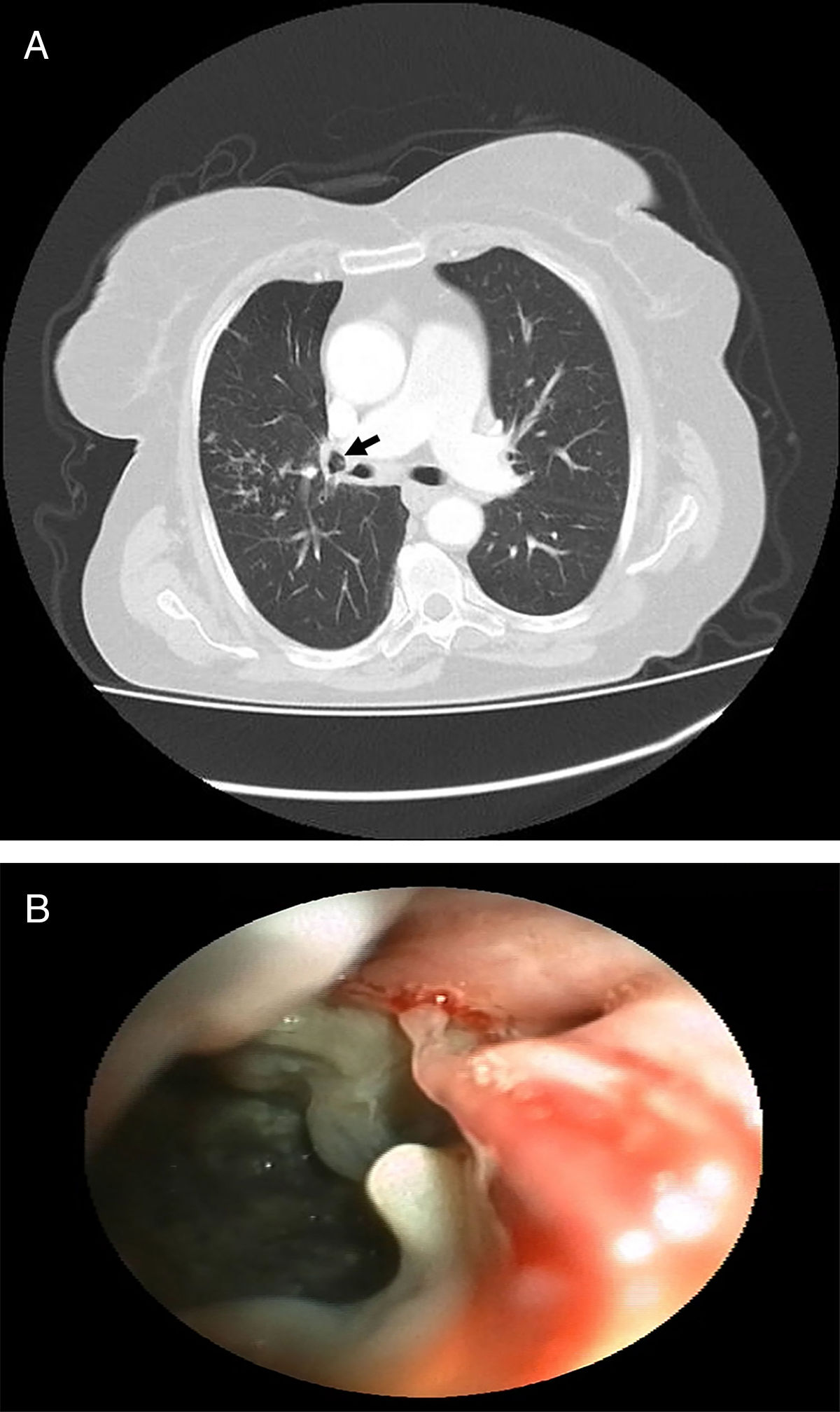
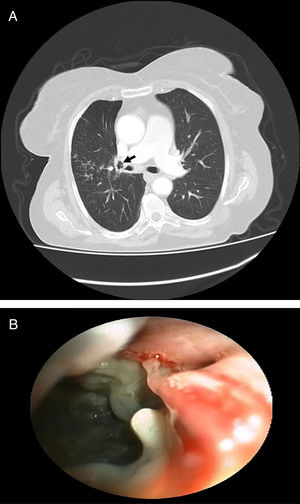
A 83-year-old female patient presented to our clinic with complaints of chronic dry cough, weakness and anorexia. On her physical examination, inspiratory crackles were present on right upper-lung field. Postero-anterior chest X-ray revealed infiltration on right middle zone. Her symptoms were not improved after antibiotic treatment. Acid fast staining (AFS) was negative for three sputum samples. Thorax computed tomography revealed tree-in-bud appearance on anterior segment of the right upper lobe (Fig. 1A). We performed fiberoptic bronchoscopy. On the right secondary carina (RC1), bronchonodal fistula was viewed. Additionally, anterior segment of the right upper lobe was obliterated (Fig. 1B and Video). Bronchial washing from right upper lobe and forceps biopsies from bronchonodal fistula were obtained. Biopsies revealed entirely necrosis. AFS of bronchial washing revealed positive. Patient was negative for human immunodeficiency virus infection and other major immunosuppression state. Patient were underwent anti-tuberculosis treatment for 6 months. At the end of the treatment, her symptoms and radiological findings were improved.
Lymph node in children or immunodeficient patients diagnosed with tuberculosis can erode adjacent bronchial walls which is called “bronchonodal fistula” and other organs including mediastinal vasculature and esophagus via inflammation and necrosis.1,2 Bronchonodal fistula due to tuberculosis in adult immunocompotent patients are extremely rare.1 During fiberoptic bronchoscopy procedure, bronchoscopists should kept tuberculosis related bronchonodal fistula in their mind if they saw erosion on the bronchial wall especially on secondary carina levels on both side.