Tracheal tumors are extremely rare, representing less than 0.2% of all neoplasms of the respiratory system,1 with only a few case reports of patients with leiomyosarcomas of the tracheal wall.2 Leiomyosarcomas are malignant tumors showing smooth muscle differentiation. They are rarely found in the trachea, with approximately only two dozen cases reported in the literature since 1950.
We report the case of a patient who presented with acute upper airway obstruction secondary to a tracheal leiomyosarcoma and the following use of rigid bronchoscopy to regain upper airway patency.
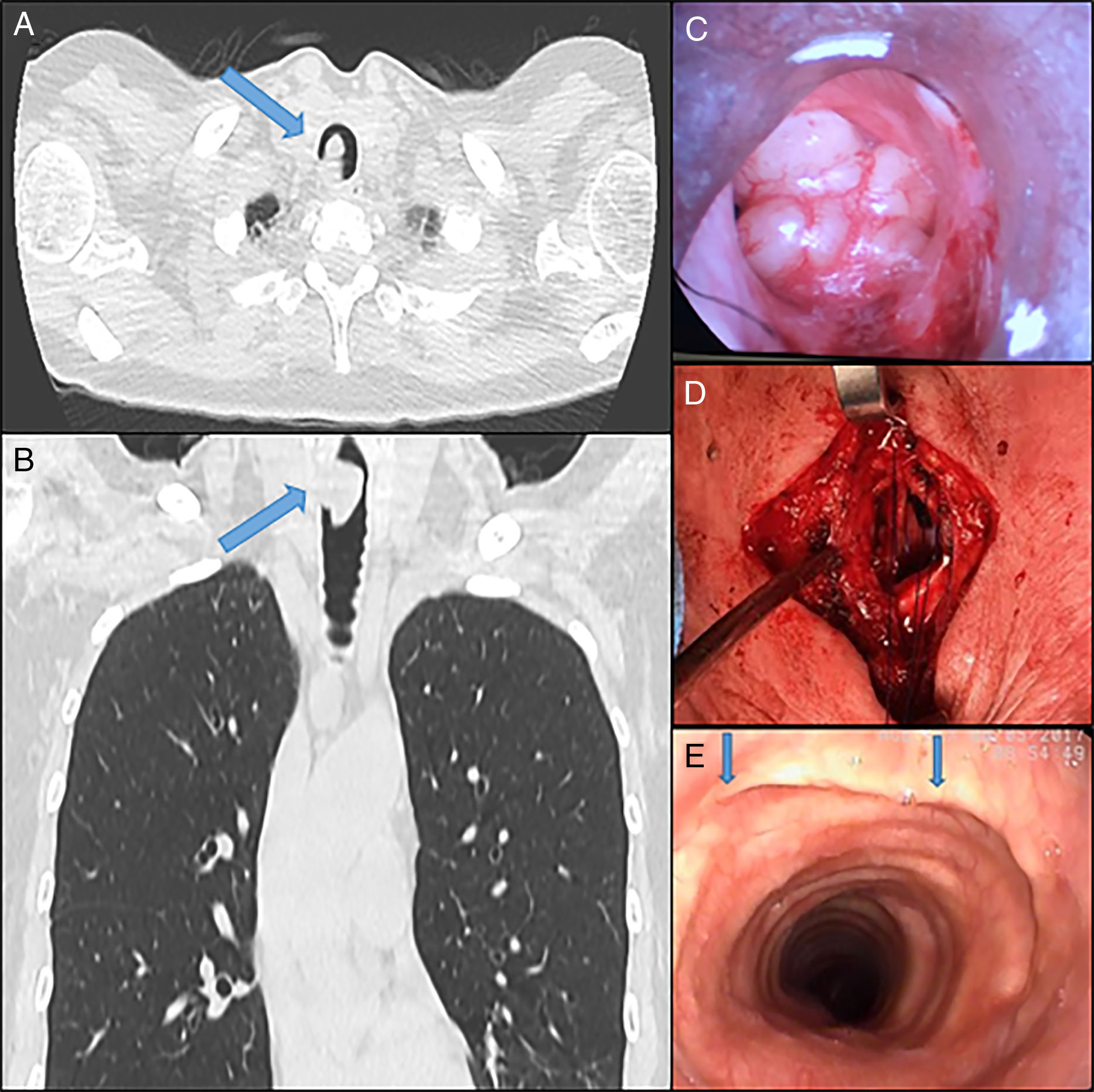
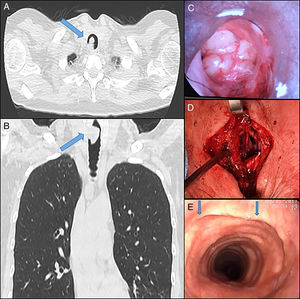
A 52-year-old patient had been undergoing chronic bronchodilator treatment due to a supposed diagnosis of asthma at another medical institution, who consulted at the emergency department referring severe dyspnea and worsening of her usual stridor. A multislice computed tomography (MSCT) showed a tracheal lesion located 3cm below the vocal cords that compromised 85% of the tracheal lumen (Fig. 1A and B). In view of critical central airway obstruction and impending respiratory failure, urgent rigid bronchoscopy and excision of the tracheal growth were performed (Fig. 1C). The anatomopathological report of the endoscopically resected lesion informed tracheal leiomyosarcoma. Eventually the patient was discharged and then scheduled to be readmitted to perform a tracheal resection and end-to-end anastomosis (Fig. 1D). The final procedure consisted of the resection of two tracheal rings and primary end-to-end anastomosis. The patient was discharged 5 days after the surgery without any complications. The definitive anatomopathological exam confirmed the nature of the lesion, with surgical margins free of lesion. Three months after the surgery, a flexible bronchoscopy was performed which evidenced absence of relapses with an anastomosis of normal caliber (Fig. 1E, blue arrows).
Primary tracheal tumors are rare. Population-based studies from tumor registries in Finland, Denmark, Netherlands, and England report annual incidence rates of tracheal cancer of approximately 0.1 per 100,000 per year, with tracheal cancers accounting for less than one-half of 1 percent of all malignant tumors.3,4 Histologically, most of them are squamous cell or adenoid cystic carcinomas.5 In most patients, tracheal tumors are symptomatic, but often misdiagnosed as asthma, chronic pulmonary disorder or tumors of the thyroid or lungs.4 According to Napieralska et al. clinical symptoms occur in 95% of patients. The most common symptom is dyspnea (72.4%), cough (53.4%), haemoptysis (32.8%), and hoarseness (27.6%). Other symptoms include weight loss (22.4%), pain (15.5%), dysphagia (12.1%), weakness (10.3%), stridor (5.2%), fever (8.6%), the feeling of having an obstacle in trachea (10.4%), and neck tumor (6.9%).6
Concerning the initial therapeutic approach of these patients, rigid bronchoscopy is an essential tool not only for treating the initial upper airway obstruction prior to oncologic resection, but also for the evaluation and planning of the tracheal limits of the subsequent surgery.7,8 Rigid bronchoscopic excision not only permits better control of the airway and simultaneous ventilation but also ensures a better hemostasis and large diameter instruments to be passed through it for endoscopic procedures.9 It has also been shown that rigid bronchoscopic intervention in patients with respiratory failure caused by malignant central airway obstruction leads to improved survival by allowing additional definitive therapeutic modalities.10 Relief of central airway obstruction can be achieved rapidly by means of both flexible and rigid bronchoscopy assisted by laser, electrocautery, argon plasma coagulation, or cryotherapy. However, in those with significant hypoxemia and critical airway obstruction, rigid bronchoscopy is the quickest method in relieving the airway obstruction. If flexible bronchoscope is being used, it should ideally be introduced through the barrel of rigid bronchoscope.11,12
Finally, although there is no sufficient evidence on the ideal therapeutic management of tracheal leiomyosarcoma, there is consensus that tracheal resection with appropriate oncological margins in patients with different tracheal tumors is the best surgical strategy since it provides the greatest benefit in terms of overall survival. Moreover, several authors agree that the optimal therapy consists of surgical resection followed by radiotherapy. However, while adjuvant radiotherapy is an important part of the treatment of patients with tracheal cancer, the role of chemotherapy requires further investigation.7,13
Further and more extensive studies are needed to clarify the particular behavior of tracheal leiomyosarcoma in regards to adjuvant or primary radiotherapy and it potential benefits.