As a result of the COVID-19 pandemic declared by the WHO in March 2020, the vast majority of Spanish hospitals have had to adapt to the new scenario by modifying their infrastructure and organization and by designing strategies for collaboration and coordination among the different specialties.1
In terms of care and logistics, the treatment of patients with COVID-19 pneumonia who develop severe respiratory failure has been one of the most important challenges faced by healthcare providers in general and by respiratory medicine experts in particular. These demands have led to the creation of physical spaces called intermediate respiratory care units (IRCU), where non-invasive respiratory support (NIRS) can be administered with proper surveillance and monitoring.2–4 Staff in the TRS-VM-CRC area conducted an exploratory survey of all hospitals in Spain with an IRCU for the purpose of analyzing the role of respiratory medicine departments during the COVID-19 pandemic, the growth of IRCUs, the burden of care involved, and the clinical outcomes. The questionnaire consists of 34 questions on the status of IRCUs before and during the COVID-19 pandemic (Annex 1). Data were collected by an external agency (Ipsos: ISIN code FR0000073298, Reuters ISOS.PA, Bloomberg IPS:F) by telephone or online between June and September 2020.
A total of 67 hospitals were included, generating an overall registry of about 40,000 patients seen up to the date of the study. Twenty-eight (42%) of the hospitals contacted already had an IRCU and 11 (16%) created one because of the pandemic.
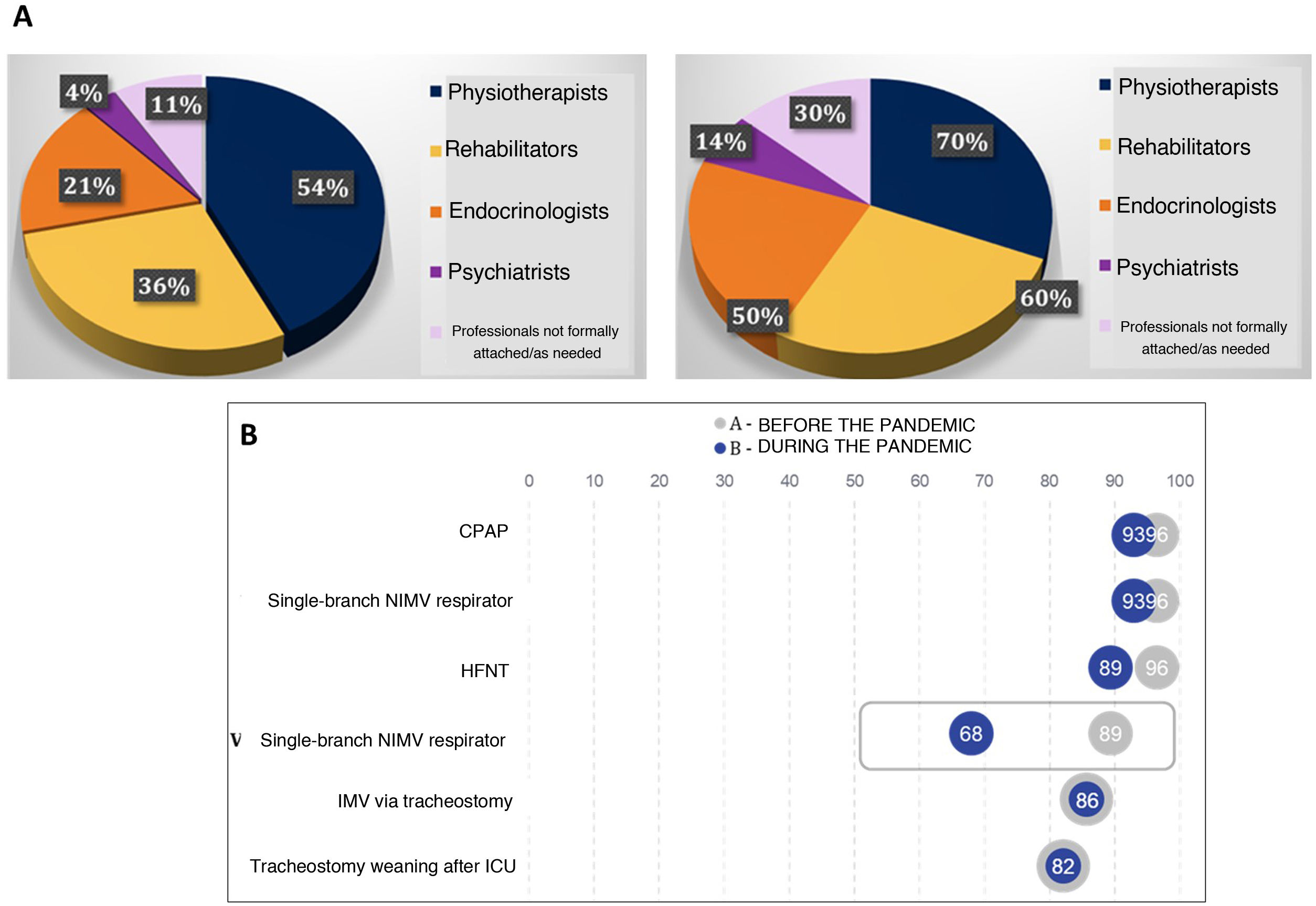
Prior to the COVID-19 pandemic, the average number of beds per IRCU was 4.07, with a nurse/patient ratio of 1:5. A total of 86% of the units had an appointed specialist physician, and the shift duration was generally 8hours (50%). Only 33% of the respiratory medicine specialists worked 12- or 24-h in-person shifts. Other specialists working in the IRCUs and the therapies used are described in Fig. 1.
Seventy percent of the 28 IRCUs existing before the pandemic have been expanded. New units have also been created and pre-existing facilities have been enlarged. There were more IRCU units managed by the respiratory medicine department in hospitals that had an IRCU before COVID-19 compared to those that had no IRCU before the pandemic (75 vs. 36, p<0.05).
IRCU equipment available during the pandemic (monitoring, capnography, flexible bronchoscopy, and blood gas analyzers) has not changed significantly. The mean number of IRCU beds has increased, and more beds are available in facilities that existed before the pandemic than in those created de novo (14.82 vs. 7.91, p<0.05).
During this period, the nurse-patient ratio improved from 1:5 to 1:4 (p<0.05) compared to the pre-pandemic situation, and although the number of clinicians working shifts longer than 12h (74%) increased, the proportion of units with a respiratory medicine specialist did not change. Other professionals attached to the unit and the therapies used are described in Fig. 1.
More specific facilities for the care of COVID-19 patients requiring NIRS were needed in regions with a high cumulative incidence (CI) (>300) compared with regions with a low/moderate CI (94.4 vs. 67, p<0.05). In addition, more respiratory medicine experts were attached to IRCUs in areas with a high CI (100% vs. 76%, p<0.05).
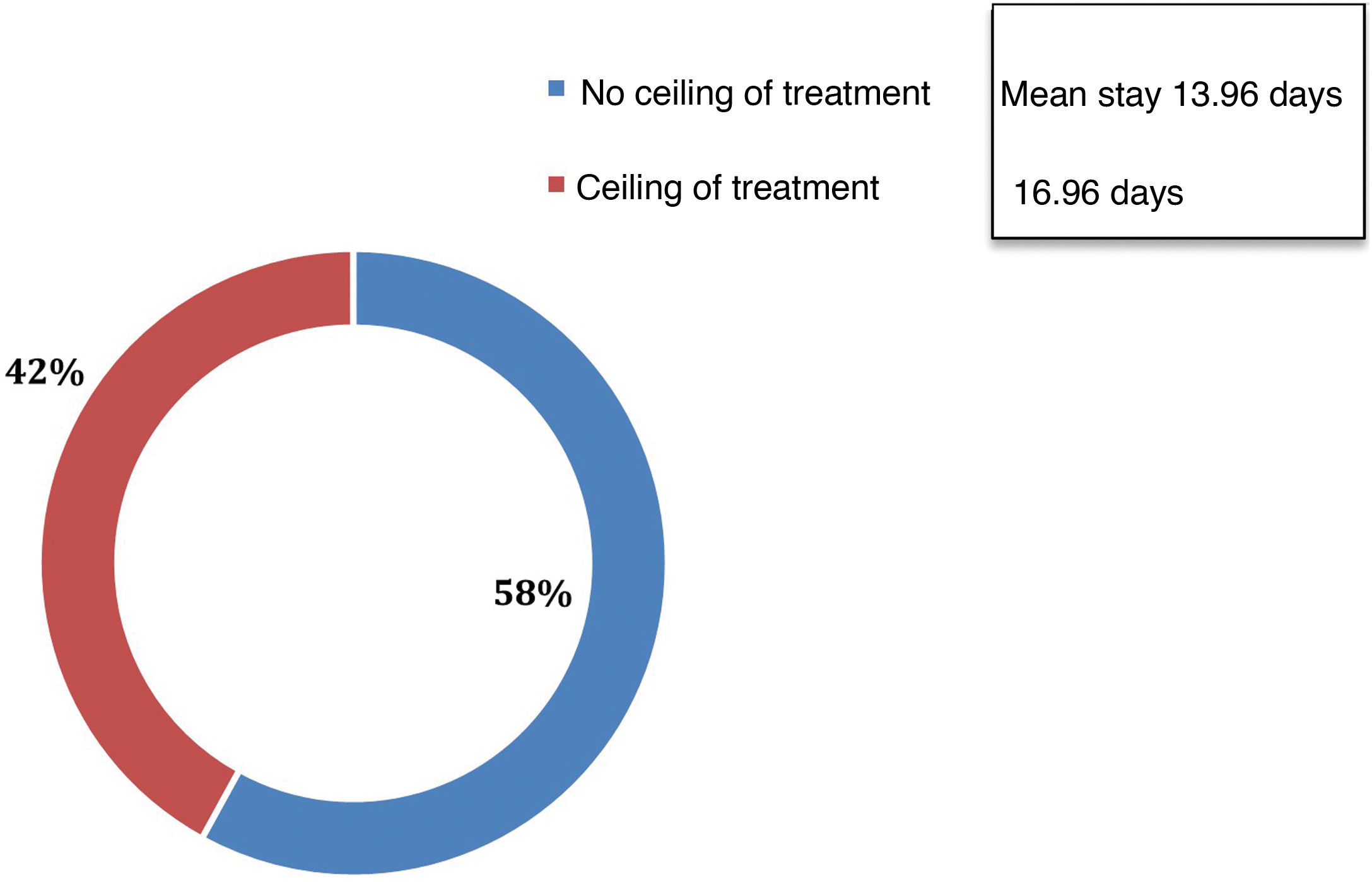
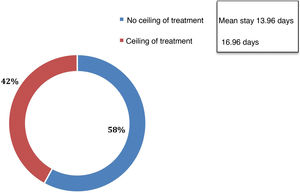
With regard to the epidemiological context of IRCUs during the pandemic, the mean number of infections per health area was 2953.31 and the mean number of admissions was 1316.20, representing 36% of all infections. A mean of 338 (28.5%) patients admitted were evaluated in a respiratory medicine department. Of the patients assessed by a pulmonologist, 71% were admitted to an IRCU. Overall, 2.8% of all infections, 10% of total admissions, and 56.3% of patients assessed by respiratory medicine were admitted to an ICU. The profile of patients assessed by respiratory medicine and mean hospital stays are described in Fig. 2.
The number of hospital admissions in each autonomous community was associated with a higher CI (r=0.57, p=0.001). In addition, the more admissions made, the greater the tendency to use NIRS (r=0.3, p=0.08), the more patients ventilated via tracheostomy (r=0.4, p=0.02), and the more weaning processes performed (r=0.4, p=0.03). The higher the number of hospital admissions, the higher the number of patients assessed by respiratory medicine experts (r=0.6, p=0.00).
The higher the CI in the autonomous community, the higher the number of monitored beds available in hospitals during the first wave (r=0.37, p=0.02).
Regarding treatment with NIRS in patients with a ceiling of treatment, a positive correlation has been found between treatment with high-flow oxygen therapy (r=0.72; p=0.04) and NIMV (r=0.7; p=0.00) and the number of hospital discharges home, showing that the more use made of these therapies, the greater the number of discharges home. The presence of a respiratory medicine expert in the IRCU has been associated with fewer weaning procedures in the ICU (r=−0.3, p=0.02) and a shorter hospital stay for patients with no ceiling of treatment (r=−0.3, p=0.008).
The results of this study show that in the past decade in Spain, and particularly now during the COVID-19 pandemic, there has been an exponential increase in the creation of units that previously were chronically understaffed despite their clear advantages.5–11
Our results also highlight the capacity of respiratory medicine departments, which bore much of the burden of care for severely ill patients, to adapt and respond to the unprecedented situation created by the COVID-19 pandemic. They have reorganized and restructured by creating new IRCUs or expanding existing units while maintaining the quality of the facilities and the respiratory therapies provided, and thus achieved good clinical outcomes, in terms of hospital stays, ICU admissions, and mortality.
Given the recent upheaval in the healthcare system and the future outlook, there is a clear need to consolidate and plan the management of the IRCUs already created, and to develop an IRCU network throughout Spain that can alleviate the demand for ICU beds and ensure appropriate care for patients with a ceiling of treatment.
In conclusion, IRCUs have been useful in the management of patients with COVID-19 and severe respiratory failure by administering NIRS and thus avoiding admission to the ICU of nearly half of our severe patients. The presence of these essential units has clearly grown throughout Spain as a result of the SARS-CoV-2 pandemic.
FundingThis study was conducted thanks to Philips’ funding of Ipsos.
Conflict of interestsNone.