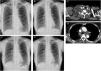
A 78-year-old female non-smoker with a history of hyperlipidemia complained of daytime sleepiness, and her family pointed out her snoring. The patient did not complain of pain in the neck, chest, shoulders, and upper limbs and dysesthesia such as paresthesia, hypoesthesia, or weakness. Her body mass index was 19.2kg/m2. Chest X-ray (CXR) revealed no abnormal findings (Fig. 1A). Polysomnography using Alice 6® (Philips Respironics; Murrysville, Pennsylvania, USA) was performed. Diagnostic polysomnography revealed that the apnea–hypopnea index (AHI) was 83.0events/h, comprising 57.3events/h of obstructive apnea, 1.3events/h of mixed apnea, 0.3events/h of central apnea, and 24.1events/h of hypopnea. Thus, the patient was diagnosed with severe obstructive sleep apnea. Continuous positive airway pressure (CPAP) therapy was introduced using an auto-titrating device (DreamStation®; Philips Respironics), which was set to auto mode (pressure setting: 4–6cmH2O). Polysomnography under CPAP therapy revealed that AHI was 8.3events/h. Diagnostic polysomnography and polysomnography under CPAP therapy showed no evidence of ventricular arrhythmia, such as premature ventricular contraction and non-sustained ventricular tachycardia. The patient's physical condition did not change after one day of the initiation of CPAP therapy. However, two days after the initiation of CPAP therapy, she complained of malaise and right-sided cervical swelling a few hours after switching the CPAP device off. On the other hand, she did not complain of headache. Physical examination revealed swelling in the right supraclavicular fossa. The D-dimer level was 1.4μg/mL. CXR revealed the enlargement of the superior mediastinum and the deviation of the trachea to the left (Fig. 1B). Although contrast-enhanced chest computed tomography revealed no evidence of thrombus and lymph node enlargement, edematous change of the right-sided subcutaneous structure and the mediastinum and right pleural effusion were detected (Fig. 1C and D). Thus, we discontinued CPAP therapy without any treatments. The next day, the follow-up CXR revealed improvement in the enlargement of the superior mediastinum and tracheal deviation; however, this CXR also revealed a slightly increased right pleural effusion (Fig. 1E). Physical examination revealed improvement of swelling in the right supraclavicular fossa. One week later, the follow-up CXR revealed improvement in the patient's right pleural effusion (Fig. 1F).
CXR images (A, B, E, and F), contrast-enhanced chest computed tomography images (C and D). (A) Before the initiation of CPAP therapy. (B–D) Two days after the initiation of CPAP therapy. (E) The day after the discontinuation of CPAP therapy. (F) One week after the discontinuation of CPAP therapy. CPAP=continuous positive airway pressure; CXR=chest X-ray.
Herein, we described a patient who developed edematous change of the right-sided subcutaneous structure and mediastinum and right pleural effusion after the initiation of CPAP therapy. We considered that these complications could be induced by CPAP therapy not but other reasons for the following reasons:
The time course: the edematous changes and pleural effusion emerged after the initiation of CPAP therapy, and they improved without any treatments after its discontinuation.
The absence of evidence of thrombus: A rare cause of unilateral cervical edema is unilateral internal jugular vein thrombosis.1
The laterality of the lesions: The edematous change and pleural effusion occurred on the right side. A rare cause of unilateral cervical edema is spontaneous cervical swelling syndrome, which induces edematous change in the left cervical region.2
The absence of typical features: The patient did not have typical clinical features of thoracic outlet syndrome.3
CPAP increases the intrathoracic pressure, which induces right arterial pressure and decreases venous return, which eventually increases ventricular arrhythmia,4 thereby increasing pressure on the superior vena cava. Additionally, this increase can close the venous valves in the jugular veins, which can cause cough headache syndrome, thereby increasing jugular vein pressure.5 The increase in pressure on the superior vena cava and jugular vein was considered to be correlated with the occurrence of edematous change of the right-sided subcutaneous structure and mediastinum and right pleural effusion after the initiation of CPAP therapy. However, the exact mechanism remains unknown.
This report provides the reconsideration that we need to pay attention to hemodynamic changes in the initiation of CPAP therapy.
Disclosure statementAll authors have seen and approved the manuscript.
Financial conflictsThe Department of Advanced Medicine for Respiratory Failure is a Department of Collaborative Research Laboratory funded by Teijin Pharma.
The Department of Respiratory Care and Sleep Control Medicine is funded by endowments from Philips-Respironics, ResMed, Fukuda Denshi and Fukuda Lifetec Keiji to Kyoto University.
This study was funded in part by the JSPS (Japan Society for the Promotion of Science), Grants-in-Aid for Early-Career Scientists (KAKENHI)22K16169 (SH).
Conflict of interestSatoshi Hamada reports grants from Teijin Pharma, outside the submitted work.
Susumu Sato reports grants from Philips Japan, ResMed, Fukuda Denshi, Fukuda Lifetec Keiji, Fuji Film corporation, and Nippon Boehringer Ingelheim outside the submitted work.
Toyohiro Hirai has nothing to disclose.
We have no acknowledgements.