A great number of high-quality original articles addressing SARS-CoV-2 infection were published during the pandemic, yet we still have much to learn about its pathophysiology. To glean more information, we must turn to multidisciplinary evidence to analyze a disease in which clinical observation takes precedence over the usual diagnostic imaging studies that, in most cases, have proved insufficient for the study of a disease that targets small vessel. We have dropped the term COVID-19 pneumonia, now that we can assume that we are dealing with a multisystemic disease. For many months, we became embroiled in the notions of a thromboinflammatory state and hypercoagulability but, finally, the concept of endothelial damage has prevailed. In this article, we will focus on the lung, the area that has been studied in greatest depth in COVID-19. In an attempt to answer at least some of the many outstanding questions, we will interpret pulmonary events in SARS-CoV-2 infection from the perspective of both the enduring concepts of coagulopathy and vascular plexus, and emerging ideas on vascular tone dysregulation.
The lungThe presence of microthrombi in small-caliber arteries (<1mm) is a common finding that has been observed in up to 86% of pulmonary necropsies.1 The mechanism of microthrombi formation is associated with COVID-related endothelial disease, and is the result of the direct infection of endothelial cells by SARS-CoV-2, which predisposes the host to thrombosis and alters vascular tone, redox balance, and acute and chronic inflammatory reactions affecting the vascular wall.2 Severe respiratory failure occurs in <5% of COVID-19 patients, in whom multiple pathogenic mechanisms (V/Q mismatch, diffusion changes, shunt effect, and increased dead space) frequently coexist, complicating therapeutic management and casting a shadow on prognosis. Brain stem and respiratory center changes associated with SARS-CoV-2 pathophysiology have been described,3 and may also be responsible for the discrepancy between the sensation of dyspnea and work of breathing so frequently observed in our patients.
Coagulopathy, vascular plexus, and the alveolocapillary membraneSARS-CoV-2 coagulopathy is characterized by very high D-dimer levels and no marked changes in other hemostasis parameters, and is associated with various thrombotic complications and disease severity.4 The overall incidence of pulmonary embolism in these patients is currently estimated to be 17%, but this rate is higher in more severe patients, in whom microthrombosis appears to be related to the severity of symptoms.5
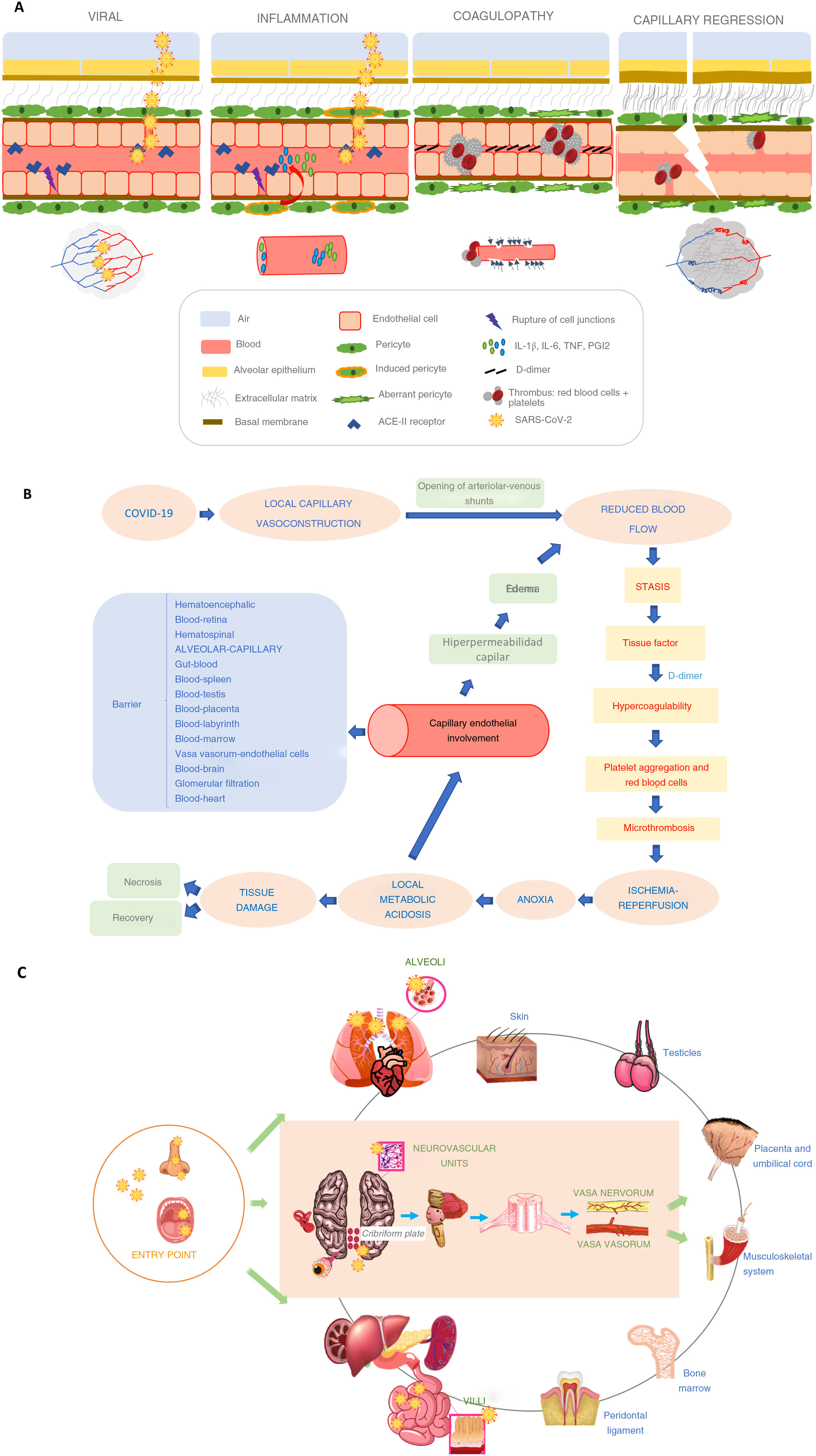
The endothelial cells are responsible for maintaining barrier function and vascular integrity, while preventing inflammation by limiting its interaction with immune cells and platelets. Pericytes are cells derived from mesenchymal stem cells that, together with the endothelial cells, create the functional vascular plexus of the capillaries.2 Pericytes are responsible for long-lasting capillary constriction in ischemia-reperfusion processes, and their dysfunction causes capillary regression. In patients with “diabesity” (obesity and type 2 diabetes), increased oxidative stress with elevated intracellular levels of reactive oxygen species (ROS) promotes the production of proinflammatory cytokines (IL-1β, IL-6, and TNF) and PGI2. This, in turn, induces endothelial cell apoptosis6 and reduces the ischemic preconditioning that normally would help cope with the infection. Some authors have argued that endothelial dysfunction is the result of direct infection by the virus: SARS-CoV-2 binds to the angiotensin-converting enzyme (ACE)-II receptor, which is expressed in large amounts in endothelial cells and pneumocytes. This has the effect of reducing ACE-II receptor activity, preventing angiotensin II inactivation and conversion to angiotensin I. Increased angiotensin II stimulates vascular constriction, and decreased angiotensin I suppresses nitric oxide production, which increases leukocyte and platelet adhesion7 (Fig. 1A). SARS-CoV-2 infection also activates tissue factor expression, not only in the endothelial cells, but also on the surface of macrophages and monocytes, thus initiating the coagulation cascade. All these factors cause vasoconstriction, platelet aggregation, and microthrombosis (Fig. 1B), as demonstrated in recent post-mortem studies, where capillary vascular damage with abundant microthrombi was observed,8 especially in patients with severe disease. Pericytes share a basal membrane with endothelial cells in the distal pulmonary capillaries, where gas exchange is performed. The breakdown of the dialog between pericytes and endothelial cells interrupts alveolocapillary homeostasis, resulting in a proinflammatory and procoagulant state that leads to the loss of pericytes, resulting in an immature vascular network that will lead to air leaks in the alveoli and thrombus formation in the capillaries6,9,10 (Fig. 1 A). These factors, along with vasculitis, are responsible for severe acute respiratory syndrome, while patients with diabesity have a greater predisposition to severe complications. Pulmonary angiography with multidetector computed tomography and iodine mapping in these patients reveals coexisting areas of inflammatory pneumonia, hypoperfusion, and thrombosis of the distal vessels that are difficult to detect with other diagnostic tools.11 Microthrombi have been found not only in the lungs, but also in the heart, kidneys, and liver of COVID-19 patients,12 confirming the presence of generalized thrombotic microangiopathy in these patients, and reminding us that endothelial dysfunction is an important precursor to subsequent cardiovascular events.
Vascular tone dysregulationAlonso et al. were the first to describe multisystemic Raynaud's phenomenon, including pulmonary Raynaud's, in COVID-19 patients.13 Natatello et al. subsequently described capillaroscopic changes in patients with COVID-19.14 These vascular tone findings suggest that pulse oximetry measurements could be incorrect, leading to poor management of hospitalized patients consisting in over-administration of oxygen to poorly perfused areas and doubts as to whether this procedure might help or further damage patients’ alveoli. It is clear that the vessel diameter of the microvascular bed makes it more sensitive to Raynaud's phenomenon. The number of studies of potent vasodilator agents in COVID-19 associated with standard corticosteroid and anticoagulation therapy is increasing, and ongoing clinical trials are investigating the administration of PDE5 inhibitors to dysmetabolic patients.15
Pericyte dysfunction causes capillary regression that is clearly associated with diseases such as diabetes mellitus, ischemia/infarction, hypertension, heart failure, neurodegenerative diseases, infectious diseases (e.g. sepsis), and cancer.10 COVID-19 could undoubtedly be added to this long list. However, vascular tone regulation is complex, because it involves not only mediators derived from the endothelium, but also central and peripheral neurogenic mechanisms, including those occurring in the alveolocapillary barrier and other systemic barriers (Fig. 1C). While some of these proposals may still be rough around the edges, we believe they continue to drive discussions that will further advance our understanding of this disease. The nature of capillary dysfunction in COVID-19 is still not well understood, and more translational research studies are needed to shed light on the matter.