A 79-year-old man with medical history of hypertension, reported fatigue and weight loss associated to discontinuous fever and night sweats over the past month. Upon admission the patient presented fever and vital signs under normal parameters (blood pressure, heart rate and oxygen saturation). There were no palpable lymph nodes, and chest examination revealed no relevant findings.
Blood test showed elevation of C-reactive protein (145mg/l). However, blood culture and infectious serology tests came back negative. Other blood parameters including complete blood count, coagulation, electrolyte tests, liver and renal function all reported normal values. Chest X-ray revealed cardiomegaly and mediastinal enlargement, with no abnormalities detected in lungs. Additional studies included: normal electrocardiogram, negative tuberculin skin test (TST), and positive interferon gamma release assays (IGRAs). For further assessment, chest and abdomen computed tomography (CT) scans with contrast were done (Fig. 1A), founding a mild free pericardial effusion with circumferential distribution, bilateral paratracheal, bilateral hiliar, and subcarinal lymph node enlargement (maximal 25mm in short axis). Lung parenchyma and bronchovascular structures were normal. Pericardiocentesis was not performed due to its low quantity, checked at transthoracic echocardiography.
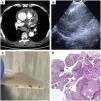
(A) Chest CT-Scan: mild and free pericardial effusion, with circumferential distribution and a large subcarinal lymph node of 48mm. (B) Endobronchial ultrasound view of the opening mini-forceps in the lymph node. (C) Intranodal forceps biopsy samples. (D) Histological intranodal forceps biopsy samples: giant cell granuloma.
The evaluation was completed with a bronchoscopy, with no endoscopic remarkable findings. Bronchoalveolar lavage (BAL) for microbiological and cellular investigations was non-diagnostic. Four samples from subcarinal blinded transbronchial needle aspirations (TBNA) reported negative results in microbiological and cytopathological examinations, including Ziehl–Neelsen staining, mycobacterial cultures and mycobacterium polymerase chain reaction (PCR).
In the absence of a confirmed diagnosis, endobronchial ultrasound (EBUS) at subcarinal lymph node with TBNA and intranodal micro-forceps biopsy (IFB) using CoreDx Pulmonary Mini-Forceps, were performed (Fig. 1B, C). The EBUS-TBNA resulted in non-diagnostic findings. Histological analysis of four EBUS-IFB samples revealed local damage, highly suggestive of giant cell granuloma with necrosis corresponding to tuberculosis (Fig. 1D).
The patient was diagnosed of tuberculous lymphadenitis and probable tuberculous pericarditis. Treatment for extrapulmonary tuberculosis was initiated with the traditional regimen (2 months of HRZE and 4 months of HR).1 The patient completed treatment with a positive clinical, analytical, and radiological response (mediastinal lymphadenitis reduction and pericardiac effusion resolution), without adverse effects.
Tuberculous lymphadenitis is one of the most common presentations of extrapulmonary tuberculosis. Clinical manifestations vary depending on tuberculous lymph node locations. In its assessment, TST and IGRAs are limited since bacterial load is lower, resulting in decreased diagnostic efficacy.2 Tuberculous lymphadenitis is diagnosed by cyto-histopathological examination, PCR testing and lymph node material culture. When mediastinal lymphadenitis is present, EBUS-TBNA is a useful diagnostic tool.1,2
EBUS-TBNA shows a strong overall diagnostic yield (80%) detecting mediastinal tuberculous lymphadenitis.3 It can be used for initial diagnosis of mediastinal tuberculous lymphadenitis, although it only obtains cytologic samples and the yield of microbiological tests are limited for the lower bacterial load in lymph nodes. Detection of granulomas in cell block preparation can be challenging as well. There are emerging EBUS-guided diagnosis techniques such as IFB, which allow to take histological samples.4 It is known that the usefulness of IFB added to EBUS-TBNA improves diagnosis efficiency in mediastinal non-malignant disease (sarcoidosis and lymphoma).5 As shown in this case report, we should consider EBUS-IFB in highly suspected cases of mediastinal tuberculous lymphadenitis when other tests are not diagnostic.
Conflict of interestsThe authors state that they have no conflict of interests.