Cigarette smoking is a major risk factor in the development of chronic obstructive pulmonary disease (COPD). Serotonin levels have been associated with COPD and smoking has been as a significant modulator. Elevated levels of serotonin are responsible for bronchoconstriction and pulmonary vasoconstriction and also nicotine dependence, thus serotonin response could be affected by genetic polymorphisms in transporters and receptors of serotonin.
ObjectivesThe aim of the current study was to analyze the effect of SLC6A4 (5HTT_LPR) (rs25531) and HTR2A-1438G/A (rs6311) genetic polymorphisms on the relation between smoking habits and COPD.
MethodsThe association between SLC6A4 (5HTT_LPR) (rs25531), HTR2A-1438G/A (rs6311), smoking degree and COPD was analyzed in a total of 77 COPD patients (active smokers) and 90 control subjects (active healthy smokers). The DNA was extracted of peripheral leukocytes samples and genotyping was performed using an allele specific polymerase chain reaction.
ResultsThe distribution of SLC6A4 genotypes did not vary between healthy smokers and COPD patients (P=0.758). On the other hand, the A allele of HTR2A (rs6311) was significantly associated with COPD incidence in the trend model (P=0.02; 1.80 [1.04–3.11]). Among all smokers, this allele was also associated with the number of pack years smoked (P=0.02) and also, we observed a marginal association with FEV1/FVC values (P=0.06).
ConclusionOur results point a possible role of the A allele of HTR2A (rs6311) in COPD pathogenesis, suggesting that this effect depends partly on tobacco consumption due to a gene-by-environment interaction.
El consumo de tabaco es el principal riesgo para desarrollar enfermedad pulmonar obstructiva crónica (EPOC). Los niveles de serotonina se han relacionado con el riesgo de desarrollo de EPOC, siendo el consumo de tabaco un modulador significativo.
Los niveles elevados de serotonina producen broncoconstricción y vasoconstricción pulmonar, así como dependencia a la nicotina. Así, la respuesta a serotonina podría verse afectada por los polimorfismos genéticos en los transportadores y receptores de este neurotransmisor.
ObjetivosEl objetivo de este estudio fue analizar el papel de los polimorfismos genéticos SLC6A4 (5HTT_LPR) (rs25531) y HTR2A -1438G/A (rs6311) en la relación entre el consumo de tabaco y la EPOC.
MétodosSe analizó la asociación entre SLC6A4 (5HTT_LPR) (rs25531), HTR2A -1438G/A (rs6311), grado de tabaquismo y EPOC en 77 pacientes con EPOC (fumadores activos) y 90 sujetos control (fumadores activos sanos). El ADN se extrajo a partir de leucocitos de sangre periférica y la genotipificación se realizó utilizando la reacción en cadena de la polimerasa alelo-específica.
ResultadosNo se observaron diferencias en la distribución de genotipos SLC6A4 entre fumadores sanos y fumadores con EPOC (p=0,758). Se encontró una asociación significativa entre el alelo A de HTR2A (rs6311) y la incidencia de EPOC en el modelo predictivo (p=0,02; 1,80 [1,04-3,11]). En los fumadores, este alelo también se asoció al número de paquetes fumados al año (p=0,02) y, además, de forma marginal con los valores de FEV1/FVC (p=0,06).
ConclusiónNuestros resultados apuntan a un posible papel del alelo A de HTR2A (rs6311) en la patogénesis de EPOC, indicando que este efecto dependería en parte del consumo de tabaco a través de una interacción gen-ambiente.
Chronic obstructive pulmonary disease (COPD) is one of the leading causes of mortality and morbidity in the world. Cigarette smoke has several deleterious effects on the airways, leading to and/or influencing chronic respiratory diseases such as COPD. As only between 10 and 20% of heavy smokers develop COPD, risk of COPD depends on environmental and genetic factors.1
The principal component of cigarettes is nicotine that acts at the central nervous system level, causing changes in the brain of the smoker. One of the principal effects of nicotine is the alteration of certain neurotransmitter levels, including dopamine and serotonin (5-hydroxytyptamine, 5-HT). Therefore, the genes encoding the receptors or transporters involved in the dopaminergic and serotonergic pathways are potential candidates in the mechanisms of nicotine addiction.2
In addition, 5-HT is a neurotransmitter that plays an important role in pulmonary function. Elevated levels of 5-HT are responsible for bronchoconstriction and pulmonary vasoconstriction and also increase the risk of risk of pulmonary hypertension (PH).3–6 The development of PH in COPD is mainly attributed to alveolar hypoxia, pulmonary vasoconstriction, vessel remodeling and pulmonary vascular resistence.7
The 5-HT transporter gene, solute carrier family 6, member 4 (SLC6A4) (or 5-HT transporter: 5-HTT), is involved in 5-HT reuptake in the 5-HT pathway, regulating plasma 5-HT levels, and it is thought to be a good candidate for a genetic association with tobacco consumption and COPD. Depression, which is one of the important comorbidities of COPD, is also associated to 5-HT levels and affects the quality of life, exacerbations and mortality in these patients.8,9 More recently, Ishii and colleagues suggest that the quantity of cigarettes smoked may partially mediate the relation between SLC6A4 genotypes and COPD pathogenesis.10 The activation of SLC6A4 on human airway epithelial cells regulates the release of interleukin-6 and interleukin-8 and could play a role in inflammatory responses of airway epithelial cells in COPD subjects by changing the concentration of 5-HT in the peripheral lungs.11
On the other hand, the 5-hydroxytryptamine 2A receptor (HTR2A), encoded by HTR2A gene, is a major post-synaptic target for 5-HT in the human brain and a therapeutic drug target. 5-HT leads to pulmonary vasoconstriction via its 2A and B receptors. Polymorphisms in HTR2A have been related to arterial hypertension or mood disorders.12,13 Very few studies have explored the association of SNPs in HTR2A gene with nicotine addiction and it has been published only one study in COPD.14–16 Functional studies have shown that the activation of 5-HT receptors stimulates different signaling pathways and regulates cytokine release in epithelial cells of the respiratory pathways.11 Therefore, increasing the risk of COPD.
Although the risk of cigarette smoking is well documented, tobacco smoking continues to be the largest preventable cause of disease and premature death. It is estimated that there are currently still over 1.2 billion smokers worldwide, and it is expected to reach about 1.6–1.9 billion by 2025. According to the latest World Health Organization estimates by 2015 about 30% of the smoking related deaths will probably be caused by chronic respiratory diseases.17
In Spain the prevalence of COPD in adult population is about 10.2% and in more than 30 pack years smoked smokers and older than 60 years is more than 40%.18,19 Therefore, it is important to investigate possible predictors in order to prevent the disease at an early stage.
On the basis of these previous findings, the 5-HT system could contribute to the development of cigarette smoke-induced COPD. The present study aimed at investigating the mediation effects of SLC6A4 (5HTT_LPR) (rs25531) and HTR2A-1438G/A (rs6311) genetic polymorphisms on the relation between smoking habits and COPD.
Material and methodsAn analytical, case–control study was conducted. This study followed the STREGA-guidelines (STrengthening the REporting of Genetic Association Studies).20
COPD patients and healthy smokers, reported more than 10 pack years smoked (PY), were randomly recruited in Hospital Gregorio Marañón Neumology Service. All participants were active smokers. The diagnosis of COPD was confirmed using spirometric criteria (a postbronchodilation forced expiratory volume in the first second and forced vital capacity ratio (FEV1/FVC ratio) less than 70%) at least 3 months after admission and with the patient in stable condition.21
All subjects were classified based on their consumption of cigarettes per day (CPD) and PY. PY is a way to measure smoking intensity and is calculated by multiplying the number of packs of cigarettes smoked per day by the number of years the person has smoked. Body mass index (BMI) was taken as anthropometric measurement. Spirometry Testing Airway function was measured at baseline in all study participants using a flow spirometer Spirolab II (Medical International Research, Rome, Italy) according to the guidelines of the European Respiratory Society (ERS). FEV1 and FVC values were expressed as a percentage of the predicted reference value according to the Spanish Society of Pulmonology and Thoracic Surgery.22
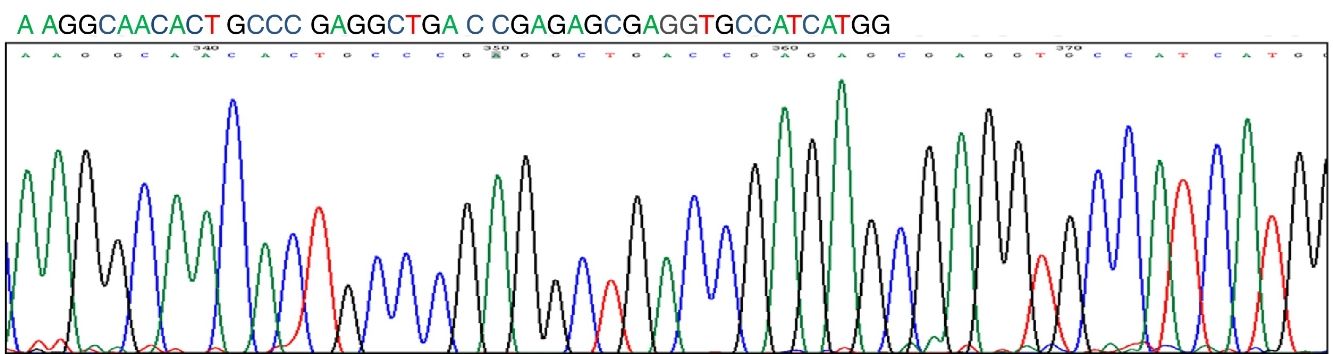
Blood samples were obtained by venipuncture and collected in tubes containing EDTA. The DNA of the peripheral leukocytes was extracted using a standard phenol chloroform protocol. DNA extraction and genotype analyses were carried out in the Biomedicine laboratory at the Universidad Europea, Madrid (Spain). The study followed recommendations for replicating genotype-phenotype association studies, genotyping was performed specifically for research purposes, and researchers in charge of genotyping were totally blinded to the participants’ identities (blood and DNA samples were tracked solely with bar-coding and personal identities were only made available to the main study researcher who was not involved in actual genotyping).23 The DNA samples were stored at −20°C until analysis. Genotyping was performed using an allele specific polymerase chain reaction as detailed elsewhere.15
The study protocol was approved by the institutional ethics committee (Hospital Gregorio Marañón, Madrid). All patients provided written informed consent. The study was in accordance with the Helsinki Declaration.
Statistical analysisAll the values are expressed as mean (SD). We compared smoking phenotypes and clinical characteristics between the different groups with the unpaired Student's t-test. We used the χ2 test to assess deviations of genotype distributions from the Hardy-Weinberg equilibrium (HWE). We also used logistic regression to determine associations between smoking phenotypes and genotypes. We compared genotypes and smoking phenotypes with ANOVA test. All statistical analyses were corrected for multiple comparisons using the Bonferroni method, in which the threshold P-value is obtained by dividing 0.05 by the number of tests. All analyses were performed with the SPSS Statistics 20.0 (SPSS Inc., Chicago, IL, USA) program.
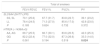
Results167 patients were included in the study (77 COPD patients and 90 healthy smokers). The baseline characteristics of the patients are shown in Table 1. The study participants smoked on average 39.9 PY (SD=22.9), 56.9% of them were female and the overall mean age was 57 years (SD=13).
Patients and healthy controls characteristics.
| All smokers (167) | Healthy smokers (90) | COPD smokers (77) | |
|---|---|---|---|
| Age (years) | 57 (13) | 49 (12) | 62 (10) |
| Females/males (number) | 95/72 | 33/57 | 62/15 |
| BMI | 26.4 (4.6) | 25.3 (4.22) | 27.6 (4.8) |
| PY | 39.9 (22.99) | 31.2 (16.37) | 50.2 (25.4) |
| FEV1/FVC | 72.3 (25.31) | 88.9 (15.48) | 68.1 (25.6) |
| FEV1% | 68.8 (19.27) | 97.3 (19.27) | 61.7 (28.2) |
| FVC% | 84.2 (21.15) | 100.1 (18.79) | 80.3 (19.9) |
Note: The values are given as mean (SD).
Abbreviations: BMI, Body mass index; PY, pack years smoked; FEV1 (%), forced expiratory volume in the first second; FVC (%), forced vital capacity; COPD, chronic obstructive pulmonary disease.
We analyzed the prevalence of the genetic polymorphisms SLC6A4 (5HTT_LPR) (rs25531) and HTR2A (-1438A>G) (rs6311) in COPD patients and healthy smokers. No departure from Hardy-Weinberg equilibrium was detected for the genetic polymorphisms (P=0.697) and (P=0.719), respectively.
The distribution of SLC6A4 genotypes did not vary between healthy smokers and COPD patients (P=0.758). On the other hand, we observed statistically significant differences between HTR2A genotypes and both groups (P=0.037). Analyses focused on associations with genotype categorized using a recessive model (i.e. homozygotes of the most common allele plus heterozygotes were the referent group, compared to homozygotes of the minor allele).
The A allele of the SNP in HTR2A (rs6311) was significantly associated with COPD incidence in the trend model (P=0.02; 1.80 (1.04–3.11)) (Table 2). Among all smokers, this allele was also associated with the number of PY (P=0.02) and we observed a marginal association with FEV1/FVC values (P=0.06) (Table 3). After stratification, we observed the same association in the group of COPD patients but not in the healthy smokers (data not shown). We didn’t find any relationship between genotype and gender or age (P=0.351 and P=0.116, respectively).
Genotypes between smokers groups.
| Smokers | ||||
|---|---|---|---|---|
| Healthy | COPD | P | OR (95%CI) | |
| SLC6A4 (5HTT-LPR) | ||||
| SS, SLa | 73.3 | 75.7 | 0.437 | 1.09 (0.65–1.85) |
| LL | 26.7 | 24.3 | ||
| HTR2A (−1438A>G) | ||||
| AA, AGa | 64.4 | 80.3 | 0.020 | 1.80 (1.04–3.11) |
| GG | 35.6 | 19.7 | ||
Note: The values are given as percentage. Values bold if P value is <0.025.
Abbreviations: SLC6A4, solute carrier family 6, member 4; HTR2A, 5-hydroxytryptamine 2A receptor; COPD, chronic obstructive pulmonary disease; OR, overall risk for non-smokers; CI confidence interval.
Significant P values (<0.025) are in bold.
The association between genotypes, phenotypes and smoking habits.
| Total of smokers | ||||
|---|---|---|---|---|
| FEV1/FEVC | FEV1% | FVC% | PY | |
| SLC6A4 (5HTT-LPR) | ||||
| SS, SL | 70.1 (25.6) | 67.7 (31.7) | 83.8 (22.7) | 39.1 (23.2) |
| LL | 78.4 (24.5) | 71.3 (27.0) | 85.6 (17.0) | 42.8 (23.0) |
| P | 0.185 | 0.624 | 0.732 | 0.372 |
| HTR2A (−1438A>G) | ||||
| AA, AG | 69.7 (25.5) | 66.7 (30.1) | 83.6 (20.5) | 42.3 (25.3) |
| GG | 82.2 (22.4) | 77.0 (32.0) | 87.3 (26.6) | 33.3 (14.0) |
| P | 0.061 | 0.194 | 0.519 | 0.024 |
Note: The values are given as mean (SD). Values bold if P value is <0.025.
Abbreviations: SLC6A4, solute carrier family 6, member 4; HTR2A, 5-hydroxytryptamine 2A receptor; FEV1, forced expiratory volume in the first second; FVC, forced vital capacity; PY, pack years smoked.
Significant P values (<0.025) are in bold.
No statistically relationship was observed between smoking habits or the clinical variables and SLC6A4 (rs25531).
As expected, we observed a correlation between PY as continuous variable and FEV1/FVC, FEV1% and FVC% (P=0.006, P=0.012 and P=0.014, respectively).
DiscussionIn our study we found a statistically significant relationship between the allele A of HTR2A-1438G/A and COPD incidence. Moreover, we observed an association between this allele and PY or FEV1/FVC, however after stratification; we only replicate the results in the COPD group. These results could indicate that HTR2A variant affects COPD pathogenesis and this effect depends partly on tobacco consumption. The acute effects of cigarette smoking produce central nervous system–mediated activation of the sympathetic nervous system. The overactive sympathetic nervous system stimulates the secretion of serotonin (5-HT) and catecholamine into blood at supraphysiological levels.24 Serotonin receptors variants in COPD patients could overactivate a cascade of inflammatory reactions induced by smoking. Although preliminary, the results of our study provide evidence that genetic variations in HTR2A may influence both smoking habits and the development of COPD.
An association between HTR2A (rs6311) and smoking behavior has been reported.14,25 In addition, some authors have indicated an association of HTR2A (rs6311) with PH.3 However, this is the first report on an association between HTR2A (rs6311) variant and COPD.
HTR2A gene is located on chromosome 13q14-q21 and encodes a key membrane receptors of 5-HT. 5-HT, a biogenic amine, is one of the principal neurotransmitters in the central nervous system, interacts with a wide range of psychoactive compounds, including nicotine, and also acts as an important endocrine regulator, playing a key role in the functioning of the cardiovascular and the respiratory system.26
The activation of 5-HT receptors activates intracellular cascades that affect the functioning of other related systems (glutamatergic, dopaminegic, and GABA-ergic).27 Functional studies showed that the activation of 5-HT receptors regulates the release of interleukin-6 and interleukin-8.11 It was also found that 5-HT stimulates different signaling pathways and regulates cytokine release in epithelial cells of the respiratory pathways; thus, it is involved in the pathogenesis of bronchial asthma.11
On the other hand, The HTR2A gene has been regarded as one of the potential candidates for susceptibility to smoking. However, it is not a major contributing factor. The mesolimbic dopaminergic system mediates nicotine reinforcement in the brain, and this system is modulated by the serotonergic system via HTR2A.28 Experimental models have shown that cigarette smoke inhibits monoamine oxidase (MAO) leading to higher levels of 5-HT. Elevated levels of 5-HT are responsible for bronchoconstriction and pulmonary vasoconstriction and also nicotine dependence.5,6
The A allele of rs6311 increases promotor activity, mRNA expression and protein levels and increases receptor binding.29,30 This promoter polymorphism supports an hyperactive serotonergic system.31 In addition, Falkerlber et al. suggested that the promoter polymorphism (rs6311) can affect both transcription factor binding and promoter methylation, and this along with an individual's stress response can impact the rate of HTR2A transcription in a genotype and methylation-dependent manner.32 The rs6311 polymorphism of HTR2A was previously shown to be associated with nicotine dependence and smoking behavior.14,25 However, there is only one published study about rs6311 polymorphism of HTR2A and COPD risk and its results are not conclusive.16
Way et al. demonstrated the association between plasma 5-HT levels, and COPD. Higher plasma 5-HT levels were found in stable COPD patients compared to the control subjects. An up-regulation of serotonergic pathway due to HTR2A genotype and smoking could be related to higher inflammatory response of airway epithelial cells and higher risk of COPD.
On the other hand, there were no differences between SCL4A6 (rs25531) genotype and COPD. There are no previous studies that analyzed SLC4A6 (rs25531) polymorphism and COPD risk. An association between SCL4A6 (rs2020936) variant and smoking behavior or nicotine dependence has been reported.15,33 In addition, Ishii and cols. concluded that SCL4A6 (rs2020936) variant affects COPD pathogenesis and depressive symptoms in Japanese population.10 It should be noted that in this study, controls were a mixture of current and ex-smokers. Other authors have reported that SLC4A6 (rs25531) long allelic variant was associated with PH in COPD.3 Ulrich et al. supported a pathogenic role of the 5-HT system in the development of PH in COPD and the need for further studies in this field.3
The present study has several limitations. First, a limitation of the current study is its relatively small sample size, and as such, the findings require replication. To strengthen confidence in our findings we have selected an ethnically homogenous sample of Caucasians. Second, we have analyzed only two genetic variants of serotonin system genes. Other different variants in the 5-HT signaling pathway, such as described in tryptophan hydroxylase 2 (TPH2) and MAO type A, could be related to the pathogenesis.34
On the other hand, despite of the small simple size of the current study, our population is homogeneous, not stratified and well defined in terms of phenotype assessment and to our knowledge, this is the first study to evaluate the relationship between smoking intensity, COPD and the polymorphism HTR2A (rs6311) in Spanish population. Moreover the study follows the STREGA guidelines, all participants were randomly recruited in Hospital Gregorio Marañón Neumology Service by a pulmonary medicine specialist, genetic polymorphisms were selected attending their prevalence and functional impact in the protein, no departure from Hardy-Weinberg equilibrium was detected for the genetic polymorphisms or multiple testing and reporting of quantitative (continuous) outcomes were used). Better reporting of studies facilitate the synthesis of available research results and the further development of study methods in genetic epidemiology improving the understanding of the role of genetic factors in the cause of diseases.
ConclusionsPrevious studies consider the hypothesis that, in addition to their involvement in nicotine dependence, 5-HT response in COPD patients could activate a cascade of inflammatory reactions induced by tobacco consumption. We speculate that the cigarette smoke-mediated injury in COPD lungs is partially mediated by HTR2A (rs6311). Despite the evidence that confer SCL4A6 gene and 5-HT response we have not found any relationship between SCL4A6 (rs25531) and COPD susceptibility.
In summary, although the effects of HTR2A (rs6311) alone are modest, our results suggest a possible role of the A allele of rs6311 in COPD pathogenesis, providing evidence that genetic variations in HTR2A may influence both, smoking habits and the development of COPD. Further investigation of the functional role and the regulation of 5-HT due to genetic variants in COPD is important for understanding and preventing the progression of this disease.
FundingThis study was supported by a grant of SEPAR (2006).
Conflict of interestThe authors declare no conflict of interest.