Amyloid deposition in tracheobronchial tree is a rare presentation and counts about 1% of benign tumors in this area. Herein, we describe a case of primary tracheobronchial amyloidosis which obstructed almost completely the distal trachea and the main left bronchus.
The mass was successfully resected by mechanical resection and Nd-YAG laser coagulation during rigid bronchoscopy. Afterwards, a self-expanding Y-stent of new generation was inserted to restore airway patency. Five months later, radiological and bronchoscopic findings showed the stent in site, with normal patency of the tracheo-bronchial tree.
El depósito de amiloide en el árbol traqueobronquial es una forma de presentación muy poco frecuente y supone alrededor del 1% de los tumores benignos de esta zona. Describimos aquí un caso de amiloidosis traqueobronquial primaria que obstruía casi por completo la parte distal de la tráquea y el bronquio principal izquierdo.
Se realizó con éxito la extirpación de la masa mediante resección mecánica y coagulación con láser Nd-YAG utilizando una broncoscopia rígida. Posteriormente, se implantó una prótesis en Y autoexpansible de nueva generación, para restablecer la permeabilidad de la vía aérea. Cinco meses después, los exámenes radiológico y broncoscópico mostraron la presencia de la prótesis en el lugar adecuado, con una permeabilidad normal del árbol traqueobronquial.
- •
Amyloid deposition with almost complete occlusion of the tracheobronchial tree is very rare.
- •
Its treatment with endoscopic resection, radiotherapy or laser photoresection has been described.
- •
Endoscopic mechanical resection with Nd-YAG laser coagulation and stent implantation may be an appropriate intervention.
- •
The stent preserves airway patency and prevents the recurrence of amyloid deposition.
Amyloidosis is characterized by the extracellular deposition of insoluble fibril proteins in organs and tissues. Amyloid deposition in the tracheobronchial tree is a very rare form of presentation and accounts for around 1% of benign tumors in this area.1 We describe a case of localized tracheobronchial amyloidosis that was successfully treated by mechanical resection and laser coagulation using a rigid bronchoscope; a covered self-expanding metal Y-stent was then implanted.
Clinical CaseA 67-year-old woman, non-smoker, was admitted to our hospital for cough, shortness of breath and hemoptysis. The patient had noticed the symptoms over the previous seven months. The dyspnea had progressed to the point that she could only walk one block without stopping. During this time, she had a productive cough (the cough was not previously accompanied by sputum production) associated occasionally with small streaks of blood in the sputum. However, the hemoptysis was not massive.
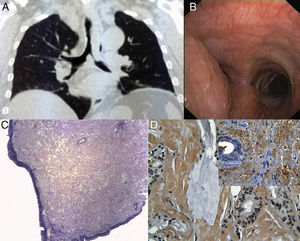
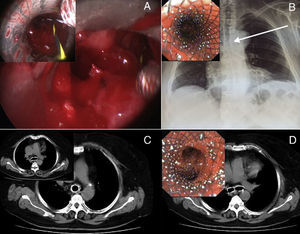
The patient did not report any pathological history of interest. Laboratory and blood tests were within normal limits. On examination, stridor and a reduction in the expansion of the left hemithorax were observed. The chest X-ray was normal, but the computed tomography (CT) scan revealed severe tracheobronchial stenosis (Fig. 1A). Endoscopic examination showed a mass obstructing 80% of the distal trachea and almost all of the left main bronchus. The mucosa was red and fragile (Fig. 1B). The mass mimicked a neoplastic lesion, but the biopsy samples were diagnostic of amyloidosis. Hematoxylin and eosin staining showed the presence of an amorphous material within the normal epithelium (Fig. 1C), which was selectively stained with Congo red (Fig. 1D). The primary objective was considered to be the re-establishment of airway patency. The patient underwent rigid bronchoscopy under conscious sedation, in addition to topical anesthesia with lidocaine. The mass was completely removed by mechanical resection and Nd-YAG laser coagulation (Fig. 1A); a new generation covered self-expanding Y-stent (Micro-tech© (Nanjing) Co., Ltd., Shanghai, China) was then inserted. Correct placement was ensured by inserting a guidewire into each main bronchus (inset, Fig. 2A). The procedure was well tolerated and the respiratory symptoms disappeared rapidly. Radiological (Fig. 2) and endoscopic examinations (inset, Fig. 2) confirmed complete expansion of the device.
The chest CT scan shows a mass with stenosis of the distal part of the trachea (5cm long) and left main bronchus (Part A). Endoscopic visualization shows a mass protruding from the lateral wall of the distal trachea, causing considerable occlusion of the trachea and orifice of the left main bronchus (Part B). The tracheal mucosa is thickened due to the presence of an amorphous substance, despite being covered by normal epithelium (hematoxylin and eosin stain, magnification ×40, Part C). The amorphous substance is selectively stained with Congo red (magnification ×400; Part D). Inset: detection of amyloid P using immunohistochemical methods (magnification ×400).
After complete resection of the mass (Part A), placement of the Y-stent was ensured by inserting a guidewire into each main bronchus (inset, Part A). The observations made on the chest X-ray (white arrow; Part B) and endoscopy (inset, Part B) confirmed complete expansion of the device. Five months later, the CT scan (Parts C and D) and bronchoscopy (inset, Part D) showed normal patency of the tracheobronchial tree, with no recurrence of amyloid deposition.
The type of AL (primary) amyloidosis was then investigated by identification of monoclonal light chains using serum and/or urine immunofixation electrophoresis (IFE). A bone marrow core biopsy was also obtained to identify the underlying plasma cell dyscrasia and to exclude plasma cell myeloma.2 IFE results failed to establish the presence of a monoclonal gammopathy, and the bone marrow biopsy did not reveal amyloid deposition. Consequently, more aggressive treatment using high-dose mephalan and autologous stem cell transplantation was not indicated.3 Physiotherapy, inhalation treatment and mucolytic medication were applied to ease expectoration and prevent clogging of the tracheal bifurcation stent.
Five months later, the patient had progressed well; the CT scan (Fig. 2C and D) and bronchoscopic examination (inset, Fig. 2D) showed normal patency of the tracheobronchial tree, with no recurrence of amyloid deposition.
DiscussionRespiratory amyloidosis can manifest in the form of diffuse parenchymal lung disease (the sub-group with worst prognosis), a nodule in the parenchyma (which is often a casual finding) or tracheobronchial (laryngeal) amyloidosis, which may progress and lead to airway obstruction.1 The case presented corresponds to this third subgroup. Mass reduction surgery may alleviate airway obstruction caused by amyloid deposits, but does not prevent recurrences. After resection of an isolated mass, recurrences are very rare. Other treatments such as pneumonectomy, radiotherapy and laser photoresection have also been described.4
The initial acute form of presentation in this case is unusual. The amyloidosis manifested as an isolated mass, which clearly suggested malignant disease, causing almost complete occlusion of the distal part of the trachea and left main bronchus. The lesion in the central airways was not suitable for surgical treatment; endobronchial resection was the only treatment that allowed airway patency to be re-established. However, these lesions often recur within 12 months after resection, and there is a high risk of perforation or cicatricial tracheobronchial stenosis. Hemorrhage may occur during surgery, and fatal cases have been reported.5 Consequently, we performed resection of the mass using Nd-YAG laser; after complete recanalization of the airways, we implanted a covered self-expanding metal Y-stent. Although no articles have been published describing the use of stents after amyloid resection, we believe that their use could be advantageous for preserving airway patency and preventing the recurrence of amyloid deposition.
We opted for a self-expanding stent instead of a silicone one, due to the greater cross-sectional airway diameter owing to the thinner wall, and the better conformation to irregular airways as a result of the self-expanding force. Furthermore, this stent imitates a normal trachea, and has better clearance of secretions.6
The size of the stent (length and diameter) was established by previous endoscopic examination and three-dimensional chest CT scan. The use of a covered stent was preferred to prevent the growth of amyloid through the mesh. Moreover, covered stents can be effectively and safely removed, without any major complications, if necessary.7
The IFE results failed to establish the presence of a monoclonal gammopathy and the bone marrow biopsy did not reveal amyloid deposition. Consequently, more aggressive treatment using high-dose mephalan and autologous stem cell transplantation was not indicated in this case.2 Physiotherapy, and inhaled and mucolytic medication were used to prevent clogging of the stent.8
In conclusion, our experience shows that amyloidosis can be a rare form of presentation of tracheobronchial obstruction that imitates bronchogenic carcinoma; endoscopic resection with laser and stent implantation may be an appropriate treatment.
Please cite this article as: Fiorelli A, et al. Amiloidosis traqueobronquial tratada con resección con láser endobronquial y prótesis en Y autoexpansible. Arch Bronconeumol. 2013;49:303–5.