Ameloblastomas are rare (1–2 cases per million people1) odontogenic tumours that seat in the jaw. They are usually big and locally aggressive, with a high recurrence rate if not completely resected. However, it is exceptional for them to progress to malignancy or metastasis.
We present the case of a 62-year-old, heavy smoking male, without other comorbidities, who presented in 2014 with swelling of the left part of the maxilla, without any other symptoms. Both vital signs and basic analytical tests were normal.
After performing a cranial/cervical CT scan and a biopsy of the lesion, he was diagnosed of follicular ameloblastoma; being treated with maxillectomy. Three years later he consulted with a local relapse, which was treated with left orbital exenteration. The post-surgical biopsy showed mainly a typical morphology of secondary type ameloblastic carcinoma, intraosseous, over areas of follicular ameloblastoma.
Two months later an MRI of the mandible was requested, with evident growth and extension of the infiltrative area, affecting the nasal septum and the base of the orbit, infiltrating the maxilla. The recurrence was confirmed with a biopsy and was managed with radiotherapy, resection and reconstruction of the affected area.
He then followed biannual controls in Oncology, remaining disease-free for the next years.
In August 2021 he was admitted in Pneumology due to a bacterial pneumonia of the right upper lobe; in the chest radiograph performed 10 weeks later the infiltrate had not completely cleared, so a chest CT was requested, showing a 15mm lesion in the right upper lobe, informed as a secretion-filled bronchocele, making it necessary to do a radiological follow-up.
An abdominal and pelvic CT, dated April 2022, showed a central mass in the right upper lobe, measuring 32mm×19mm, with focal stenosis of the anterior segmental bronchus, solid, with spiculated margins, which made us suspect malignancy.
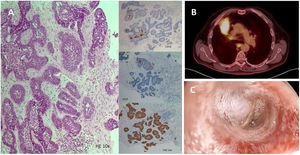
A PET-CT scan and a bronchoscopy were performed to characterize the lesion. The imaging technique showed the known pulmonary mass and hypermetabolic mediastinal lymphadenopaties, suspected to be malignant. Furthermore, the architecture and immunohistochemistry of the bronchial lesion were compatible with an odontogenic lesion (ameloblastoma), thus confirming the metastatic origin of the tumour (Fig. 1).
(A) Lesion composed of cords or sheets of basaloid odontogenic epithelial cells with peripheral palisading and reverse polarity surrounding nests of stellate reticulum-like cells. (H–E 10×, CD56 10×, ck19 10×, P40 10×). (B) PET-CT Showing central mass in the right upper lobe measuring 32mm×19mm with mediastinal spread. (C) Bronchoscopy finding of the image shown in B.
After deliberation at multidisciplinary team, it was decided to treat with chemotherapy and radiotherapy, which the patient is currently receiving.
Ameloblastomas are tumours that generally have an indolent course. Only 2% of the cases metastasize1,3 and, when they do, it is preferably to the lung, lymphatic nodes, bone or brain. Metastases can appear decades after the primary tumour, thus making it mandatory to follow life-long check-ups. The physiopathology why in some cases they are prone to disseminate is not fully understood, but one of the many proposed mechanisms is the extension following inhalation of malignant cells during a surgical procedure,2 which could explain the predilection for metastasizing to the lung.
As of today there is no consensus towards the treatment of metastatic ameloblastomas in the lung; however, it was recently suggested that targeted therapy against V600 BRAF mutation could be used, showing a favourable clinical outcome.4