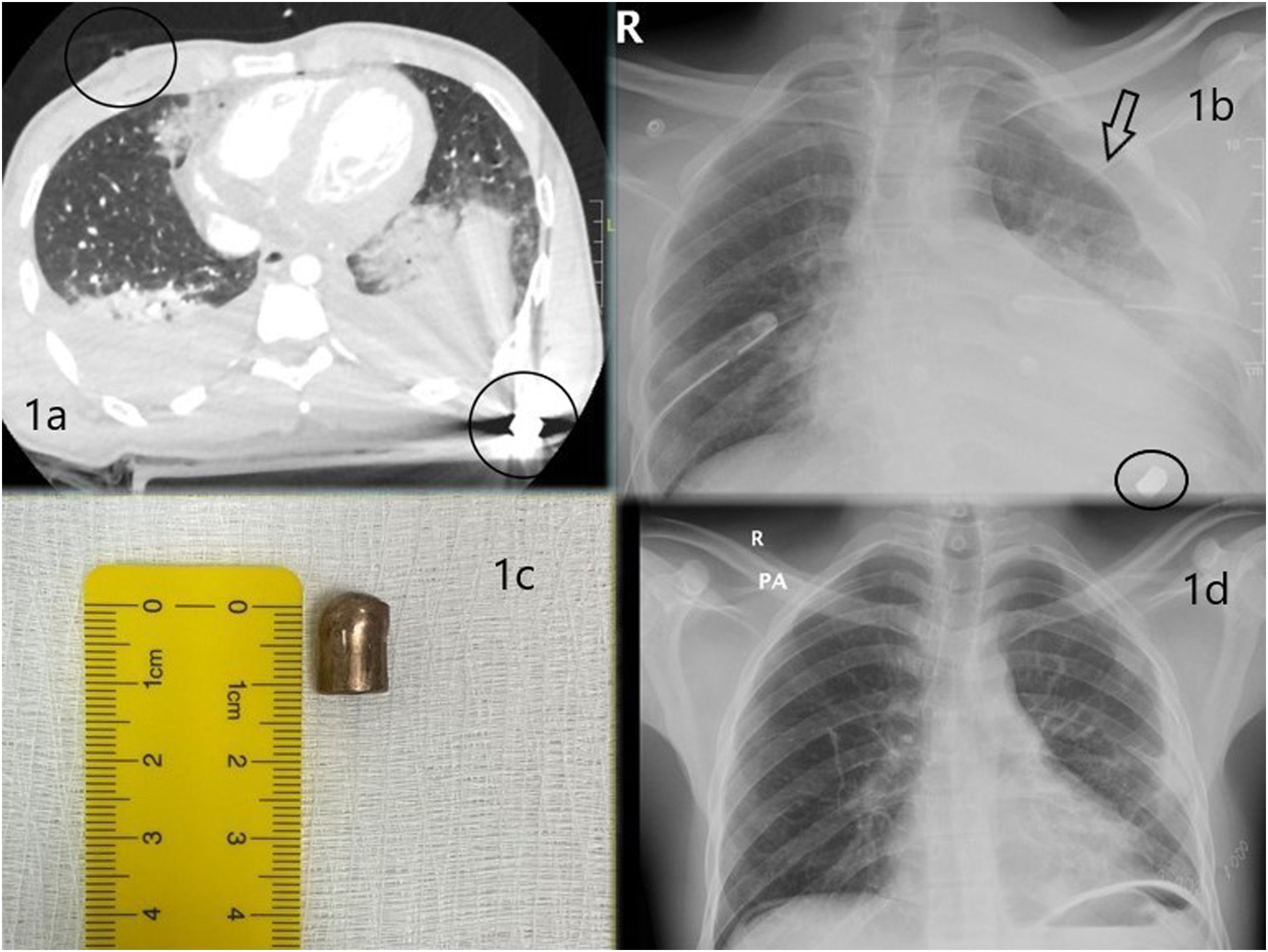
We report the case of a 26-year-old man referred to our emergency department after receiving a firearm injury to the chest. On examination, the patient presented an entry wound in the midclavicular line of the fourth right intercostal space with no exit wound. Breathing and hemodynamics were stable. Emergency chest computed tomography showed bilateral hemothorax and pulmonary contusion (Fig. 1a), a right bullet entry wound (upper circle in Fig. 1a), and the projectile lodged in the dorsal level, below the posterior arch of the seventh left rib (lower circle in Fig. 1a and b). No cardiac, large vessel or tracheobronchial lesions were found. We decided on conservative treatment of the bilateral hemothorax with placement of chest tubes.
On the fourth day of admission, the patient developed fever and leukocytosis, and an image of left pleural occupation was obtained (arrow Fig. 1b). Exploratory left single-port video-assisted thoracic surgery (VATS) was performed, revealing 2 pulmonary tears in the left lower lobe, with no air leak or active bleeding. A retained hemothorax was also located and evacuated, and no intrathoracic bleeding focus was observed. No other relevant endothoracic lesions were found. On completion of the VATS, the bullet (Fig. 1c), which was located in the dorsal subcutaneous plane, causing discomfort to the patient, was extracted independently.
The postoperative period was incident-free and the patient was discharged on the fifth postoperative day after showing good clinical and radiological progress (Fig. 1d). The patient was followed up in the outpatient clinic 1 month after the trauma, confirming an incident-free late postoperative period.
Our case has prompted us to address certain aspects of the management of transmediastinal firearm wounds.
- 1)
Is a systematic invasive tracheobronchial, esophageal or vascular diagnostic examination required in the stable patient? A large number of authors in the literature advocate this approach.1–3 Undiagnosed occult lesions occur only in around 20% of stable patients,3 so we would be systematically subjecting large numbers of patients without injuries to multiple unnecessary invasive treatments. Our recommendation is that if there are clinical, laboratory or radiological issues (after urgent chest CT scan) that suggest tracheobronchial, esophageal and/or cardiovascular lesions, specific diagnostic examinations should be performed in these areas.
- 2)
When should treatment be conservative? We believe that if the patient's respiratory status and hemodynamics are stable, there is no obvious benefit in performing urgent damage-limiting surgery.1–3 Clinical observations derived from the monitoring of vital signs, laboratory parameters (anemia and/or leukocytosis), and the radiological follow-up may indicate the need to stray from the conservative strategy.
In our patient, we had to evacuate a late retained hemothorax by minimally invasive surgery (single-port VATS). This approach is very useful in patients with stable hemodynamics and respiratory status because it offers the possibility of exploring the entire pleural cavity, inspecting and repairing intrathoracic structures if necessary.2,4,5