Mucosa-associated lymphoid tissue refers to lymphoid tissue located under the epithelia of the gastrointestinal, respiratory, and urogenital tracts. Mucosa-associated lymphoid tissue located under respiratory tract epithelia is called bronchus-associated lymphoid tissue (BALT). Marginal-zone B-cell lymphoma of BALT is by far the most common form of pulmonary lymphoma (PL), comprising up to 90% of cases.1–3
The most common computed tomography (CT) findings of BALT lymphoma are lung nodules and air space consolidation, with or without air bronchogram. Other findings are masses, small nodules, and ground-glass opacities. Pleural effusion and mediastinal or hilar lymphadenopathy are rare findings. In most cases, the disease is bilateral.1–5 Although the CT findings of PL have been well described, to our knowledge no study has examined the specificity of dilated air bronchogram inside areas of consolidation (DABIC) for the diagnosis of PL.
To assess the value of DABIC as a sign suggestive of the diagnosis of PL, we retrospectively reviewed the CT scans of 188 adult patients who presented with parenchymal consolidation caused by various diseases (e.g., bacterial pneumonia, tuberculosis, fungal infection, organizing pneumonia, eosinophilic pneumonia, lymphoma, adenocarcinoma, pulmonary hemorrhage, pulmonary edema, lipoid pneumonia). The patients were examined in a tertiary hospital in Brazil between 2010 and 2017. Etiological diagnoses of the consolidations were confirmed by clinical, laboratory, and histopathological criteria.
DABIC was present in three of the six patients with confirmed PL (Fig. 1) and in none of the 182 patients with consolidation caused by other diseases. The patients with PL and DABIC were two men and one woman with a median age at diagnosis of 62 years (range, 56–69 years). The diagnosis of BALT lymphoma was confirmed by video-assisted thoracoscopy in two patients and by open-lung biopsy in one patient. Four patients were asymptomatic on initial diagnosis, and the pulmonary lesions were discovered by routine radiography. Two patients presented with nonspecific pulmonary symptoms, such as cough, dyspnea, thoracic pain, and hemoptysis.
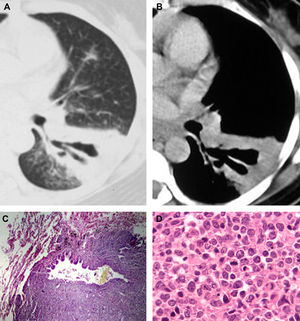
A 45-year-old woman with biopsy-proven BALT lymphoma. Axial computed tomography with the lung (A) and mediastinal (B) window settings showing an area of consolidation in the left lower lobe containing a markedly dilated bronchus. In (C), histopathological section demonstrating a dilated bronchiole with peribronchiolar infiltration of neoplastic cells (hematoxylin and eosin stain, magnification 40×). In (D), histological section showing proliferation of lymphoid cells (hematoxylin and eosin stain, magnification 400×).
Definitive diagnosis of BALT lymphoma requires tissue sampling with immunohistochemical studies to confirm a monoclonal B-cell population.1,2 Wislez et al.3 studied CT findings from 13 patients with BALT lymphoma. They observed consolidations with air bronchograms in six patients. The air bronchograms seemed to be dilated in three cases. CT abnormalities correlated with gross pathological appearance and were related to lymphomatous infiltration with a peribronchovascular distribution. Pathological examination confirmed the presence of airway dilation within lymphomatous lesions. The authors observed no destruction of the bronchial wall or tumor necrosis. They also reported that there are many differences between the bronchial dilation seen in BALT lymphoma and that observed in bronchiectasis. In BALT lymphoma, the bronchial wall is not destroyed, and the dilation is reversible after the lymphoma has been treated. Lymphoma-associated bronchial dilation is always surrounded by a consolidation or mass (generally absent on CT in bronchiectasis) and is not accompanied by sputum. On the other hand, bronchial dilation associated with bronchiectasis is irreversible due to bronchial wall destruction and is frequently associated with productive cough. The authors suggested that bronchial dilation in BALT lymphoma results from the collapse and destruction of the peribronchial parenchyma secondary to lymphomatous proliferation.3 Other authors have also reported air bronchograms with bronchial dilation in patients with BALT lymphoma.4,5 In conclusion, the presence of DABIC appears to be a sufficiently specific CT finding to suggest the diagnosis of PL.