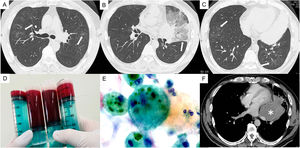
A 56-year-old non-smoker man presented to the outpatient clinic with a chief complaint of dysgraphia. Magnetic resonance imaging of the brain revealed a 62-mm mass in the left occipital lobe, and brain biopsy revealed metastatic lung cancer harboring a rearrangement in the anaplastic lymphoma kinase (ALK) gene. Five days after initiating first-line chemotherapy with alectinib, the patient complained of a dry cough. Chest computed tomography showed bilateral scattered ground-glass opacities with thickening of the interlobular septa (Fig. 1A–C). Bronchoalveolar lavage of the right upper lobe retrieved a bloody fluid with a gradual increase in concentration (Fig. 1D), and cytology revealed hemosiderin-laden macrophages (Fig. 1E). We diagnosed the patient with alectinib-induced diffuse alveolar hemorrhage (DAH).1 The patient's condition rapidly improved after discontinuation of alectinib and initiation of systemic steroid therapy. Lorlatinib was safely administered as the second-line chemotherapy without DAH. ALK-inhibitor induced DAH has not been previously reported. In this case, age was the only risk factor for interstitial lung disease associated with ALK inhibitors.2 In central lung cancer, promptly performing a bronchoscopy aids the treatment strategy because airway obstruction due to bleeding can be critical (Fig. 1F). The patient provided informed consent for the publication this article.
Chest computed tomography shows bilateral scattered ground-glass opacities with thickening of the interlobular septa (A–C, white arrows). Bloody bronchoalveolar lavage fluid (D); cytology shows hemosiderin-laden macrophages (E). Chest computed tomography shows an irregular mass in the left central lung (F, asterisk).
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNone.
We would like to thank Editage (www.editage.jp) for English language editing. In addition, we would like to thank the staff of the department of pathology at Showa University Koto Toyosu Hospital.