Recent publication of multi-ethnic spirometry reference equations for subjects aged from 3 to 95 years aim to avoid age-related discontinuities and provide a worldwide standard for interpreting spirometric test results.
ObjectivesTo assess the agreement of the Global Lung Function Initiative (GLI-2012) and All ages (FEV0.5) reference equations with the Spanish preschool lung function data. To verify the appropriateness of these reference values for clinical use in Spanish preschool children.
MethodsSpirometric measurements were obtained from children aged 3–6 years attending 10 randomly selected schools in Barcelona (Spain). Stanojevic's quality control criteria were applied. z-Scores were calculated for the spirometry outcomes based on the GLI equations. If the z-score (mean) of each parameter was close to 0, with a maximum difference of ±0.5 from the mean and a standard deviation of 1, the GLI-2012 equations would be applicable in our population.
ResultsOf 543 children recruited, 405 (74.6%) were ‘healthy’, and of these, 380 were Caucasians. Of these 380, 81.6% (169 females, 141 males) performed technically acceptable and reproducible maneuvers to assess FEVt, and 69.5% achieved a clear end-expiratory plateau. z-Scores for FVC, FEV1, FEV1/FVC, FEV0.75, FEV0.75/FVC, FEV0.5, FEF75 and FEF25–75 all fell within ±0.5, except for FEV1/FVC (0.53 z-scores).
ConclusionsGLI equations are appropriate for Spanish preschool children. These data provide further evidence to support widespread application of the GLI reference equations.
La publicación reciente de ecuaciones de referencia de espirometría multiétnicas para edades de 3 a 95 años tiene como objetivo evitar las discontinuidades relacionadas con la edad y proporcionar un estándar mundial para la interpretación de los resultados de la espirometría.
ObjetivosValidar las ecuaciones de la Global Lung Function Initiative (GLI-2012) y All ages (FEV0,5) en niños preescolares españoles, para verificar la adecuación de estas ecuaciones para su uso clínico.
MétodosSe realizaron espirometrías forzadas en niños de 3 a 6 años de edad de 10 colegios seleccionados aleatoriamente en Barcelona (España). Se aplicaron los criterios de control de calidad de Stanojevic et al. Se calculó el z-score según las ecuaciones GLI-2012. Se consideró que para que las ecuaciones GLI-2012 pudieran ser aplicables en nuestra población, la media expresada en z-score de cada parámetro debía de tener un valor próximo a 0 y una desviación estándar (DS) de 1, aceptando como máximo una diferencia de ± 0,5 z-scores respecto a la media.
ResultadosDe los 543 niños reclutados, 405 (74,6%) eran «sanos», y de ellos 380 caucásicos. De estos, 81,6% (169 mujeres, 141 hombres) realizaron maniobras técnicamente aceptables y reproducibles para evaluar la FEVt, y el 69,5% logró una meseta espiratoria final adecuada. Los z-scores para FVC, FEV1, FEV1/FVC, FEV0,75, FEV0,75/FVC, FEV0,5, FEF75 y FEF25-75 estuvieron incluidos entre ± 0,5 z-scores, salvo el FEV1/FVC (0,53 z-scores).
ConclusionesLas ecuaciones GLI son apropiadas para los niños preescolares españoles. Estos datos proporcionan nuevas evidencias para apoyar su utilización.
Several publications1–4 have shown that preschool children aged 3–6 years are able to perform spirometry, thanks to improved spirometric techniques and a test adapted for this age range using computer-animated systems with visual incentives, prompting the European Respiratory Society (ERS) and the American Thoracic Society (ATS)5 to publish standardized procedures for preschoolers in 2007. Reference equations have also been published for this age group in various populations,3,6–11 including Spain (CANDELA study12). Developing reference equations for preschoolers has been useful for demonstrating the applicability of spirometry in this age group, but one of the problems is the discontinuity of values for children older than 6 years of age.13 This inevitably produces gaps between preschool and school age children which may lead to the misinterpretation of final test results.14 The situation is further complicated by the high number of available reference equations to choose from. Using the wrong equations may lead to both under- and overdiagnosis, so it is essential that data are available to help us assess the adequacy of the equations in our population.
In order to solve these problems, All ages equations for subjects from 3 to 80 years of age were developed,15,16 and in 2010 the Global Lung Function Initiative (GLI) was created to develop the first worldwide continuous reference equations for forced spirometry for all ages (3–95 years) and different ethnic groups.17 Since then, various authors have validated these equations,18–20 and assessed the implications of using them instead of the equations currently in use.21–23
The aim of this study was to validate the GLI-2012 reference equations in a series of healthy Caucasian preschool children aged 3–6 years from the city of Barcelona (Spain), and to assess the validity and reliability of the forced spirometric technique in this age range, by evaluating the different quality criteria of the test.
MethodsThe study was performed with the approval of the Clinical Research Ethics Committee. The City Council of Barcelona and school heads agreed to the conduct of the study. Informed consent for participating in the study was obtained in all cases from the parents or legal guardians of the children.
Population and Calculation of Sample SizeThe study population consisted of randomly selected, healthy preschool children aged 3–6 years, attending various private and public schools in Barcelona (Spain). The sample size was estimated according to the recommendations of Quanjer et al.,24 which require the inclusion of at least 300 local controls (150 boys and 150 girls) to validate the reference equations and avoid differences of 0.5 z-scores occurring by chance.
MethodologyParents were given a health questionnaire to distinguish “healthy” children from “non-healthy” children, in terms of respiratory disease. To avoid creating any sense of discrimination among the children, spirometry was performed in all children whose parents authorized their participation in the study, although those who did not meet the criteria for participation were subsequently excluded from the analysis.
Inclusion criteria were as follows: age between 3 and 6.99 years; born at term (>37 weeks); absence of repeated episodes of bronchitis or other chronic lung disease; no significant heart disease; no neuromuscular or bone disease that might contribute to a restricted lung capacity; and no systemic disease with pulmonary involvement. Children who had had an isolated episode of bronchitis without hospitalization were included.
Spirometries were performed in schools during school hours by the same pediatrician (CMV), who is experienced in the use of forced spirometry techniques adapted for children. Weight was determined using weighing scales, and height using a measuring rod (Seca mod. 173, Seca®, Hamburg); both devices were correctly calibrated. Spirometries were performed with a MasterScreen® spirometer with 5.0 software (VIASYS Healthcare, Höchberg, Germany). The spirometer was calibrated every day with a 3-liter syringe (ViasysHealthcare, Hochberg, Germany). Environmental calibration was performed on a daily basis. Biological control was also performed. Disposable mouthpieces with antibacterial filters (Neumofilt®; Hospital Hispania, Madrid, Spain) were used.
Height was measured without shoes and weight with lightweight clothing. Spirometry was conducted according to ERS/ATS recommendations5 with the subject in an upright seated position. Nasal clips were not used. Computer-animated systems were used to help subjects correctly achieve peak expiratory flow (PEF) (blowing candles) and forced vital capacity (FVC) (knocking down bowling pins). Each child performed up to 8 maneuvers.
Spirometric Variables and Quality CriteriaThe following parameters were collected for each child: flow–volume (F/V) and volume–time (V/T) curves, forced expiratory time, PEF, FVC, forced expiratory volume in the first second (FEV1), 0.75s (FEV0.75), and 0.5s (FEV0.5), forced expiratory flow at 75% of FVC (FEF75%), forced expiratory flow between 25% and 75% of FVC (FEF25%–75%), and back-extrapolated volume (Vbe).
All spirometries were assessed independently for quality by 2 of the investigators (CMV, IMM, SRA, ATV, SG, IIS, AMG). In case of discrepancies, a third investigator performed an assessment and consensus was reached on interpretation. The ATS/ERS5 quality criteria, modified by Stanojevic et al.,16 were used for this analysis, as follows: (1) rapid onset of expiration (Vbe<80ml or Vbe/FVC<12.5%); (2) clearly defined PEF; (3) visually correct expiratory curve, without artifacts, cough, glottic closure or air leaks; (4) good repeatability: difference of <100ml or <10% between the 2 best values of the forced expiratory volume in a given time (FEVt) and FVC, with the requirement of at least 2 correct maneuvers; (5) clearly defined final plateau in the V/T curve. For the analysis of FEV1, FEV0.75, and FEV0.5 to be considered acceptable, criteria 1, 3 and 4 had to be met. For the analysis of FVC, FEVt/FVC ratios and flows (FEF75 and FEF25–75) to be considered acceptable, criterion 5 of a well-defined plateau was required.
Data Analysisz-Scores were calculated from the GLI-2012 reference equations. FEV0.5 reference values are not included in GLI-2012, so All ages equations were used to calculate the FEV0.5z-score16 (see Appendix A). Weight and height z-scores were calculated with the reference equations for the Spanish population.25
For the GLI-2012 equations to be applicable in our population, the z-score (mean) of each parameter must be close to 0, with a standard deviation (SD) of 1 and a maximum difference of ±0.5 z-scores from the mean.20,24
Mean, SD, median and range were used to describe quantitative variables.
The Cochran–Armitage trend test was used to compare the different quality criteria of the spirometric maneuvers according to age. The Student's t-test was used to compare values obtained between girls and boys. A P value <.05 were considered statistically significant. Analyses were performed using the MedCalc Statistical Software package, version 13.0.2 (MedCalc Software bvba, Ostend, Belgium).
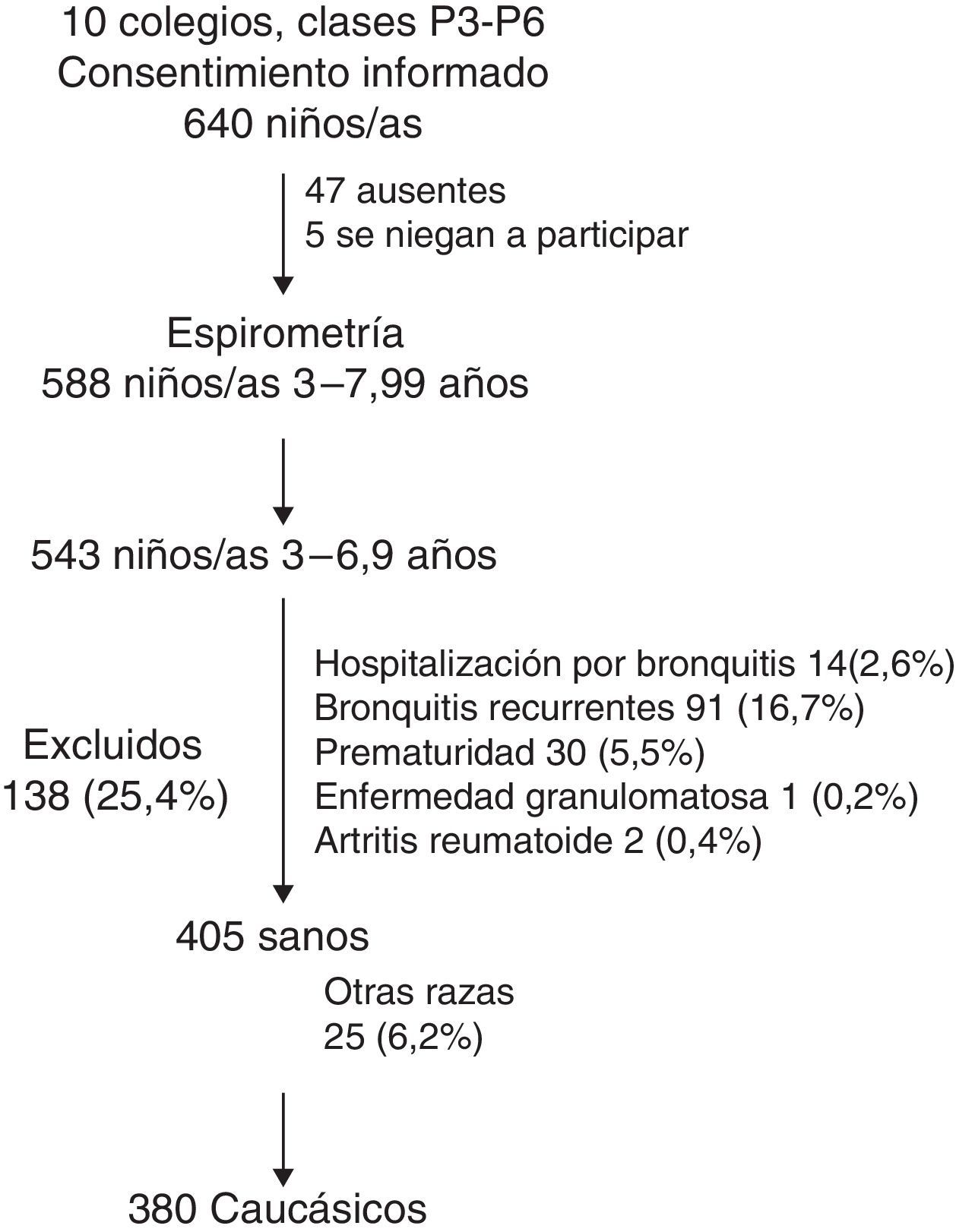
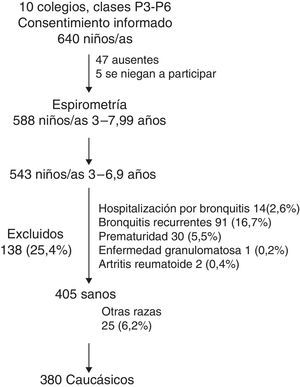
ResultsThe study was conducted in 10 schools with preschool and first grade classes. Fig. 1 depicts the inclusion of children in the study. Informed consent was signed by the parents of 640 children. At the time of the study, 47 were absent and 5 refused to participate. In total, 588 individuals performed spirometry, of whom 45 were excluded because they had already turned 7, and 138 (25.4%) due to underlying disease: 91 (16.7%) had (or had had) repeated episodes of bronchitis; 14 (2.6%) had been hospitalized for an episode of bronchitis; 30 (5.5%) were premature at birth; 1 had chronic granulomatous disease; and 2 had rheumatoid arthritis. Of the 405 healthy children who performed spirometry, 380 Caucasians were selected.
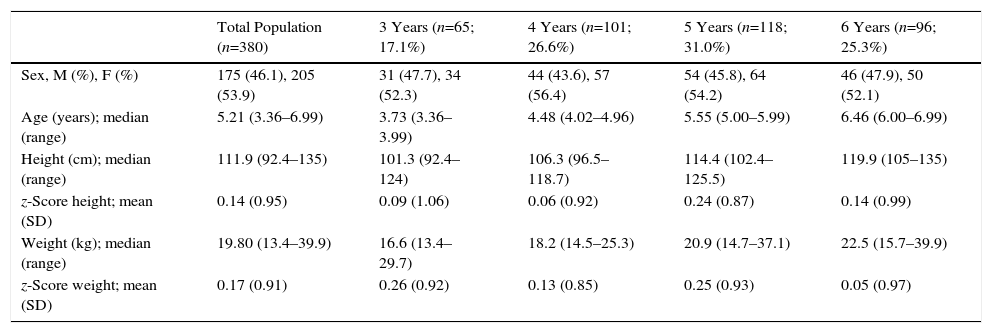
Table 1 summarizes the demographic characteristics of the 380 children. Median age was 5.21 years (range 3.36–6.99 years). Girls were slightly predominant (53.9%) and the 3-year-old group was somewhat less represented (17.1%). Weight and height z-scores for all age groups were within the normal range.
Demographic Characteristics of the 380 Children Included in the Study.
| Total Population (n=380) | 3 Years (n=65; 17.1%) | 4 Years (n=101; 26.6%) | 5 Years (n=118; 31.0%) | 6 Years (n=96; 25.3%) | |
|---|---|---|---|---|---|
| Sex, M (%), F (%) | 175 (46.1), 205 (53.9) | 31 (47.7), 34 (52.3) | 44 (43.6), 57 (56.4) | 54 (45.8), 64 (54.2) | 46 (47.9), 50 (52.1) |
| Age (years); median (range) | 5.21 (3.36–6.99) | 3.73 (3.36–3.99) | 4.48 (4.02–4.96) | 5.55 (5.00–5.99) | 6.46 (6.00–6.99) |
| Height (cm); median (range) | 111.9 (92.4–135) | 101.3 (92.4–124) | 106.3 (96.5–118.7) | 114.4 (102.4–125.5) | 119.9 (105–135) |
| z-Score height; mean (SD) | 0.14 (0.95) | 0.09 (1.06) | 0.06 (0.92) | 0.24 (0.87) | 0.14 (0.99) |
| Weight (kg); median (range) | 19.80 (13.4–39.9) | 16.6 (13.4–29.7) | 18.2 (14.5–25.3) | 20.9 (14.7–37.1) | 22.5 (15.7–39.9) |
| z-Score weight; mean (SD) | 0.17 (0.91) | 0.26 (0.92) | 0.13 (0.85) | 0.25 (0.93) | 0.05 (0.97) |
F: female; M: male; n: number of individuals; SD: standard deviation.
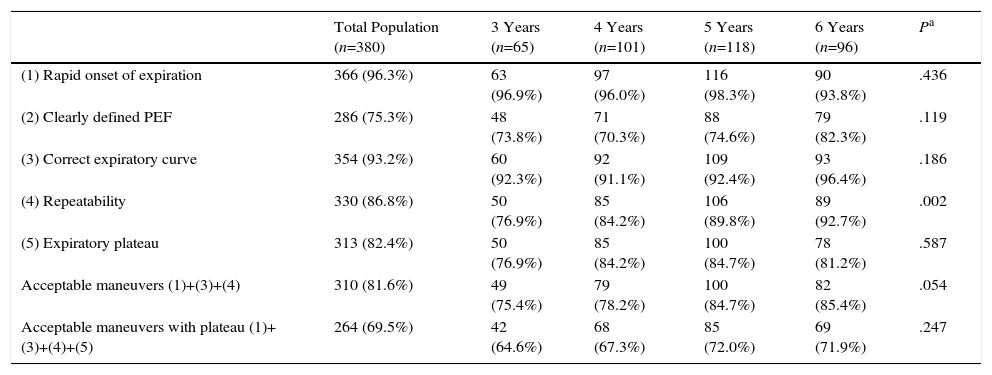
In total, 81.6% of the children (Table 2) presented a spirometry with quality criteria permitting the assessment of FEVt. Of the 380 children, 67.6% were able to perform FEV1 correctly, 78.9% FEV0.75, and 81.6% FEV0.5. Older children tended to achieve more valid maneuvers (75.4% in 3-year-olds vs 85.4% in 6-year-olds; P=.054). The percentage of spirometries with a correct plateau was 69.5%, with no differences observed between the different ages (64.6% in 3-year-olds vs 71.9% in 6-year-olds; P=.247).
Number of Children Achieving Correct Spirometric Maneuvers Meeting the Different Quality Criteria.
| Total Population (n=380) | 3 Years (n=65) | 4 Years (n=101) | 5 Years (n=118) | 6 Years (n=96) | Pa | |
|---|---|---|---|---|---|---|
| (1) Rapid onset of expiration | 366 (96.3%) | 63 (96.9%) | 97 (96.0%) | 116 (98.3%) | 90 (93.8%) | .436 |
| (2) Clearly defined PEF | 286 (75.3%) | 48 (73.8%) | 71 (70.3%) | 88 (74.6%) | 79 (82.3%) | .119 |
| (3) Correct expiratory curve | 354 (93.2%) | 60 (92.3%) | 92 (91.1%) | 109 (92.4%) | 93 (96.4%) | .186 |
| (4) Repeatability | 330 (86.8%) | 50 (76.9%) | 85 (84.2%) | 106 (89.8%) | 89 (92.7%) | .002 |
| (5) Expiratory plateau | 313 (82.4%) | 50 (76.9%) | 85 (84.2%) | 100 (84.7%) | 78 (81.2%) | .587 |
| Acceptable maneuvers (1)+(3)+(4) | 310 (81.6%) | 49 (75.4%) | 79 (78.2%) | 100 (84.7%) | 82 (85.4%) | .054 |
| Acceptable maneuvers with plateau (1)+(3)+(4)+(5) | 264 (69.5%) | 42 (64.6%) | 68 (67.3%) | 85 (72.0%) | 69 (71.9%) | .247 |
n: number of individuals; SD: standard deviation.
When quality criteria were analyzed separately, we observed that the older the children, the more they tended to achieve maneuvers with good repeatability (76.9% in 3-year-olds vs 92.7% in 6 year-olds; P=.002). No differences were observed in the remaining criteria (Table 2).
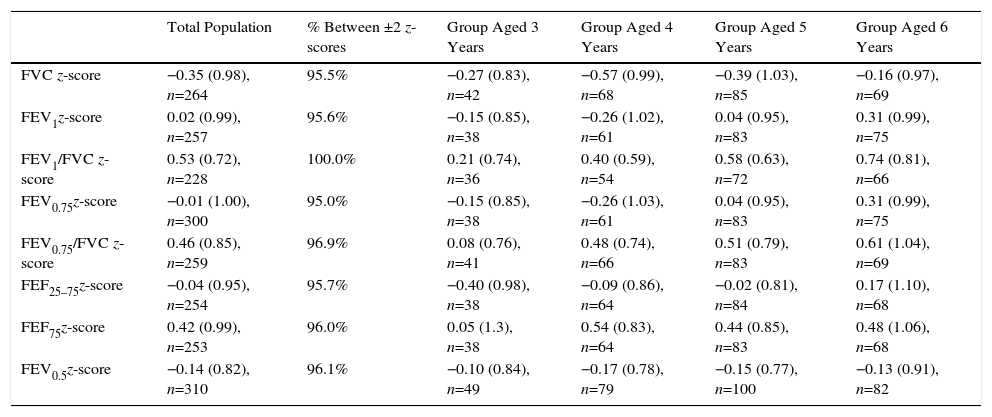
Table 3 lists the z-score values of the spirometric variables calculated according to the GLI-2012 equations in our overall population. As can be seen, all values are within ±0.5 z-scores, with the exception of FEV1/FVC (0.53 z-scores). At least 95% of all values were within ±2 z-scores.
z-Score Values of the Spirometric Variables Calculated According to GLI-2012 Equations by Total Population and Various Age Groups.
| Total Population | % Between ±2 z-scores | Group Aged 3 Years | Group Aged 4 Years | Group Aged 5 Years | Group Aged 6 Years | |
|---|---|---|---|---|---|---|
| FVC z-score | −0.35 (0.98), n=264 | 95.5% | −0.27 (0.83), n=42 | −0.57 (0.99), n=68 | −0.39 (1.03), n=85 | −0.16 (0.97), n=69 |
| FEV1z-score | 0.02 (0.99), n=257 | 95.6% | −0.15 (0.85), n=38 | −0.26 (1.02), n=61 | 0.04 (0.95), n=83 | 0.31 (0.99), n=75 |
| FEV1/FVC z-score | 0.53 (0.72), n=228 | 100.0% | 0.21 (0.74), n=36 | 0.40 (0.59), n=54 | 0.58 (0.63), n=72 | 0.74 (0.81), n=66 |
| FEV0.75z-score | −0.01 (1.00), n=300 | 95.0% | −0.15 (0.85), n=38 | −0.26 (1.03), n=61 | 0.04 (0.95), n=83 | 0.31 (0.99), n=75 |
| FEV0.75/FVC z-score | 0.46 (0.85), n=259 | 96.9% | 0.08 (0.76), n=41 | 0.48 (0.74), n=66 | 0.51 (0.79), n=83 | 0.61 (1.04), n=69 |
| FEF25–75z-score | −0.04 (0.95), n=254 | 95.7% | −0.40 (0.98), n=38 | −0.09 (0.86), n=64 | −0.02 (0.81), n=84 | 0.17 (1.10), n=68 |
| FEF75z-score | 0.42 (0.99), n=253 | 96.0% | 0.05 (1.3), n=38 | 0.54 (0.83), n=64 | 0.44 (0.85), n=83 | 0.48 (1.06), n=68 |
| FEV0.5z-score | −0.14 (0.82), n=310 | 96.1% | −0.10 (0.84), n=49 | −0.17 (0.78), n=79 | −0.15 (0.77), n=100 | −0.13 (0.91), n=82 |
FEV0.5 calculated according to All ages equations.
n: number of individuals; SD: standard deviation.
Data expressed as mean (SD).
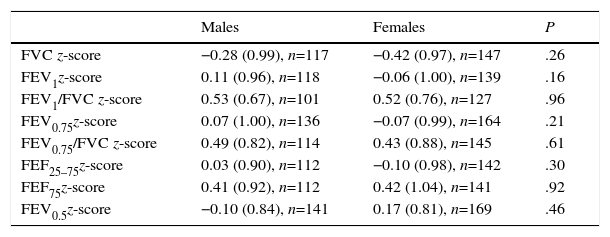
No significant differences were observed between values for the various spirometric variables by sex (Table 4), with all z-scores falling within ±0.5, except for FEV1/FVC in boys (0.53) and girls (0.52).
Comparison of z-Scores of Spirometric Variables According to Sex.
| Males | Females | P | |
|---|---|---|---|
| FVC z-score | −0.28 (0.99), n=117 | −0.42 (0.97), n=147 | .26 |
| FEV1z-score | 0.11 (0.96), n=118 | −0.06 (1.00), n=139 | .16 |
| FEV1/FVC z-score | 0.53 (0.67), n=101 | 0.52 (0.76), n=127 | .96 |
| FEV0.75z-score | 0.07 (1.00), n=136 | −0.07 (0.99), n=164 | .21 |
| FEV0.75/FVC z-score | 0.49 (0.82), n=114 | 0.43 (0.88), n=145 | .61 |
| FEF25–75z-score | 0.03 (0.90), n=112 | −0.10 (0.98), n=142 | .30 |
| FEF75z-score | 0.41 (0.92), n=112 | 0.42 (1.04), n=141 | .92 |
| FEV0.5z-score | −0.10 (0.84), n=141 | 0.17 (0.81), n=169 | .46 |
FEV0.5 calculated according to All ages equations. Data expressed as mean (SD).
n: number of individuals; SD: standard deviation.
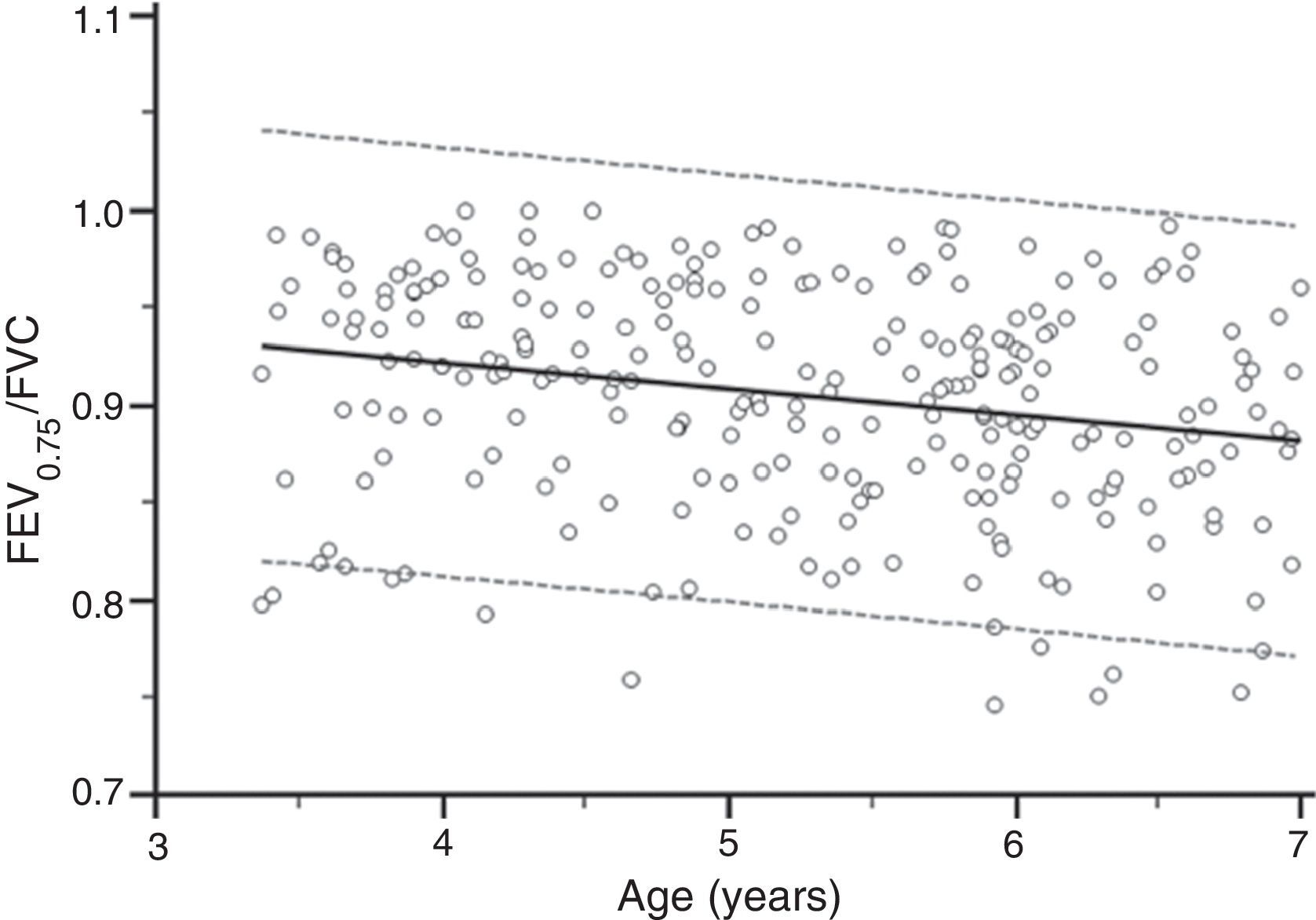
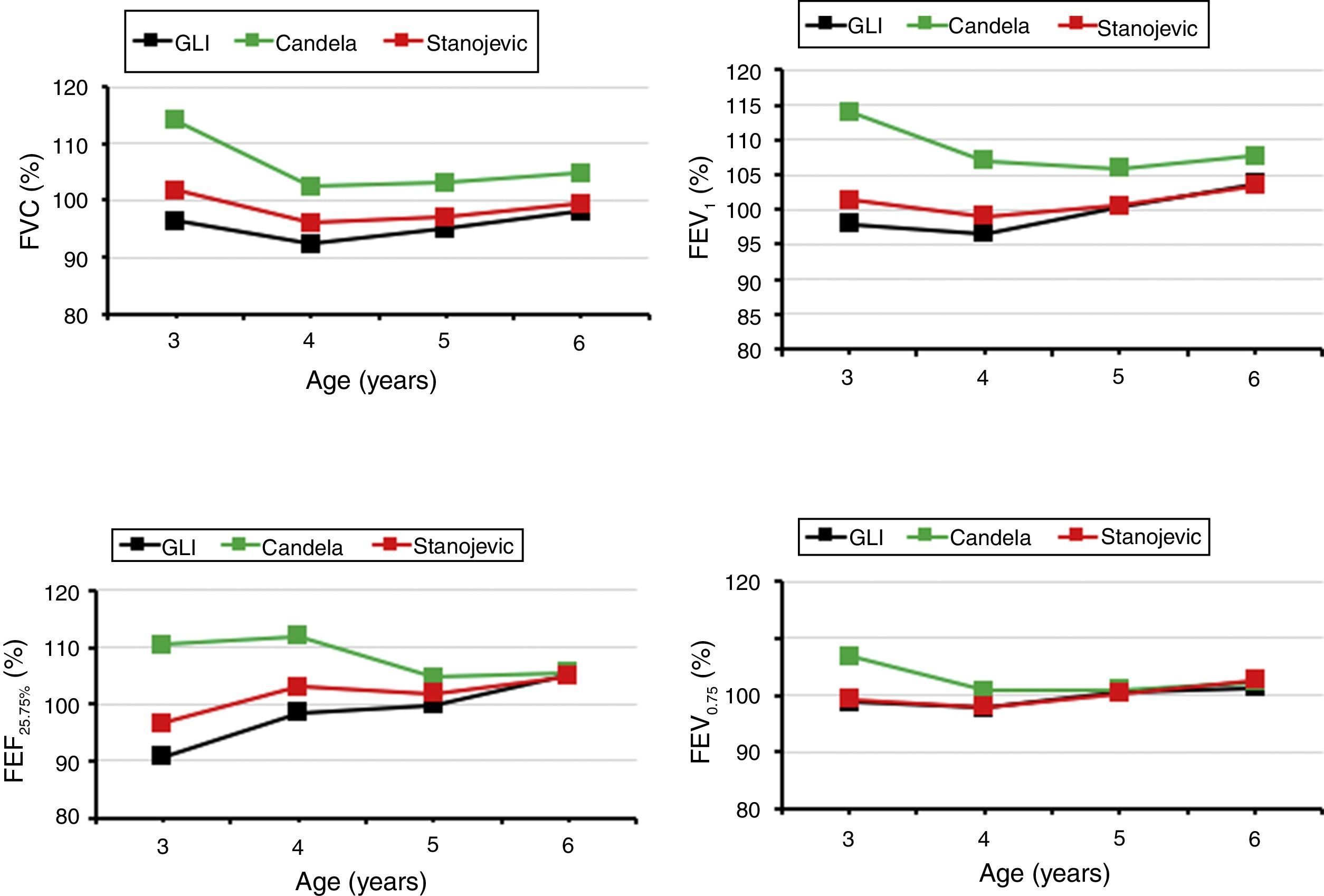
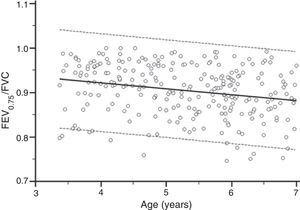
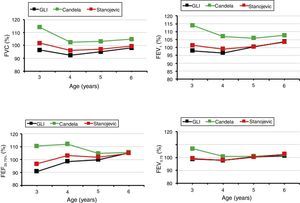
Fig. 2 shows the discreet relationship between FEV0.75/FVC ratio and age (r=0.24, P=.001), with a value of between 0.8 and 1, except in 7 children. Fig. 3 is a comparison between mean FVC, FEV1, FEV0.75, and FEF25%–75%, expressed as percentage of the predicted value for age, using the GLI-2012, All ages, and CANDELA equations. The All ages and GLI-2012 equations show a better fit with our population, whereas the values from the CANDELA equations deviated more from the 100% predicted value, particularly in 3- and 4-year-olds.
Our results indicate that the GLI-2012 and All ages equations for FEV0.5 are suitable for Spanish preschoolers of Caucasian ethnicity. In total, 81.6% of preschool children aged 3–6 years were able to perform a quality spirometry to assess FEVt, and 69.5% achieved spirometry with a correct plateau and FVC.
For many years, the most widespread criterion for the interpretation of spirometry has been the use of local reference values representative of the target population, selecting subjects in the same age group and race, and using different equations for different age groups: 3–6 years, 6–7 to 18–19 years, and adults. The CANDELA equations are currently recommended for preschool children in Spain.12 After the age of 7, other reference equations must be used, usually those developed by Casan et al.,26 but this can cause gaps and discontinuities in the values, and may lead to misinterpretations.14
GLI-2012 equations17 can continue to be used after 7 years of age and throughout adulthood. It is important that the GLI-2012 equations continue to be validated in older children. Since they were first published, they have been validated in British children aged 5–11 years from different ethnic groups,19 in a Caucasian population aged 4–80 years in Australia and New Zealand,20 and in a Norwegian population aged 12–90 years.27 However, in a German population aged 4–19 years, a good fit was observed for children younger than 10 years, but deviations were rather high for adolescent boys.28 Systematic deviations have also been observed in adults in studies conducted in Finland.29 This would suggest that the GLI-2012 equations may not be a perfect fit for some specific age ranges and certain populations. For this reason, validation studies should be performed before they are used systematically. In our series, we have seen that the GLI-2012 equations adapt better to our population than the CANDELA equations, particularly in children aged 3–4 years, in whom the CANDELA equations overestimate percentages of the predicted value.
The advantage of the statistical approach used to develop the GLI-2012 equations is that it takes into account the wide variability that occurs with age, which is greater in younger and in older individuals. Results expressed as z-scores and the precise definition of lower limits of normal for each age range allows results to be better categorized.18 As our results show, the FEVt/FVC ratio (Fig. 2) is greater than in adults, calling for equations that precisely define normal limits for each age group, instead of using fixed limits such as 0.7 that would lead to underdiagnosis, since at these ages the lower limit of normal is higher.
Our study confirms that quality spirometry can be obtained in preschool children with no prior training. The success rate (81.6% for FEVt and 69.5% for FVC) is similar to that of previous studies.30 The 2 parameters that the children achieved less frequently were a clearly defined PEF, although this parameter is not considered essential for analyzing the data obtained, and an adequate plateau. Repeatability was also difficult to achieve, and was lowest in 3-year-old children (76%).
In our study, we obtained a valid FEV1 in 67.6% of the children, a valid FEV0.75 in 78.9%, and a valid FEV0.5 in 81.6%. These results are similar to those of Neve et al.,31 who reported 69%, 82%, and 99%, and Santos et al.,32 who reported 65%, 86%, and 88%, respectively.
In preschool children aged 3–6 years, the GLI group33 recommends using FEV0.75 only, and this parameter was finally included in their calculations. They recommend that practitioners reserve FEV0.5 for infants and use FEV1 in children over 7 years of age.33 Due to changes in postnatal lung growth, the airways are relatively large in relation to lung volume, and infants expel air from the lungs during forced expiration in a very short time − less than 1 second − so FEV0.5 would provide a good picture of central and peripheral airway function in children younger than 2 years. In preschoolers, air is expelled rather more slowly, and lower lung volumes would be achieved somewhat later, so FEV0.75 may be more sensitive for reflecting changes in central and peripheral airways. In contrast, few children achieve FEV1, as occurred in our study, and the FEV1 value is often very similar to that of FVC, a fact that might limit its use in preschool children.33
The GLI developers also argue that FEV0.5 is of less use than FEV0.75 for discriminating between preschoolers with and without lung disease.33 However, although some studies have shown that FEV0.75 was more sensitive for identifying preschool children with lung disease than FEV0.5, others have found that FEV0.5 was useful for detecting lung disease,34 and it seems likely that this debate will continue. For this reason, we also validated the GLI-2012 equations for FEV1 and the All ages equations for FEV0.5, which at the time of the study were available in the software tools published by these groups.
One of the strengths of our study is that the inclusion criteria used allow our results to be extrapolated to the general population of children aged 3–6 years. We did not exclude children with risk factors such as exposure to tobacco smoke, pollution or a history of mild respiratory symptoms, such a previous episode of bronchitis. We did exclude children with more severe respiratory symptoms, such as hospitalization for bronchitis or repeated episodes of bronchitis, and children who had been born premature, factors which would clearly affect the results.35 Other strengths include strict adherence to international quality criteria for the performance of spirometry in preschool children and an appropriate sample size. One limitation of our study is the inclusion of Caucasian children and preschool children only, which prevents validation of the GLI equations from being extrapolated to other races or ages. While the equations show a very good fit for the overall population, we observed small deviations in the analysis of age subgroups, although the sample size had not been calculated for these subanalyses.
In conclusion, our study shows that the performance of valid spirometries meeting strict quality criteria is possible in preschool children. The GLI-2012 and All ages equations (for FEV0.5) are appropriate for Spanish preschool children of Caucasian ethnicity, so we recommend their use in this age group. These equations must continue to be validated in other age groups and ethnic groups to endorse their widespread use.
FundingThis study was conducted with the help of a grant from the Fundació Catalana de Pneumologia (FUCAP).
Conflict of InterestThe authors state that they have no conflict of interests.
We would like to thank the principals and teachers of the participating schools for their help and for their collaboration in the recruitment of the children. We also especially thank the parents and the children who participated in the study.
We are especially grateful for the advice and guidance of Prof. Janet Stocks in the design and conduct of the study.
The GLI-2012 equations and software tools for calculating values for individuals or data sets are available for consultation at the following links: www.lungfunction.org and http://www.ers-education.org/guidelines/global-lung-function-initiative.aspx.
The All ages equations for FEV0.5 were consulted on www.growinglungs.org.uk of the Asthma UK Spirometry Collaborative Group, not currently available for consultation. The equations, in Excel nomenclature, are as follows:
FEV0.5 males
z-Score FEV0.5 males=(((FEV0.5 observed/M)−1)/S)
M=EXP(−2.048+0.0156*height (cm)+0.049*age (years))
S=EXP(−1.847−0.0005*POWER (age (years);3))
FEV0.5 females
z-Score FEV0.5 females=(((FEV0.5 observed/M)−1)/S)
M=EXP(3.927−42.94*POWER (height (cm); −0.5)+0.000298*POWER (age (years);3))
S=EXP(−1.745−0.004*POWER (age (years);2))
Please cite this article as: Martín de Vicente C, de Mir Messa I, Rovira Amigo S, Torrent Vernetta A, Gartner S, Iglesias Serrano I, et al. Validación de las ecuaciones de referencia de la Global Lung Function Iniciative y All ages para la espirometría forzada en niños sanos preescolares españoles. Arch Bronconeumol. 2018;54:24–30.