We report the case of a 45-year-old woman who consulted due to dyspnea and bronchial hyperreactivity. She had been operated at the age of 3 years for an ostium secundum atrial septal defect.
Transthoracic echocardiography showed dilated right chambers, and transesophageal echocardiography revealed normal left pulmonary venous drainage, while the right pulmonary veins (PV) were not visualized. We requested a chest spiral CT without intravenous contrast (IVC), angio-CT of the PVs, and 3-dimensional reconstructions.
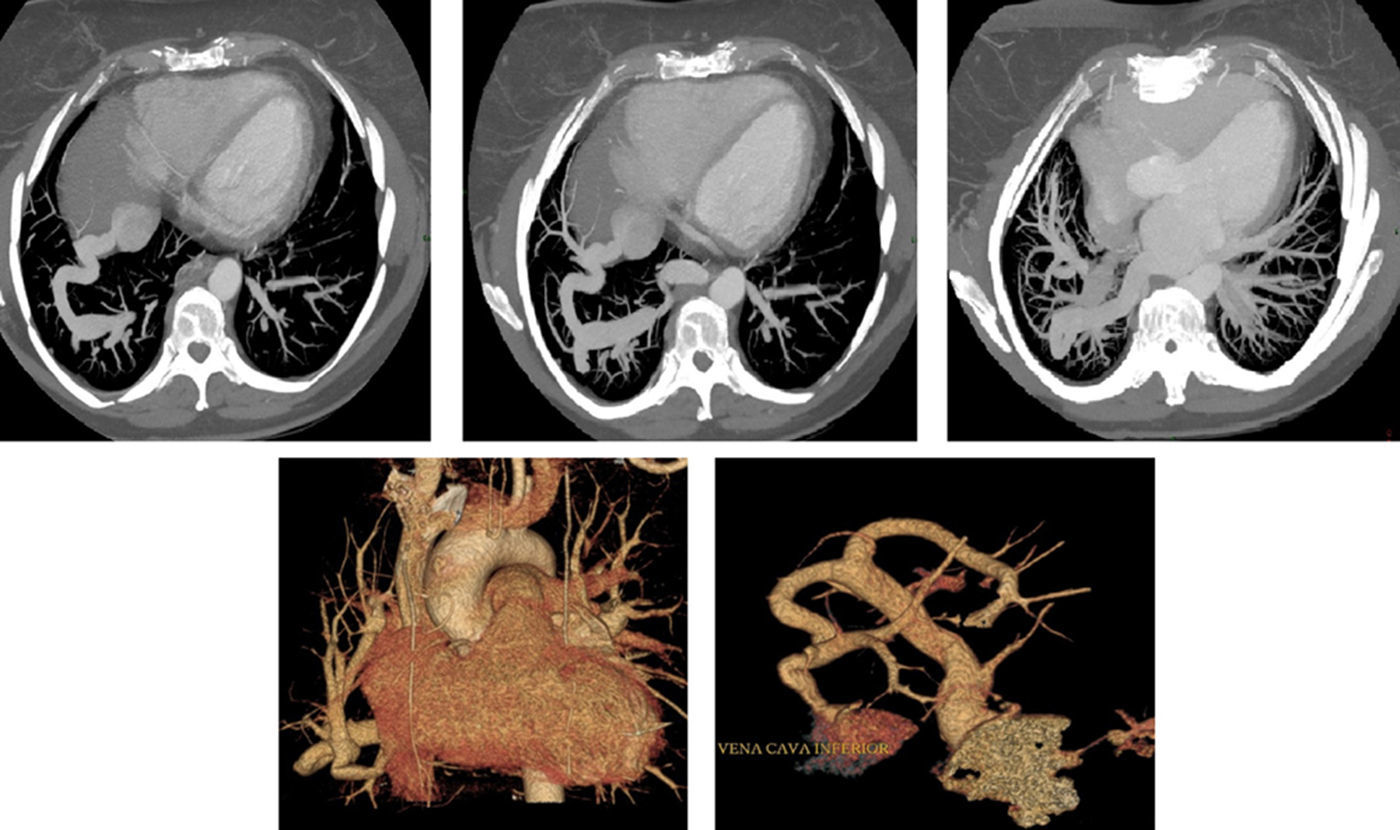
The studies showed anomalous PV venous return into a vessel that communicated with the left atrium (LA) at one end and the inferior vena cava (IVC) at the other. There were no other associated malformations. Findings were compatible with a congenital venolobar syndrome (Fig. 1).
The upper panel shows a series of axial CT slices revealing the double connection of the aberrant vessel to the LA and IVC. The lower left panel shows a 3-D reconstruction of the heart and great vessels with the aberrant vein, and the lower right panel shows a reconstruction of the aberrant vein with its two ends communicating with the IVC and the LA.
An isotope scan was performed, showing increased pulmonary output (Qp/Qs 1.7).
Given the patient's symptoms and the hemodynamic impact, the end of the vessel that was draining to the IVC was occluded percutaneously with the use of an Amplatzer device.
Scimitar syndrome is a set of abnormalities that includes the abnormal connection of the right PVs to the IVC. Its incidence is low and 25% of patients have other associated malformations.1
Our case is unusual because it is a variant of the scimitar syndrome with double drainage to the IVC and LA, which could be treated percutaneously, thus avoiding surgery.
Please cite this article as: Rodríguez-Torres DJ, Segura-Rodríguez D, García-Orta R. Una variante rara del síndrome de la cimitarra. Arch Bronconeumol. 2017;53:639.