A previously healthy 45-year-old male presented to local hospital due to fever, chest tightness and dyspnoea with a temperature of up to 39°C before this admission. Laboratory tests revealed elevated indicators of infection and computed tomography pulmonary angiography (CTPA) showed bilateral lung infection with minimal pleural effusion. Paracetamol was given to the patient, effectively reducing his fever but inadequately addressing his breathing difficulties. Eventually, he was transferred to our hospital.
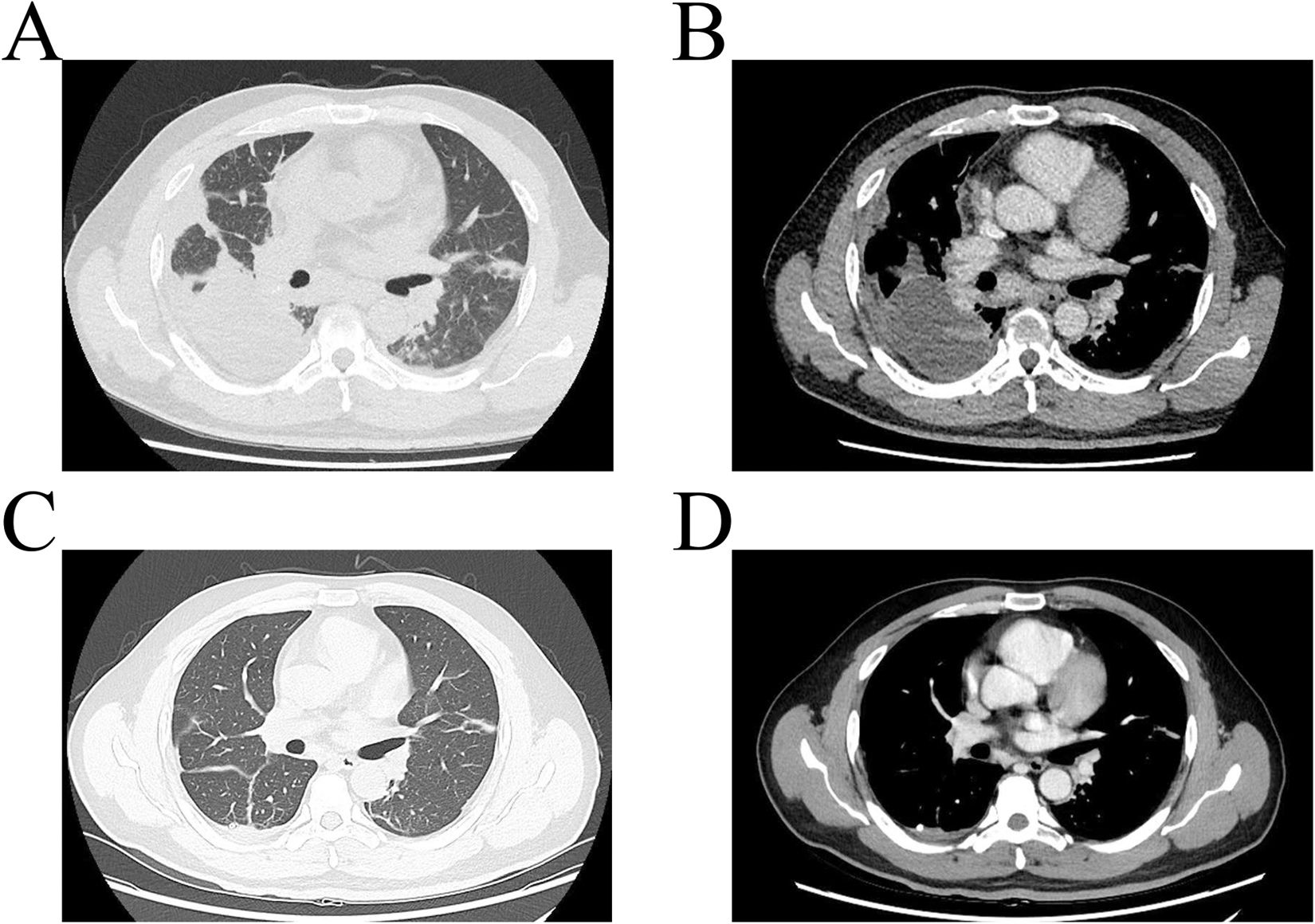
On admission, blood gas analysis revealed a PO2 reading of 107mmHg, a PCO2 measurement of 40mmHg, FiO2 49% and an oxygenation index of 218mmHg. CTPA uncovered bilateral pneumonia characterized by partial consolidation of lung tissue and slight bilateral pleural effusion (Fig. 1A/B). The next generation sequencing detection of alveolar lavage fluid revealed the novel coronavirus mutant named XBL with 12229 sequence numbers. Other pathogen detection of lavage solution including aspergillus and mycobacterium tuberculosis were negative. After receiving treatment with Nematavir/Ritonavir and methylprednisolone, he experienced significant improvement in chest tightness and breathing difficulties. Re-examination indicated a decrease in blood routine infection index, and CT imaging showed dramatically absorption of double pneumonia (Fig. 1C/D). A throat swab tested negative for COVID-19. Therefore, he was discharged on the 10th day of hospitalization.
The patient tested positive for COVID-19 in December 2022, which was the time of the Omicron pandemic in China. During his first contraction of COVID-19, he only experienced transient fever alongside upper respiratory symptoms including cough and sputum as the same as other Omicron infection. The symptoms gradually improved within one day, which are in stark contrast to this admission including chest tightness and hoarseness. Furthermore, he did not exhibit typical Omicron sequelae such as muscle pain and sleep disturbance, which are called “long COVID”.1 The patient received three doses of the Sinovac-CoronaVac vaccine in May, June, and December 2021, which was categorized under WHO Emergency Use Listing Qualified Vaccines.2 Vaccine is effective in preventing Omicron infection including XBB, and easing associated symptoms.3 The patient's symptoms improved quickly when he first contraction of COVID-19, which may indicate that vaccine protected him to some extent. While antibodies produced by the patient's first COVID-19 positive four months ago neither prevent the second infection, nor shorten the course or reduce the severity of it.
The common CT manifestation of COVID-19 includes multiple segmental ground glass opacities distributed dominantly in extrapulmonary zones and along bronchovascular bundles.4,5 In contrast to other variants such as XBB and Delta, initial CTPA at the onset of XBL showed multiple solid parenchyma and nodular densification, with minimal effusion in bilateral pleural cavities. After five days of antiviral treatment, a subsequent CTPA indicated a significant absorption in both lung consolidation and pleural effusion. These findings suggest that XBL may present with solid and pleural fluid manifestations similar to those observed in bacterial pneumonia, although further cases are required to confirm this association.
As no cases of XBL have been reported, we present a case report of this variant with uncommon imaging presentations to improve scientific understanding of its pathogenicity and clinical implications.
FundingThis work was supported by the Natural Science Foundation of Guangdong Province (2021A1515010480 to Y.B. Zhou).
Conflicts of InterestNone declared.