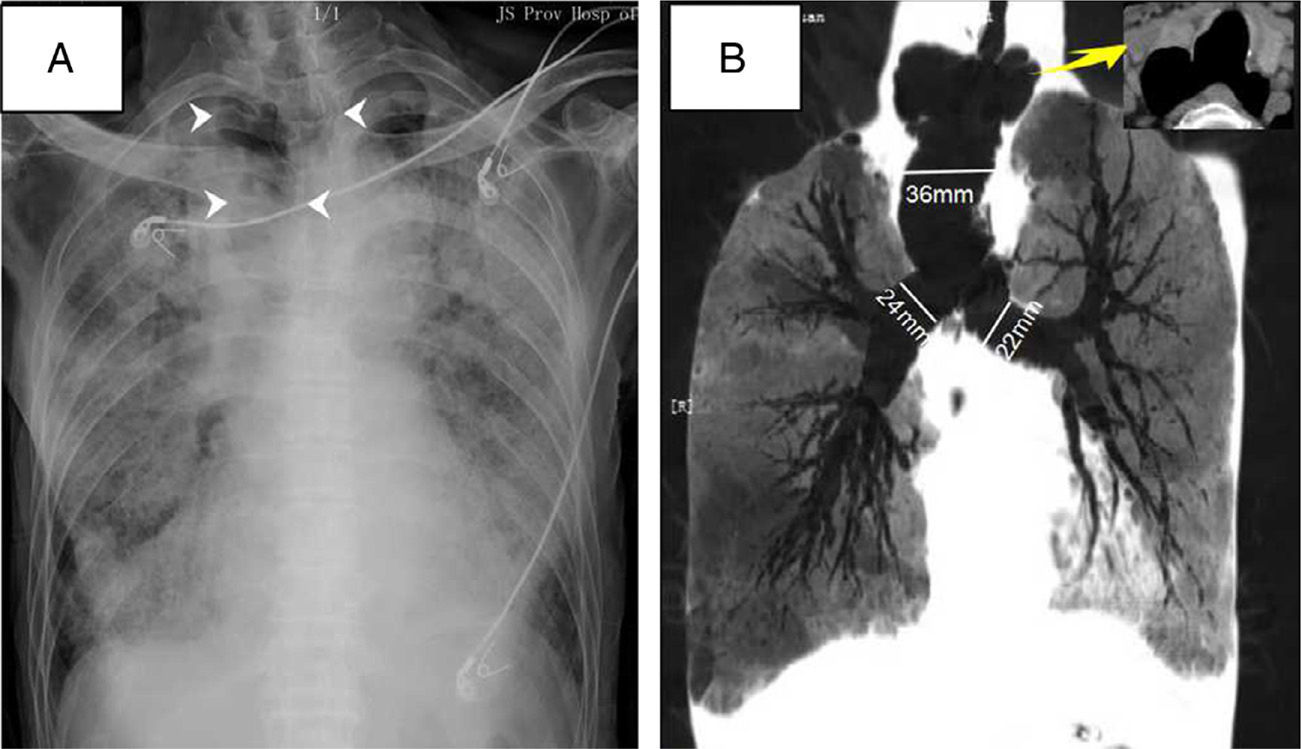
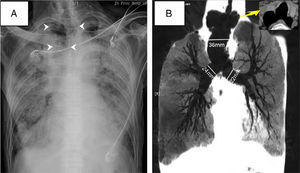
A 79-year-old man with a history of pulmonary fibrosis and Sjogren's syndrome was admitted to ICU for management of severe ARDS (Acute Respiratory Distress Syndrome) after radical prostatectomy. He presented with respiratory distress with bilateral opacities in chest radiograph (Fig. 1A). Tracheal intubation was performed the next day. However, the tidal volume continued to be instable at about 50•200ml even under fully sedation. A serious gas leakage was found as breath flow could be heard, which became better when head position fixed to the left. Taking back his history, he had had untreated tracheal abnormalities for decades. Chest computed tomography later showed diverticulum on both sides at the upper part of the trachea, and marked dilated trachea at the lower portion (Fig. 1B). Dueing to the poor attachment between the cuff of the endotracheal tube and the trachea wall, recruitment maneuvers for ARDS did not go well. The patient's condition continued to deteriorate and eventually died on the 11th day at ICU. Tracheobronchomegaly is a rare disease characterized by abnormally enlarged tracheo-bronchial tree. Chest X-ray may be misleading as it is easily overlooked on radiograph (Fig. 1A). Inexplicable poor ventilation in intubated patients should take into account the possibility of anatomic abnormalities, such as tracheobronchomegaly.
The Impact Factor measures the average number of citations received in a particular year by papers published in the journal during the two preceding years.
© Clarivate Analytics, Journal Citation Reports 2025
SRJ is a prestige metric based on the idea that not all citations are the same. SJR uses a similar algorithm as the Google page rank; it provides a quantitative and qualitative measure of the journal's impact.
See moreSNIP measures contextual citation impact by wighting citations based on the total number of citations in a subject field.
See more