The distribution of chronic obstructive pulmonary disease (COPD) in women, and its underdiagnosis and determinants in the general population, have not been well described. The EPI-SCAN study is an epidemiologic, observational study conducted at 11 Spanish centers on the general population aged 40–80.
Patients and methodThis paper describes the rates and extrapolates the population burden from the 3802 participants of the EPI-SCAN study.
ResultsWith 2005 female and 1797 male participants, there was a lower prevalence of COPD in women (5.7%; 95% CI, 4.7–6.7) than in men (15.1%; 95% CI, 13.5–16.8; P<.05). Among the 386 participants with COPD, 114 (29.5%) were women, who were younger, currently smoked less and had lower tobacco smoke exposure, while reporting a lower level of education (P<.05). As for the respiratory symptoms, there were no differences between sexes for cough, dyspnea or wheezing, but the women with COPD reported sputum less frequently (P<.05). There were no differences in the spirometric severity of COPD between women and men. Overall, 73% of the patients with spirometric COPD criteria were underdiagnosed, and this percentage is unevenly distributed by sex, being 1.27 times more frequent in women (86.0%) than in men (67.6%) (P<.05). By extrapolating the rates of prevalence and underdiagnosis of COPD to the general population, we estimate that there are 628102 Spanish women between the ages of 40 and 80 with COPD, 540168 of whom still have not been diagnosed.
ConclusionsThere is a greater underdiagnosis of COPD in women than in men in Spain.
La distribución de la enfermedad pulmonar obstructiva crónica (EPOC) en mujeres y su infradiagnóstico y determinantes en la población no están bien descritos. El estudio EPI-SCAN es un estudio epidemiológico, observacional, realizado en 11 centros españoles en la población general de edades entre 40 y 80 años.
Pacientes y métodoEn este trabajo se describen las tasas y se extrapola la carga poblacional a partir de los 3.802 participantes del estudio EPI-SCAN.
ResultadosCon 2.005 mujeres y 1.797 hombres participantes, se obtuvo una prevalencia de EPOC inferior en mujeres (5,7%; IC 95%, 4,7–6,7) que en hombres (15,1%; IC 95%, 13,5-16,8; p<0,05). Entre los 386 participantes con EPOC, las 114 (29,5%) mujeres eran más jóvenes, menos fumadoras actualmente y tenían menor exposición tabáquica, y referían menos nivel de estudios (p<0,05). Respecto a los síntomas respiratorios, no existían diferencias por sexo en tos, disnea o sibilantes, pero las mujeres con EPOC referían esputo menos frecuentemente (p<0,05). No existían diferencias en la gravedad espirométrica de la EPOC entre mujeres y hombres. El 73% de los pacientes con criterios de EPOC fueron infradiagnosticados, y este porcentaje se distribuye desigualmente por sexo, siendo 1,27 veces más frecuente en mujeres (86,0%) que en hombres (67,6%) (p<0,05). Extrapolando las tasas de prevalencia e infradiagnóstico de EPOC a la población, se estima que en España entre las mujeres con edades comprendidas entre 40 y 80 años existirían 628.102 mujeres con EPOC, de las cuales 540.168 aún estarían sin diagnosticar.
ConclusionesLa EPOC está más infradiagnosticada en mujeres que en hombres en España.
The main risk factors for chronic obstructive pulmonary disease (COPD) are a history of tobacco smoking and aging.1 Current projections indicate that in Spain, population aging (with a special effect in women due to their greater longevity) and the massive incorporation of women to smoking in the 1960–70s is already causing an epidemiological change, increasing smoking-related chronic diseases, particularly COPD,2 which in women has been receiving growing interest in the literature.3–8
In 2007, the EPI-SCAN study found that the prevalence of COPD in Spain was 10.2% (15.1% in men and 5.6% in women) of the population aged 40–80 years.9 Previously, the IBERPOC study, conducted in 1997, found a COPD prevalence of 9.1% (14.3% in men and 3.9% in women).10 Both studies used different spirometric definitions and some modifications in the sampling methodology,11 but the difference in the prevalence of COPD by gender remained, and significant geographical variability was demonstrated in the distribution of COPD.12
The determinants of underdiagnosis of COPD according to sex have received relatively a little attention to date, since most international initiatives on COPD such as the Latin American Project for the Investigation of Obstructive Lung Disease (PLATINO)13 and the Burden of Obstructive Lung Disease (BOLD),14 only describe the prevalence by sex, without even referring to underdiagnosis/undertreatment in women.
The aim of this study was to quantify the distribution of COPD, its underdiagnosis and determinants in women in Spain, and to provide a list of actions to reduce the expected imbalance in the management of COPD by sex, for both national and international use.
MethodsThe methodology and protocol used in the EPI-SCAN study have been previously described in detail.15 Briefly, EPI-SCAN is a Spanish national epidemiological, observational, multicenter population-based cross-sectional study with random participant selection using two-phase sampling, and stratified by areas close to the participating centers. These centers were selected according to four Spanish geographical areas (North, Mediterranean Coastal, South and Center), namely: Barcelona, Burgos, Córdoba, Huesca, Madrid (two centers), Oviedo, Seville, Valencia, Vic and Vigo. Study sampling was two-phase, population-based and random; it was carried out by telephone survey and included men and women from the general population aged between 40 and 80 years and resident in Spain. The field work was carried out between May 2006 and July 2007. The study was authorized by the relevant Ethics Committees, and all participants voluntarily agreed in writing to undergo the study tests.
Information on sociodemographic data, smoking habits, previous diagnosis of respiratory diseases and other pathologies, COPD exacerbations, dyspnea scale, and treatment for respiratory diseases was collected, among other variables. The presence of respiratory symptoms (habitual cough on rising, frequent sputum and occasional presence of dyspnea and wheezing) was collected using the Spanish version of the European Community for Coal and Steel (ECSC) questionnaire.16 Forced spirometry was performed using the Master Scope CT (VIASYS Healthcare, Hoechberg, Germany). Acceptability and reproducibility criteria, and selection of the maneuver, proposed in the most recent American Thoracic Society/European Respiratory Society (ATS/ERS) recommendations17 were employed; ECSC reference values were used.18 The maneuvers were repeated 15–30min after the inhalation of 200mcg of salbutamol. Using the criteria in the ATS/ERS guidelines,19 the bronchodilator test was considered positive when an increase in FEV1 or FVC >200ml and greater than 12% with respect to baseline was recorded. ECSC reference values were used to calculate the predicted spirometry values.18 COPD was defined as a post-bronchodilator FEV1/FVC ratio <0.70, and in a sub-analysis also as a post-bronchodilator FEV1/FVC below the lower limit of normal (LLN).
Statistical AnalysisThe EPI-SCAN study was conducted based on the following sample size calculation: a COPD prevalence of 12% was estimated, with precision ±1%. Assuming 20% losses, the theoretical number of individuals for inclusion in the study was 5071. Considering a posteriori that among the 11 areas in EPI-SCAN, the mean number of participants was 345 per area, with a maximum of 439 in Burgos and a minimum of 136 in Asturias, there was statistical power for most area comparisons with respect to the mean. As this was a descriptive population study, participation quotas by sex or other variables were not set. The estimator and its 95% confidence interval are presented in most of the analyses. The results for each variable are presented as mean and standard deviation in the case of continuous variables, and using the number of cases in each category and the relative frequency of the total number of responses in the case of categorical variables.
To quantify the number of COPD cases in the population, the rates obtained in EPI-SCAN were standardized according to the age and sex distribution of the Spanish population from official statistics.20 Statistical significance was analyzed by performing an initial ANOVA and then a two-sided test for continuous variables and a Chi2 test for categorical variables.
Finally multivariate analysis by logistic regression of the EPI-SCAN variable “being previously diagnosed with COPD” in the subsample of COPD individuals according to GOLD is presented, exploring, in addition to sex, the following factors by relative risk and 95% confidence interval (RR, 95% CI): age, smoking, education level, mMRC dyspnea, GOLD COPD severity, Charlson index and having performed previous spirometry. A statistical significance level of less than 0.05 was used in all statistical tests.
ResultsOf a total of 4274 subjects chosen randomly by telephone in the eleven centers, 3885 (90.9%) agreed to participate in the study; a sample of 3802 (88.9%) patients were eventually available for the analysis (minimum data set on sex, age and lung function). As presented previously,9 the 389 (9.1%) individuals who refused to participate in the survey were slightly older and more often women, including more non-smokers and ex-smokers.
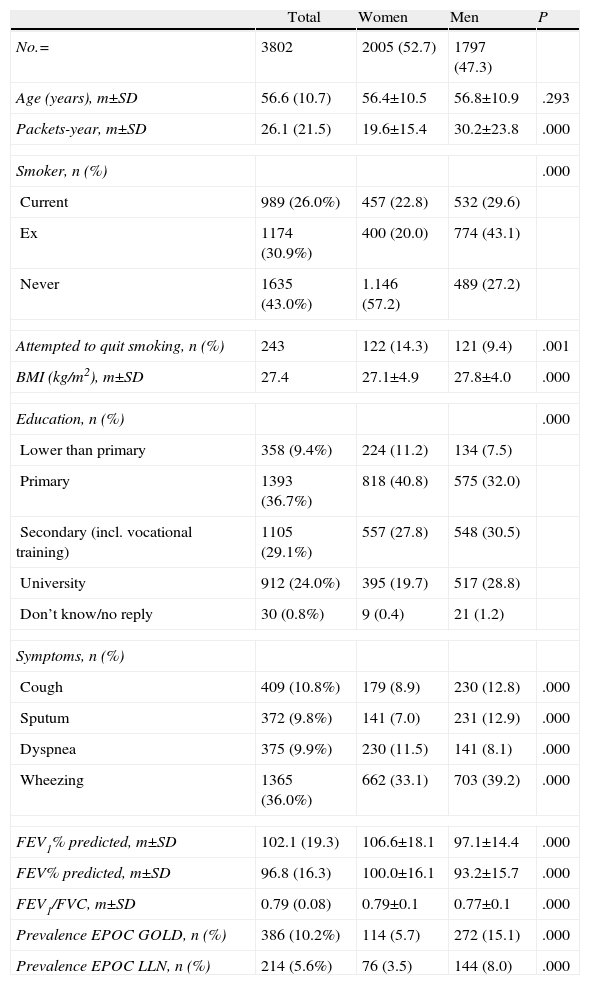
The sociodemographic and clinical characteristics of the 3802 participants in the EPI-SCAN study corresponded to 2005 women and 1797 men (Table 1). Except for the mean age of 56.6±10.7 years, where there were no differences by sex, the other sociodemographic and clinical variables differed between women and men. There were fewer smokers among the women and they had less exposure to tobacco smoke, had tried to quit smoking more often and reported a lower education level (P<.05). Likewise, women in the general population reported fewer respiratory symptoms such as cough, sputum or wheezing, but more dyspnea (P<0.05). With respect to spirometry, they had a wider distribution of FEV1 (%), FVC (%) and FEV1/FVC ratio values than men (P<.05). Finally, women had a lower prevalence of COPD than men, using both the GOLD (5.7% in women [95% CI 4.7–6.7] and 15.1% in men [95% CI 13.5–16.8]) and LLN criteria (3.5% in women [95% CI 2.7–4.4] vs 8.0% in men [95% CI 6.8–9.4]), both P<.05.
Sociodemographic and Clinical Characteristics in Participants of the EPI-SCAN Study, by Sex.
| Total | Women | Men | P | |
| No.= | 3802 | 2005 (52.7) | 1797 (47.3) | |
| Age (years), m±SD | 56.6 (10.7) | 56.4±10.5 | 56.8±10.9 | .293 |
| Packets-year, m±SD | 26.1 (21.5) | 19.6±15.4 | 30.2±23.8 | .000 |
| Smoker, n (%) | .000 | |||
| Current | 989 (26.0%) | 457 (22.8) | 532 (29.6) | |
| Ex | 1174 (30.9%) | 400 (20.0) | 774 (43.1) | |
| Never | 1635 (43.0%) | 1.146 (57.2) | 489 (27.2) | |
| Attempted to quit smoking, n (%) | 243 | 122 (14.3) | 121 (9.4) | .001 |
| BMI (kg/m2), m±SD | 27.4 | 27.1±4.9 | 27.8±4.0 | .000 |
| Education, n (%) | .000 | |||
| Lower than primary | 358 (9.4%) | 224 (11.2) | 134 (7.5) | |
| Primary | 1393 (36.7%) | 818 (40.8) | 575 (32.0) | |
| Secondary (incl. vocational training) | 1105 (29.1%) | 557 (27.8) | 548 (30.5) | |
| University | 912 (24.0%) | 395 (19.7) | 517 (28.8) | |
| Don’t know/no reply | 30 (0.8%) | 9 (0.4) | 21 (1.2) | |
| Symptoms, n (%) | ||||
| Cough | 409 (10.8%) | 179 (8.9) | 230 (12.8) | .000 |
| Sputum | 372 (9.8%) | 141 (7.0) | 231 (12.9) | .000 |
| Dyspnea | 375 (9.9%) | 230 (11.5) | 141 (8.1) | .000 |
| Wheezing | 1365 (36.0%) | 662 (33.1) | 703 (39.2) | .000 |
| FEV1% predicted, m±SD | 102.1 (19.3) | 106.6±18.1 | 97.1±14.4 | .000 |
| FEV% predicted, m±SD | 96.8 (16.3) | 100.0±16.1 | 93.2±15.7 | .000 |
| FEV1/FVC, m±SD | 0.79 (0.08) | 0.79±0.1 | 0.77±0.1 | .000 |
| Prevalence EPOC GOLD, n (%) | 386 (10.2%) | 114 (5.7) | 272 (15.1) | .000 |
| Prevalence EPOC LLN, n (%) | 214 (5.6%) | 76 (3.5) | 144 (8.0) | .000 |
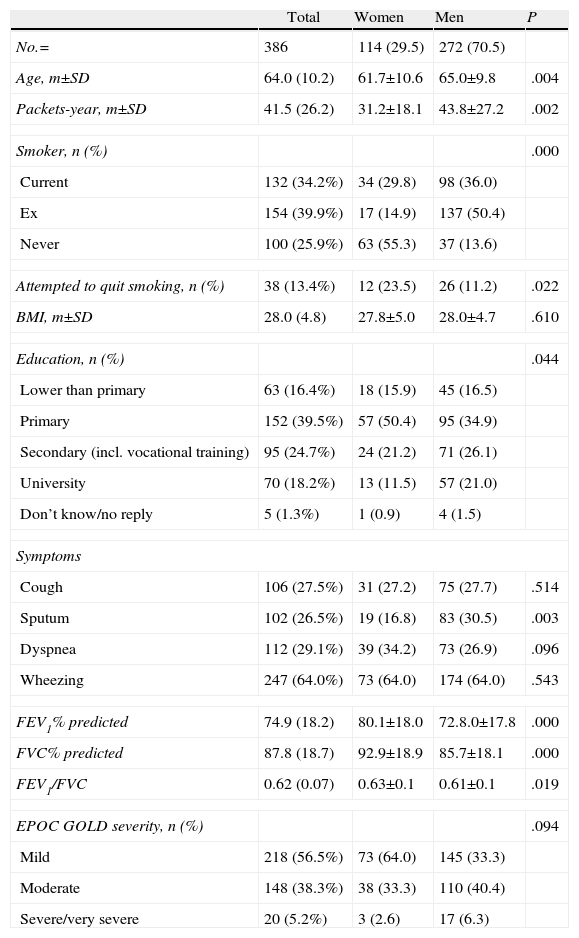
Among the 386 participants with COPD (GOLD criteria), the 114 (29.5%) women were younger, there were fewer smokers and they had less exposure to tobacco smoke, but they reported more attempts to quit smoking (Table 2). They also reported a lower level of education (P<.05). With respect to respiratory symptoms, there were no differences by sex in cough, dyspnea or wheezing, but women with COPD reported sputum less often (P<.05). With respect to spirometry, again women had a wider distribution of FEV1 (% predicted), FVC (% predicted) and FEV1/FVC ratio values than men (P<.05). There were no differences in the spirometric severity of COPD between women and men.
Characteristics of the COPD Individuals (According to GOLD) in the EPI-SCAN Study, by Sex.
| Total | Women | Men | P | |
| No.= | 386 | 114 (29.5) | 272 (70.5) | |
| Age, m±SD | 64.0 (10.2) | 61.7±10.6 | 65.0±9.8 | .004 |
| Packets-year, m±SD | 41.5 (26.2) | 31.2±18.1 | 43.8±27.2 | .002 |
| Smoker, n (%) | .000 | |||
| Current | 132 (34.2%) | 34 (29.8) | 98 (36.0) | |
| Ex | 154 (39.9%) | 17 (14.9) | 137 (50.4) | |
| Never | 100 (25.9%) | 63 (55.3) | 37 (13.6) | |
| Attempted to quit smoking, n (%) | 38 (13.4%) | 12 (23.5) | 26 (11.2) | .022 |
| BMI, m±SD | 28.0 (4.8) | 27.8±5.0 | 28.0±4.7 | .610 |
| Education, n (%) | .044 | |||
| Lower than primary | 63 (16.4%) | 18 (15.9) | 45 (16.5) | |
| Primary | 152 (39.5%) | 57 (50.4) | 95 (34.9) | |
| Secondary (incl. vocational training) | 95 (24.7%) | 24 (21.2) | 71 (26.1) | |
| University | 70 (18.2%) | 13 (11.5) | 57 (21.0) | |
| Don’t know/no reply | 5 (1.3%) | 1 (0.9) | 4 (1.5) | |
| Symptoms | ||||
| Cough | 106 (27.5%) | 31 (27.2) | 75 (27.7) | .514 |
| Sputum | 102 (26.5%) | 19 (16.8) | 83 (30.5) | .003 |
| Dyspnea | 112 (29.1%) | 39 (34.2) | 73 (26.9) | .096 |
| Wheezing | 247 (64.0%) | 73 (64.0) | 174 (64.0) | .543 |
| FEV1% predicted | 74.9 (18.2) | 80.1±18.0 | 72.8.0±17.8 | .000 |
| FVC% predicted | 87.8 (18.7) | 92.9±18.9 | 85.7±18.1 | .000 |
| FEV1/FVC | 0.62 (0.07) | 0.63±0.1 | 0.61±0.1 | .019 |
| EPOC GOLD severity, n (%) | .094 | |||
| Mild | 218 (56.5%) | 73 (64.0) | 145 (33.3) | |
| Moderate | 148 (38.3%) | 38 (33.3) | 110 (40.4) | |
| Severe/very severe | 20 (5.2%) | 3 (2.6) | 17 (6.3) | |
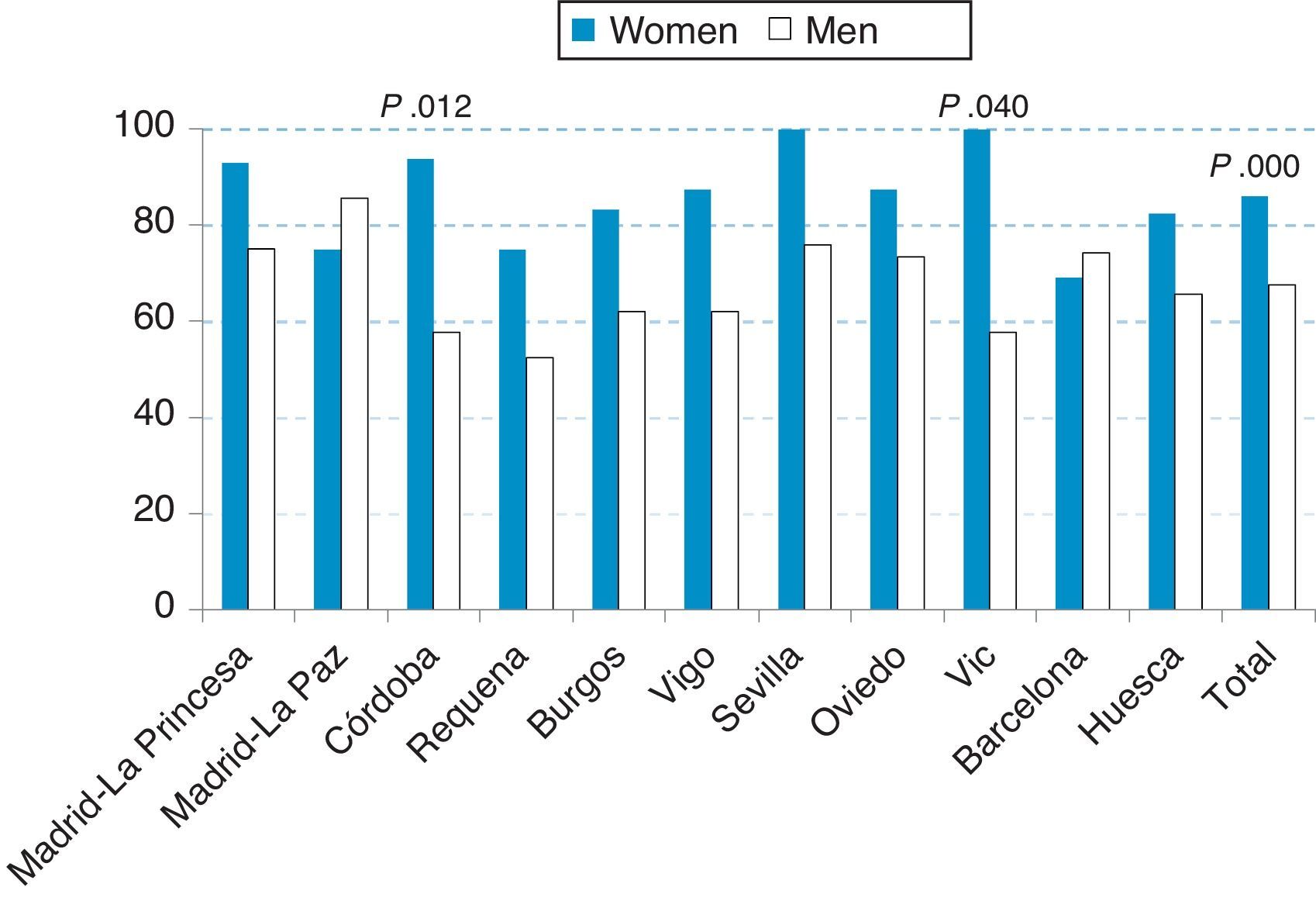
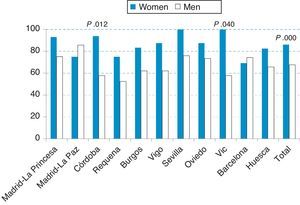
As can be seen in Fig. 1, 73% of the underdiagnosis of airflow limitation compatible with COPD in EPI-SCAN was distributed unequally by sex, and was 1.27-fold more frequent in women (86.0%) than in men (67.6%) (P<.05). In two EPI-SCAN areas, Seville and Vic, 100% of the participants with COPD were underdiagnosed; similarly, in Madrid-La Princesa and Córdoba it exceeded 90%. By contrast, the greatest underdiagnosis of COPD in men occurred in Madrid La Paz (85.7%) and Seville (75.9%). Comparatively, the participating centers with better (lower) rates of underdiagnosis were Requena (57.7%) in men and Barcelona (69.2%) in women. Within the eleven areas, the differences in underdiagnosis of COPD by sex were significant in Córdoba (93.8% in women vs 57.7% in men) and in Vic (100.0% in women vs 57.7% in men), P<.05.
Extrapolating the prevalence and underdiagnosis rates of COPD to the Spanish population, it is estimated that among the 11 million women and 10.4 million men in Spain aged between 40 and 80 years, there are 2185764 people with COPD in Spain, corresponding to 628102 women and 1571868 men, of whom 540168 women and 1062583 men are still undiagnosed.
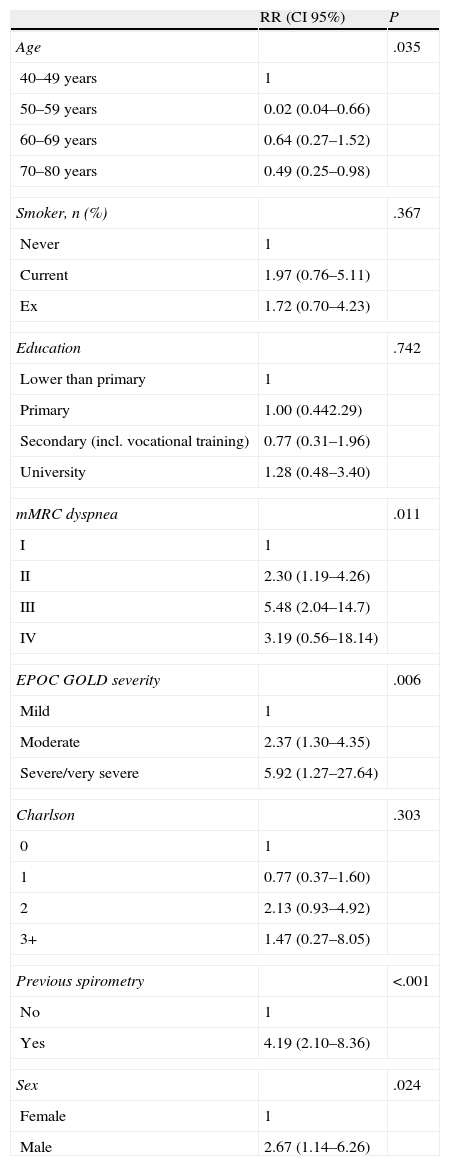
Finally, multivariate analysis of the factors potentially associated with being previously diagnosed with COPD is presented, performed in the 386 COPD GOLD individuals in EPI-SCAN (Table 3). It can be observed that even adjusting for variables with high clinical and statistical significance, such as having performed previous spirometry (P<.001), increasing COPD GOLD severity (P=.006), mMRC dyspnea (P=.001) and age (P=.035), and other non-significant variables in the model such as smoking, education level and Charlson index (P>.05 in all), being female continued to be an independent factor for having underdiagnosed COPD, with RR=2.67 (95% CI 1.14–6.26).
Factors Associated With being Diagnosed Previously With COPD in COPD Individuals (According to GOLD) in the EPI-SCAN Study (RR and CI 95%).
| RR (CI 95%) | P | |
| Age | .035 | |
| 40–49 years | 1 | |
| 50–59 years | 0.02 (0.04–0.66) | |
| 60–69 years | 0.64 (0.27–1.52) | |
| 70–80 years | 0.49 (0.25–0.98) | |
| Smoker, n (%) | .367 | |
| Never | 1 | |
| Current | 1.97 (0.76–5.11) | |
| Ex | 1.72 (0.70–4.23) | |
| Education | .742 | |
| Lower than primary | 1 | |
| Primary | 1.00 (0.442.29) | |
| Secondary (incl. vocational training) | 0.77 (0.31–1.96) | |
| University | 1.28 (0.48–3.40) | |
| mMRC dyspnea | .011 | |
| I | 1 | |
| II | 2.30 (1.19–4.26) | |
| III | 5.48 (2.04–14.7) | |
| IV | 3.19 (0.56–18.14) | |
| EPOC GOLD severity | .006 | |
| Mild | 1 | |
| Moderate | 2.37 (1.30–4.35) | |
| Severe/very severe | 5.92 (1.27–27.64) | |
| Charlson | .303 | |
| 0 | 1 | |
| 1 | 0.77 (0.37–1.60) | |
| 2 | 2.13 (0.93–4.92) | |
| 3+ | 1.47 (0.27–8.05) | |
| Previous spirometry | <.001 | |
| No | 1 | |
| Yes | 4.19 (2.10–8.36) | |
| Sex | .024 | |
| Female | 1 | |
| Male | 2.67 (1.14–6.26) | |
This study highlights that COPD is a major health problem in women, both at population and individual level. Among all the EPI-SCAN participants, women with COPD reported the same level of respiratory symptoms and spirometric severity as men with COPD, even though they were younger, fewer were current smokers and they had less exposure to tobacco smoke; they also reported a lower education level. However, women had greater underdiagnosis of COPD (1.27-fold) and in some EPI-SCAN participating areas, almost all were underdiagnosed. As previously stated, extrapolating the rates of COPD prevalence and underdiagnosis to the population, it is estimated that in Spain, among women aged between 40 and 80 years, there are 628102 women with COPD, of whom 540168 are still undiagnosed. In short, after adjusting for other sociodemographic and clinical values, being female is an independent factor with RR=2.67 (95% CI 1.14–6.26) of having underdiagnosed COPD.
Although COPD is still clinically diagnosed more in men than in women, mainly due to the secular effects of exposure to tobacco smoke in the Western population, we can begin to see an epidemiological change. Due to the delay of up to 20 years in the mass initiation of women smoking in the twentieth century, even though the transition occurred in different ways in different countries,21 an increase can be expected in all chronic diseases associated with aging and smoking which will be disproportionally greater in women than in men.
Context and Literature ReviewIn Spain, the IBERPOC study, conducted with a similar methodology 10 years before EPI-SCAN, observed a prevalence of COPD in women of 3.9% using the lower limit of normal,10 which is almost equal to the 3.5% observed in EPI-SCAN with the same criteria. In IBERPOC, 22% of COPD cases detected were women, compared with 29% in EPI-SCAN. It was also observed in the IBERPOC study that being female was significantly and independently associated with a higher risk of not being previously diagnosed with COPD.10 Comparing these new results with the IBERPOC results, women continue to have a 1.3-fold increased risk (95% CI 0.3–6.2) of having underdiagnosed COPD. In the IBERPOC study, a large percentage of newly diagnosed COPD cases occurred in women with little exposure to tobacco smoke and respiratory symptoms. Therefore, it can be concluded that the situation has not improved in 10 years. In comparison with the PLATINO study, where underdiagnosis of COPD exceeded 88%, the factors associated independently with underdiagnosis were younger age, less severity of airway obstruction (lower GOLD severity), fewer respiratory symptoms (cough, sputum, wheezing and difficulty breathing), and no prior diagnosis of asthma; however, women in the PLATINO study did not show significant differences in underdiagnosis of COPD with respect to men, with 1.38 (95% CI 0.76–2.52, P=.29).22 The PLATINO study including other population studies (mostly in a recent review in these pages)7 indicates that overall the prevalence of COPD in women is lower than that in men. For example, in the multicentre BOLD study,14 the prevalence of COPD in women varied between 7.6% in Guangzhou, China and 25.7% in Salzburg, Austria, while the prevalence of COPD in men varied between 15.3% in Guangzhou, China (i.e. twice that in women there) and a maximum of 28.7% in Capetown, South Africa.14
The last Spanish National Health Survey in 2009 estimated the prevalence of smoking at 26.4% of the population aged over 16 years, with a clear difference between men (31.17%) and women (21.33%), regardless of the Autonomous Region.23 In the absence of more recent data, a slow progressive decline in the number of smokers has been observed in the general population in recent years,24 and the mean age for starting smoking is an average of 21.32 years (20.76 in men and 22.10 in women), which, compared with the 2006 National Health Survey, shows that an average delay of almost four years has been achieved in the age at which individuals start smoking; this is greater than four years in the case of women (in 2006, it was 17.04 in men and 17.78 in women).
It is estimated that more than 18 thousand people in Spain die each year due to COPD, of which one quarter (more than 4500) are women.25 In Spain, the latest data available are from 2009. According to these data, COPD is the fifth leading cause of death among men, with an annual rate of 44.0 deaths per 100000 persons, and the seventh leading cause for women, with an annual rate of 14.2 deaths per 100000 persons. In comparison, Spain is in the intermediate range within the European Union, headed by some Eastern European and Anglo-Saxon countries. Among the 19 European countries with available data, we are in eighth position in terms of mortality due to COPD in men and are among the lowest in women.26 The morbidity and use of healthcare resources associated with COPD in Spain are high.27
Irrespective of the disease, the estimated prevalence in the population depends on the definition used for its diagnosis. In the case of COPD, different approaches have historically been used, including the following: medical diagnosis, diagnosis based on the presence of respiratory symptoms, and diagnosis based on the presence of airflow limitation (with or without a bronchodilator test). Each of these methods will produce very different results. Up until 2000, international COPD guidelines such as those of the European Respiratory Society28 recommended different spirometric thresholds for defining COPD in women, such as FEV1/FVC ratio <88% in men and <89% in women. Nowadays, the use of new sex-specific reference equations29 has eliminated this distinction.
Currently in Spain, more women (42.7%) than men (40.8%) smoke between the ages of 16 and 24 years.23 This is a new and disturbing phenomenon in the history of tobacco use in Spain, which has also been observed in the young population in other developing countries in recent years. In the 25–44 years old age group, almost half are smokers (52.6% of men vs 43.5% of women). Proper implementation of recent legislative measures such as Act 42/2010,30 which came into effect on 2 January 2011, limiting the use of tobacco in public places and its advertising, should have an impact not only on greater protection for non-smokers, but also on a future reduction in smoking in the Spanish population, as has been observed in Ireland, Italy and California. Furthermore, Spanish population growth is expected to peak in 2050, with 53 million inhabitants, with peak aging around 2060,31 resulting in an increase in the population at risk of developing irreversible airflow obstruction. Our results agree with those obtained recently by Naberán et al.,32 who concluded in a patient population in Primary Care centers and hospitals in Spain that women with COPD were younger, smoked less and had better lung function than men; they also observed that they had poorer quality of life (measured by EuroQoL and AQ20) and more often associated anxiety and depression with COPD. Some studies established differences in the clinical presentation in women and men with diagnosed and underdiagnosed COPD.7 EPI-SCAN found that 55.3% of women with COPD had never smoked; this percentage is even lower than the 75% observed in IBERPOC.33 The IBERPOC results also showed that women with COPD, in addition to lower exposure to tobacco smoke than men, had less impairment of spirometric parameters, fewer symptoms and better quality of life.10
The use and interpretation of spirometry as a tool for defining COPD are different at population compared to individual level. For example, in the population strategy, of all the women in EPI-SCAN with spirometry consistent with COPD, it may be surprising that more than half reported that they had never smoked. At clinical level, a doctor would explore the cause of this airflow limitation (passive smoking, other occupational exposures, comorbidities, etc.) and would start classifying his/her symptoms to diagnose, and if need be, initiate treatment. Unfortunately, it seems that, to date, population-based epidemiological initiatives (or case-finding initiatives in sub-populations at risk) for COPD screening have only provided partial solutions to the still high underdiagnosis of COPD, which continues to be a mainly female problem.34
Recommendations and ActionsThe general perception of physicians of women with respiratory symptoms and suspected COPD must improve, and informative and educational measures on the importance and different characteristics of COPD in women would help to reduce underdiagnosis and its undertreatment.3,31
Monitoring of risk factors and generation of new epidemiological data on COPD and its determinants by sex should be considered a research priority in Spain. In comparison to other chronic diseases, there are few data with respect to the distribution and characteristics of COPD in women. However, in the light of IBERPOC, EPI-SCAN and other studies, we can now say that women are already and will increasingly become the object of medical care for COPD. This implies early diagnostic strategies that are appropriate for women. As with smoking, it seems that women have a higher susceptibility to inhaled industrial pollutants for developing respiratory diseases in general, compared to men. The efficacy of treatments in COPD may be different, especially with respect to smoking cessation and pulmonary rehabilitation. As regards respiratory drugs, there were no differences in efficacy initially,35 although new drugs appear to be less effective in women.36 As has previously been reported, although the clinical presentation of COPD in women may have slight differences, there should be greater emphasis on comorbidities in women, such as osteoporosis, anxiety and depression as accompanying elements.37 The population shift toward chronic illnesses with the triad of aging, comorbidities and polypharmacy38 can already be applied to COPD, along with increased relative feminization.
ConclusionsCOPD is a major health problem in women in Spain, at both population and individual level. Progressive implementation of the recommendations of the National Strategy on COPD and monitoring of its indicators in women should be considered priority issues. Among other aspects, resources should be identified and initiatives established to reduce the high underdiagnosis of COPD in women.
Conflict of InterestThe authors have no conflict of interest to declare.
The sponsor of the EPI-SCAN study is GlaxoSmithKline S.A. The company would like to acknowledge the hard work of all the investigators and collaborators in each center, and to thank the selfless voluntary collaboration of all the participants.
EPI-SCAN scientific committee
Julio Ancochea, Hospital La Princesa (Madrid)
Guadalupe Sánchez, Departamento Médico, GlaxoSmithkline S.A. (Madrid)
Enric Duran-Tauleria, Institut Municipal d’Investigació Mèdica (IMIM) (Barcelona)
Francisco García Río, Hospital La Paz (Madrid)
Marc Miravitlles, Hospital Clínic (Barcelona)
Luis Muñoz, Hospital Reina Sofía (Córdoba)
Vıctor Sobradillo-Peña, Hospital de Cruces (Bilbao)
Joan B Soriano, Fundació Caubet-CIMERA Illes Balears (Mallorca)
EPI-SCAN principal investigators
Julio Ancochea, Hospital La Princesa (Madrid)
Luis Borderías, Hospital San Jorge (Huesca)
Francisco García Río, Hospital La Paz (Madrid)
Jaime Martínez, Hospital Central de Asturias (Oviedo)
Teodoro Montemayor, Hospital Virgen de la Macarena (Sevilla)
Luis Muñoz, Hospital Reina Sofía (Córdoba)
Luis Piñeiro, Hospital Xeral Cies (Vigo)
Joan Serra, Hospital General de Vic (Vic, Barcelona)
Juan José Soler-Cataluña, Hospital General de Requena (Requena, Valencia)
Antoni Torres, Hospital Clínic (Barcelona)
Jose Luis Viejo, Hospital General Yagüe (Burgos)
Please cite this article as: Ancochea J, et al. Infradiagnóstico de la enfermedad pulmonar obstructiva crónica en mujeres: cuantificación del problema, determinantes y propuestas de acción. Arch Bronconeumol. 2013;49:223–9.