Congenital unilateral pulmonary vein atresia with no other cardiac abnormalities is a very rare entity.1,2 It usually presents in childhood or adolescence as recurrent episodes of lung infection or hemoptysis, and is an exceptional finding in adults. We have only found 11 cases in the literature to date (including our own).
We present the case of a 43-year-old man, who we examined after admission for pneumonia. His medical history included type 1 diabetes and congenital right pulmonary venous atresia diagnosed in childhood, with no subsequent follow-up. This was the third episode of pneumonia in the right upper lobe in 2 years. He also reported small-volume hemoptysis daily, and dyspnea on major exertion. Decreased breath sounds were observed throughout the right hemithorax on auscultation, with persistent wheezing in the anterior axillary line.
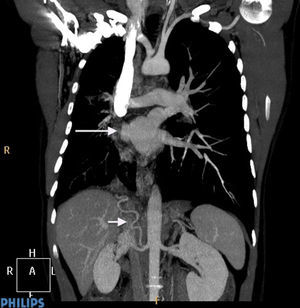
Chest radiograph showed a resolving consolidation together with decreased right lung volume with a mediastinal shift to that side. The computed tomography (CT) scan is shown in Fig. 1. Bronchoscopy was performed, with the following findings: absence of right upper lobe bronchus; in its place was the opening of 2 accessory bronchi that prevented the bronchoscope from advancing. The opening of the apical and paracardiac bronchus of the right lower lobe could not be seen either. Spirometry revealed a moderately restrictive pattern, while the echocardiogram showed mild aortic stenosis with no pulmonary hypertension findings.
Finally, an angiography was performed. This confirmed all the findings described in the CT and also showed that part of the collateral system formed to supply the right lung came from an inferior phrenic artery (Fig. 1).
After the study was completed, the case was discussed in a meeting with the thoracic surgery and vascular surgery departments, where it was decided that the most appropriate therapeutic option was pneumonectomy.
Unilateral pulmonary vein atresia occurs due to failure of incorporation of the common pulmonary vein into the left atrium. It is associated with other cardiac abnormalities in up to 50% of cases, and may occur in either lung.1,2
The clinical spectrum ranges from asymptomatic patients3 to the development of pulmonary hypertension2 and death. Diagnosis is confirmed by pulmonary angiography. However, modern techniques such as CT scan or magnetic resonance imaging together with symptoms consistent with the condition may now be sufficient to make the diagnosis.4
There are 3 therapeutic options proposed in the literature. Pneumonectomy has been shown to control symptoms, and to prevent pulmonary hypertension.1,5 Another, less aggressive, therapeutic option is coil embolization of the systemic arterial collateral vessels. In the article by Heyneman et al.,2 this procedure controlled hemoptysis in one of the patients, who subsequently remained asymptomatic. The third option, in cases of asymptomatic patients or those with few symptoms, is follow-up, focusing particularly on the early detection of pulmonary hypertension.
Please cite this article as: Santos-Morano J, Rodríguez-Hernández S, Hilares-Vera JI. Atresia congénita unilateral de venas pulmonares en adultos. Descripción de un caso y revisión de la literatura. Arch Bronconeumol. 2015;51:423–424.