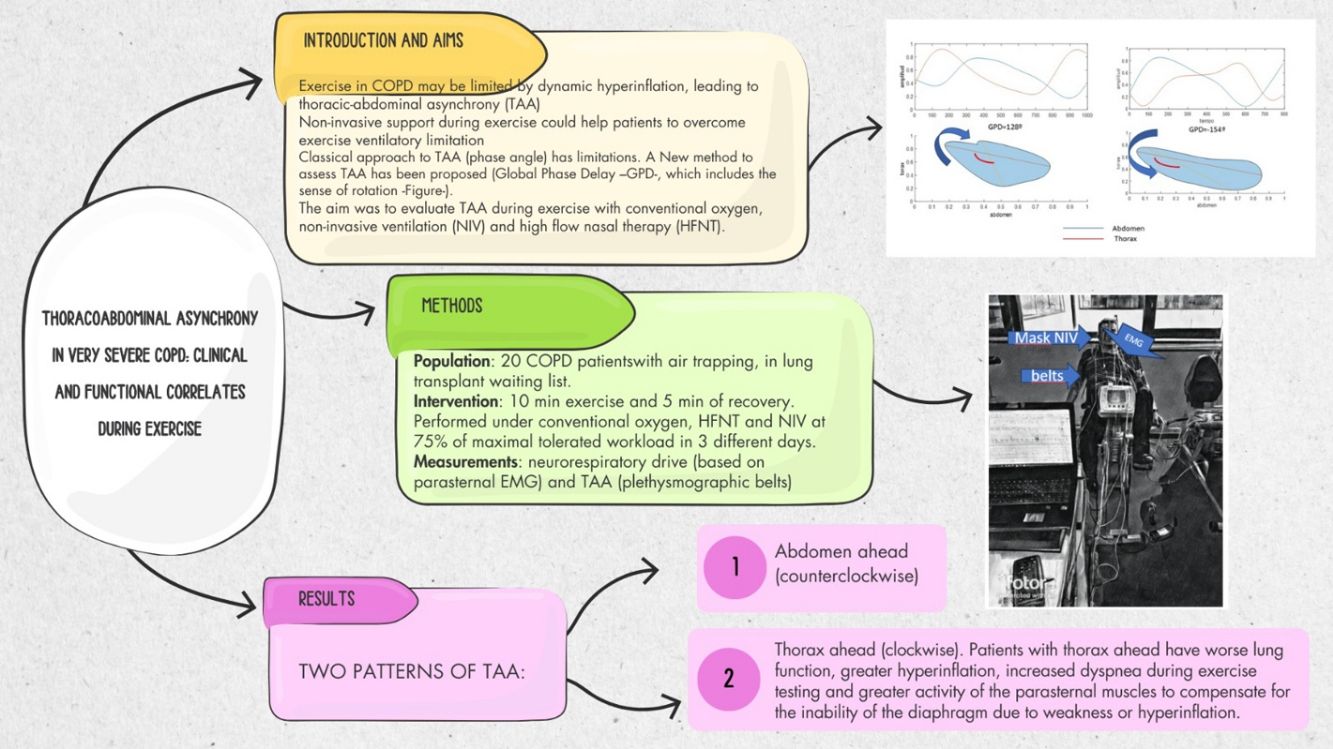
Patients with severe Chronic Obstructive Pulmonary Disease (COPD) often experience breathlessness and exercise limitations due to expiratory flow limitation. Pulmonary rehabilitation programmes, including exercise with non-invasive ventilation (NIV) or high-flow nasal therapy (HFT), aims to improve quality of life and exercise tolerance. This study investigates the relationship between thoracoabdominal asynchrony (TAA) during supported (NIV and HFT) and unsupported (conventional oxygen therapy – COT) exercise and clinical and functional parameters in severe COPD patients awaiting lung transplantation.
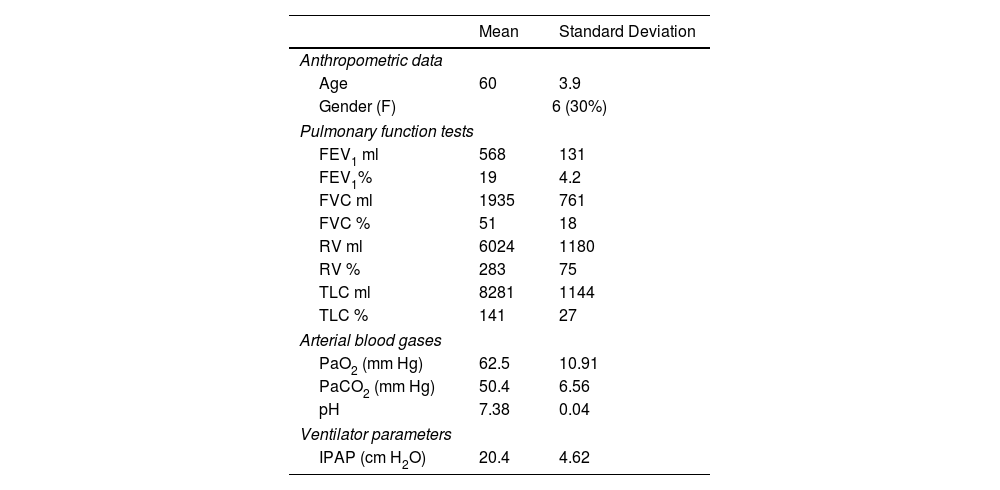
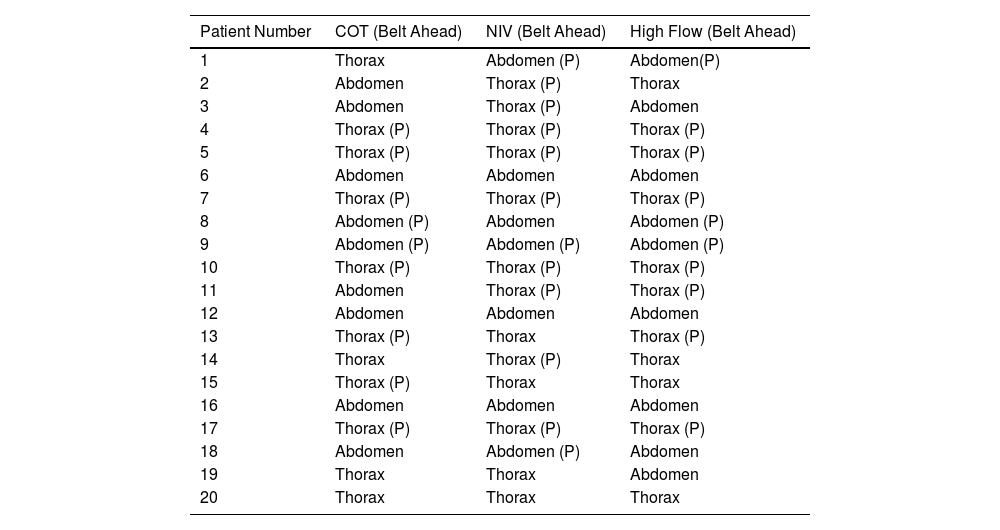
MethodsThis experimental, longitudinal, prospective, controlled study included 20 severe COPD patients on the lung transplant waiting list. Patients underwent three constant load exercise tests under COT, NIV, and HFT conditions. TAA was measured using respiratory inductance plethysmography, and neurorrespiratory drive (NRD) was assessed via parasternal electromyography.
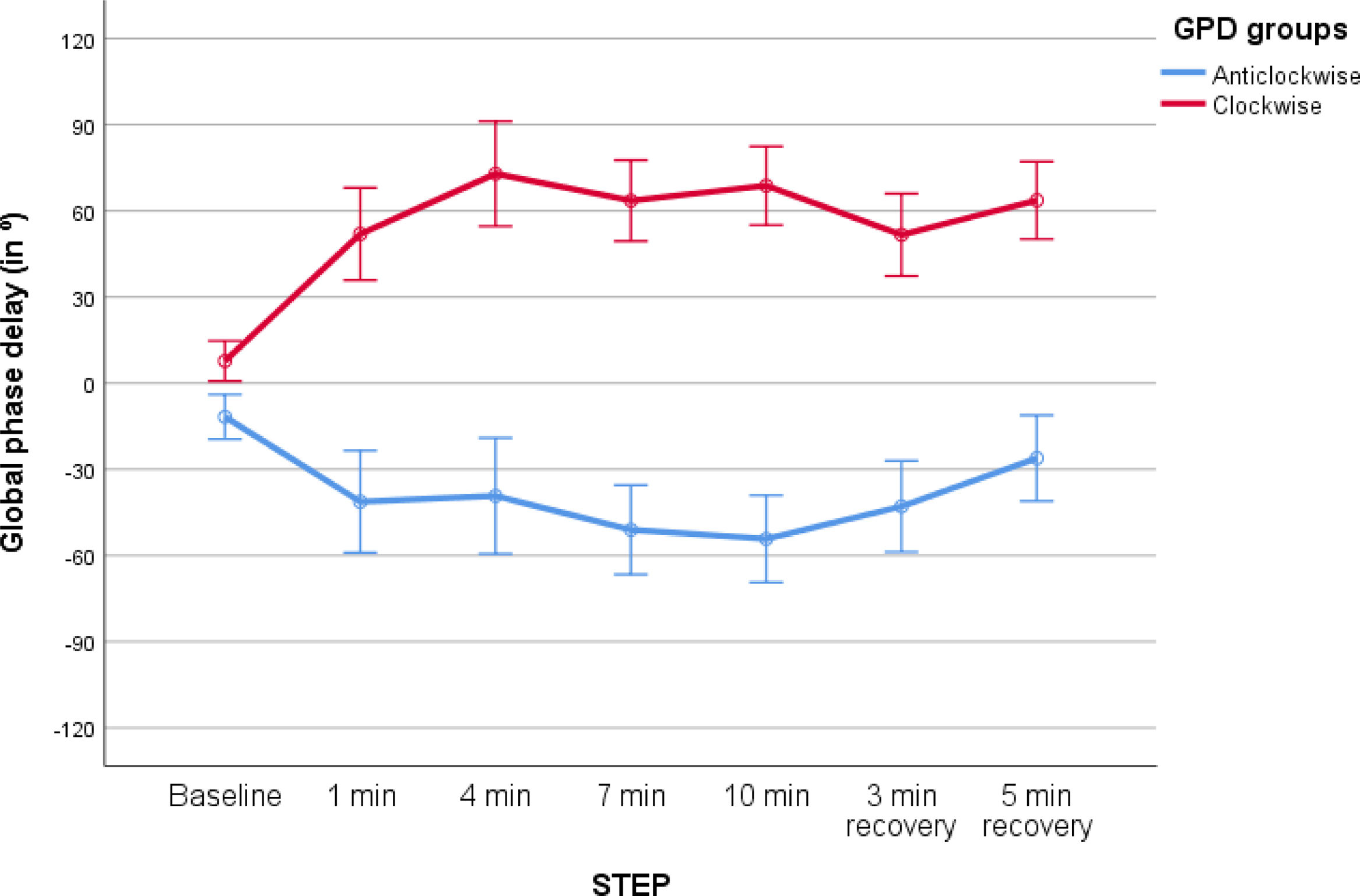
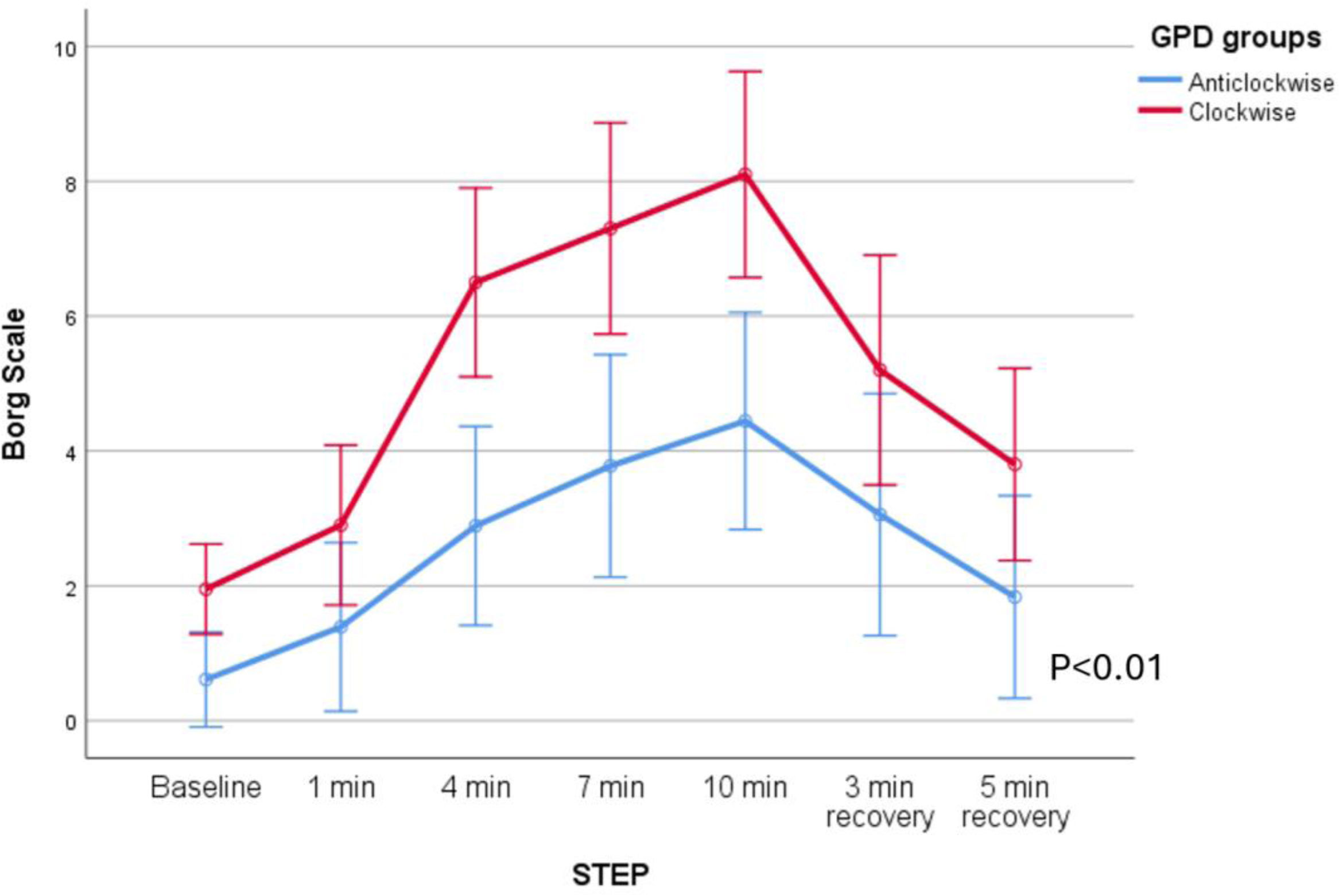
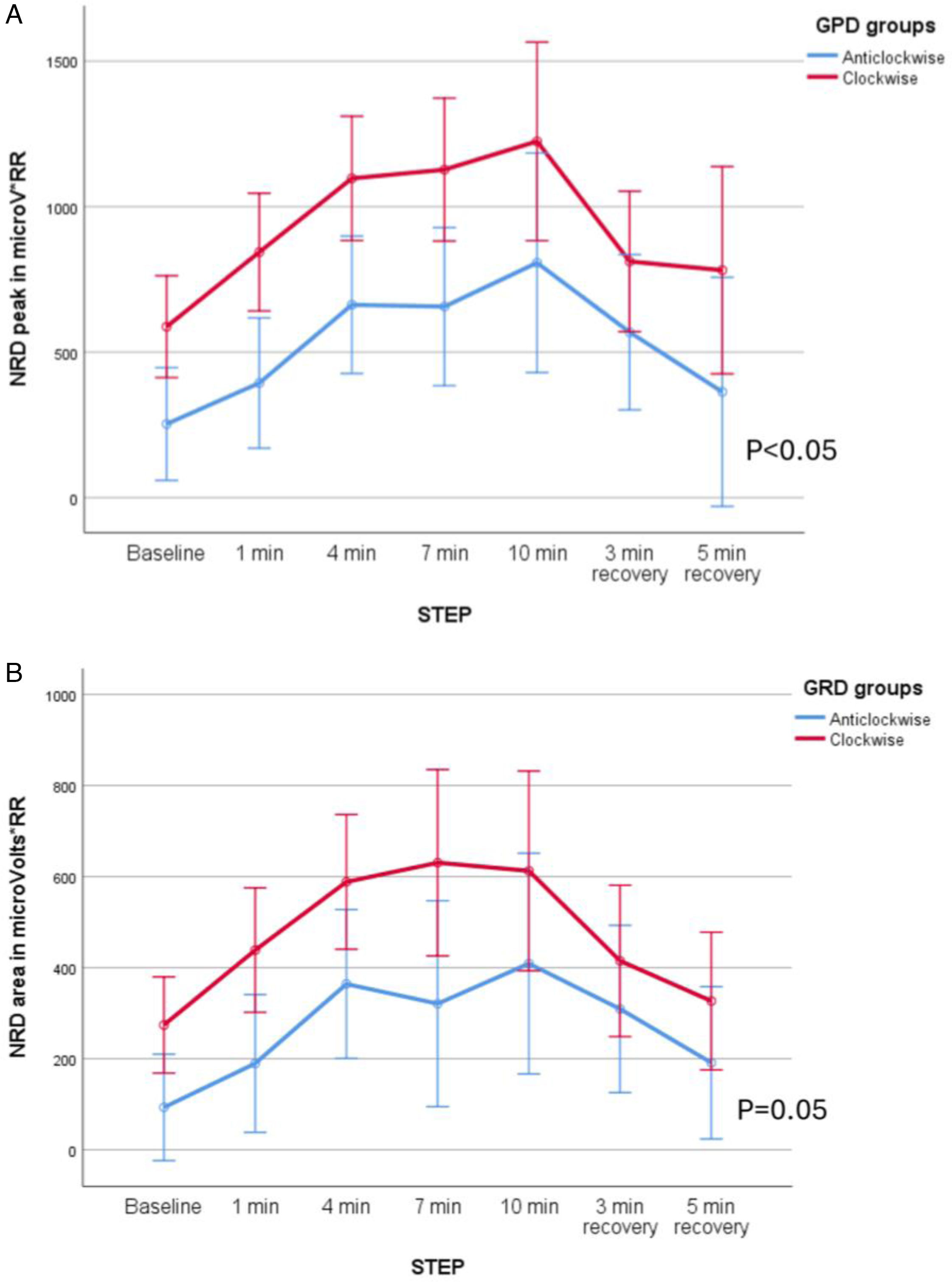
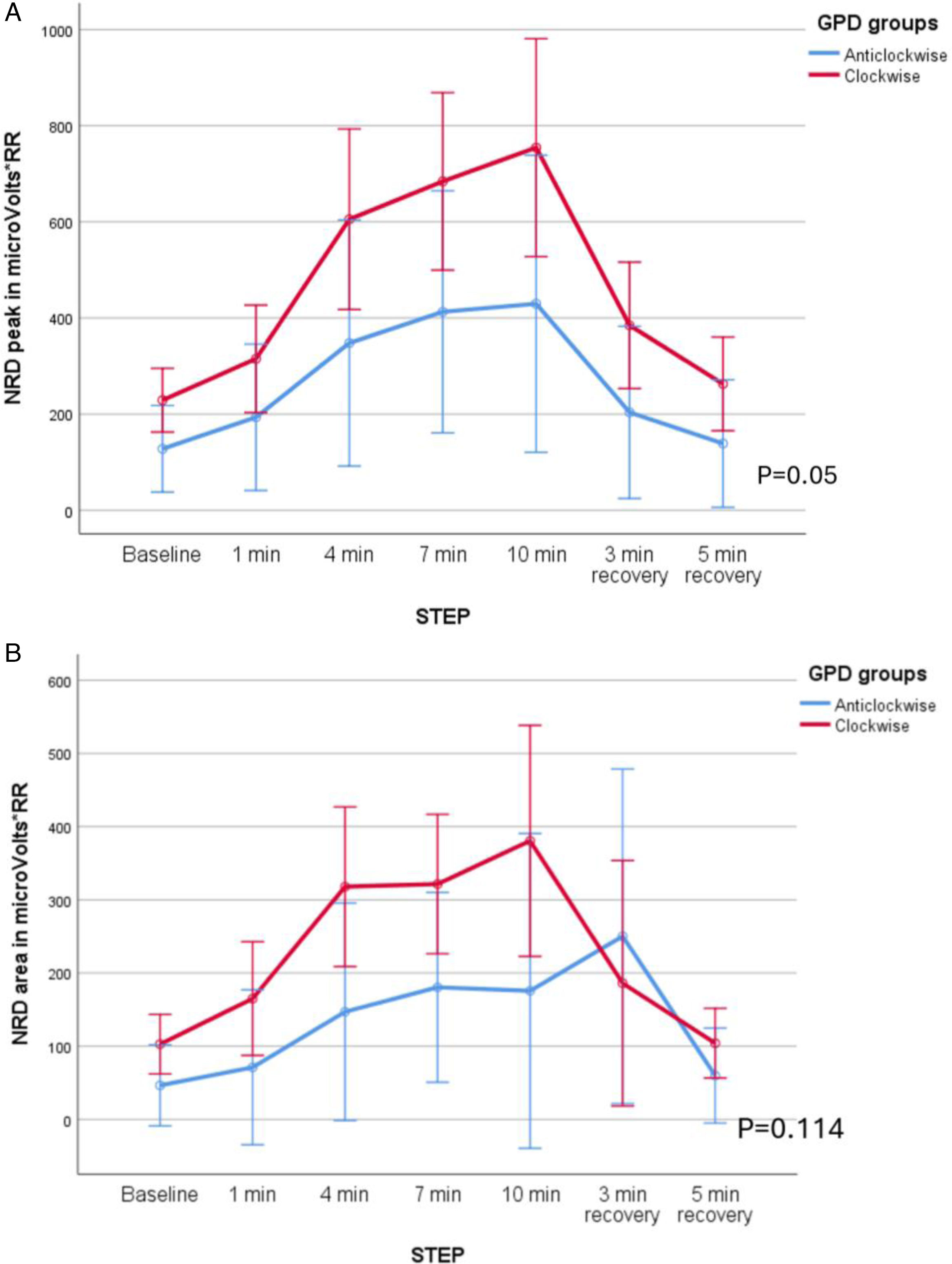
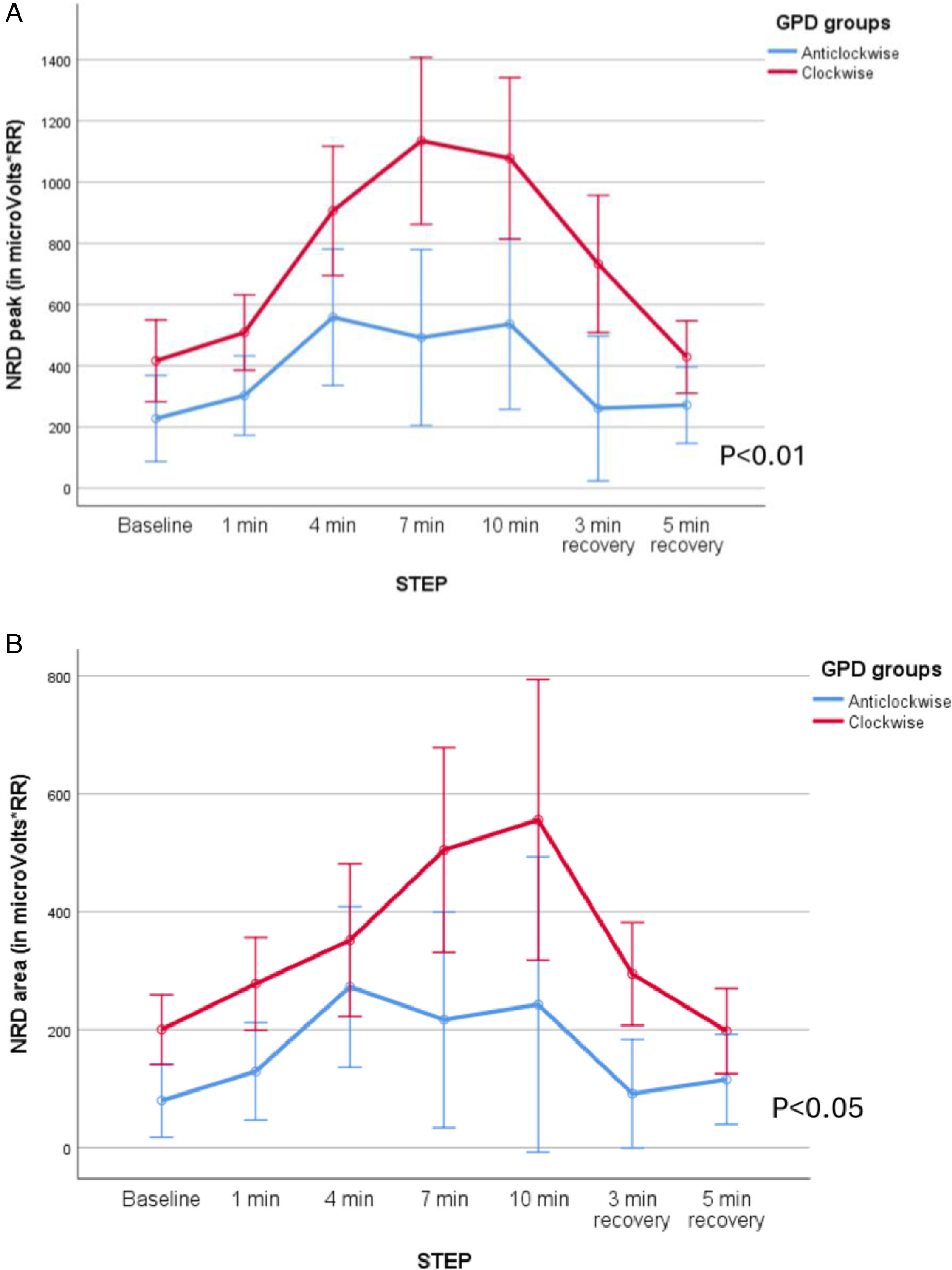
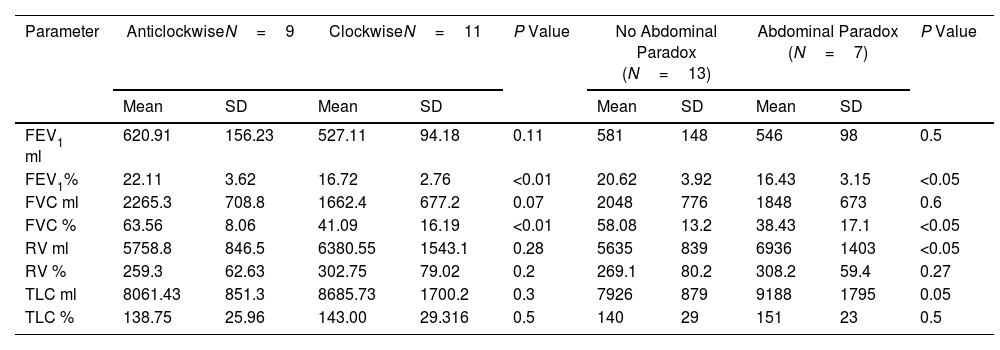
ResultsPatients exhibited distinct TAA patterns during exercise. Clockwise rotation (thorax ahead) was associated with worse baseline lung function, higher peak exercise dyspnoea and higher peak exercise NRD compared to counterclockwise rotation (abdomen ahead). No significant differences in TAA were observed between the three exercise conditions (COT, NIV, HFT). However, patients with clockwise TAA were more likely to have reduction in breathlessness with NIV compared to COT than those with counterclockwise rotation.
ConclusionsTAA patterns during exercise in severe COPD patients can indicate the severity of lung function impairment and predict severity of exercise induced dyspnoea. Analysis of TAA may predict response to respiratory support modalities and therefore monitoring TAA and NRD should be further studied to allow better tailoring of respiratory support during rehabilitation.