The Spanish Lung Transplant Registry (SLTR) began its activities in 2006 with the participation of all the lung transplantation (LT) groups with active programs in Spain. This report presents for the first time an overall description and results of the patients who received lung transplants in Spain from 2006 to 2010. LT activity has grown progressively, and in this time period 951 adults and 31 children underwent lung transplantation. The mean age of the recipients was 48.2, while the mean age among the lung donors was 41.7. In adult LT, the most frequent cause for lung transplantation was emphysema/COPD, followed by idiopathic pulmonary fibrosis, both representing more than 60% the total number of indications. The probability for survival after adult LT to one and three years was 72% and 60%, respectively, although in patients who survived until the third month post-transplantation, these survival rates reached 89.7% and 75.2%. The factors that most clearly influenced patient survival were the age of the recipient and the diagnosis that indicated the transplantation. Among the pediatric transplantations, cystic fibrosis was the main cause for transplantation (68%), with a one-year survival of 80% and a three-year survival of 70%. In adult as well as pediatric transplantations, the most frequent cause of death was infection.
These data confirm the consolidated situation of LT in Spain as a therapeutic option for advanced chronic respiratory disease, both in children as well as in adults.
El Registro Español de Trasplante Pulmonar (RETP) inició su actividad en 2006, participando en él todos los equipos de trasplante pulmonar (TP) con un programa activo en España. Este informe presenta por primera vez de forma global la descripción y resultados de los pacientes trasplantados de pulmón en España entre los años 2006 y 2010. La actividad de TP ha ido en progresivo aumento, trasplantándose en este periodo 951 adultos y 31 niños. La media de edad del receptor fue 48,2 años, siendo 41,7 años en el donante pulmonar. En el TP adulto, la causa más frecuente de trasplante fue el Enfisema/EPOC, seguido de la fibrosis pulmonar idiopática, representado ambas más del 60% del total de las indicaciones. La probabilidad de supervivencia tras el TP adulto a uno y tres años es del 72% y 60% respectivamente, si bien en los pacientes que sobreviven al tercer mes post trasplante, estas supervivencias son del 89,7% y 75,2%. Los factores que más claramente inciden en la supervivencia del paciente son la edad del receptor y el diagnóstico que indicó el trasplante. En los trasplantes pediátricos, la fibrosis quística es la principal causa de trasplante (68%), siendo la supervivencia al año del 80% y del 70% a los tres años. Tanto en el trasplante adulto como en el pediátrico, la causa más frecuente de fallecimiento es la infección.
Estos datos confirman la consolidación del TP en España como una opción terapéutica para la enfermedad respiratoria crónica avanzada, tanto en niños como en adultos.
Patient registries are tools that are very useful for determining the clinical reality of many processes. This is particularly relevant in rare processes and pathologies, such as in the case of solid organ transplants (SOT). There are national and international registries for most SOT that are a fundamental source of information for clinicians, researchers and healthcare authorities.
In Spain, lung transplantation (LT) is a clinical activity that has been getting developed over the course of the last 20 years. Currently, lung transplantation activity in Spain represents around 6% of the worldwide total. Therefore, Spanish lung transplantation groups have thought it necessary to develop a national lung transplantation registry. The Spanish Lung Transplant Registry (SLTR) was created in 2006 with the objective to understand and provide data about transplantation activity and to analyze the evolution of LT tendencies in Spain. The SLTR constitutes a common work platform for lung transplantation teams in our country, and it is expected to be of great use in national multi-center studies and to enable Spanish participation in international studies and/or registries.
The Registry is the result of the collaboration between the National Transplant Organization (NTO) and lung transplantation teams working in Spain. The Spanish LT groups are jointly responsible for developing the operational guidelines and selection of variables included in the SLTR. Data started to be collected in November 2006, including information about the donors, recipients and transplants, while reporting baseline as well as follow-up data. The database is managed by a computer application specifically designed for the registry (SURUS), which allows for data to be uploaded on-line through the website. The SLTR database is managed by the NTO, whose staff is in charge of donor data entry. A person from each lung transplantation team is responsible for entering the data of the recipient, surgical procedure and follow-up of transplant recipients at their respective hospitals. The NTO is in charge of annual data filtering and analysis as well as creating an annual report of SLTR results. Since 2007, SLTR participates in the International Society for Heart and Lung Transplantation (ISHLT) registry.1,2
The SLTR database is registered at the Spanish Agency for Data Protection, record number 2100491808, published in the BOE number 00003 04/01/2010 under resolution from 16/12/2009 of the National Transplant Organization, with ISO accreditation 27001:2007 (Information Systems Security Certification), record number ES-SI-0033/2008. This guarantees that the SLTR meets with the requirements established in the Data Protection Law 15/1999.
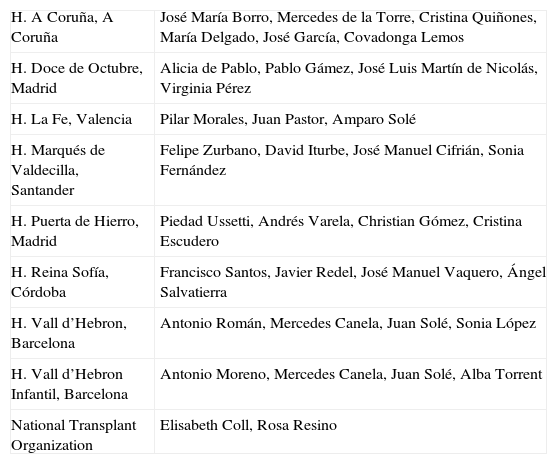
This document presents the description and analysis of the results from all the lung transplantations done by Spanish lung transplantation teams between 2006 and 2010. Annex 1 provides information on the participating groups, those responsible for the registry and the persons from each center and the NTO who collaborated in the data collection and transcription.
Statistical MethodsThe frequency distributions of the categorical variables are presented. Donor and recipient ages are reported with means and standard deviation (SD), together with frequency distributions after being stratified in different age groups.
Survival studies were analyzed using the Kaplan–Meier method, while log-rank was used to compare the curves. For comparisons of the variables with more than 2 categories, Cox proportional hazards models were used. The figures presented are truncated after 3 years, because beyond this time period the sample sizes did not reach the minimum value necessary for statistical assessment. The patient survival analysis included all the LT recipients for whom follow-up data were available.
In the risk factor study one year after transplantation, Cox proportional hazards models were also used. To ensure a follow-up time of at least one year in this analysis, we included only those transplantations performed from January 2006 to December 2009.
Both in the description of donors and recipients as well as in the survival data, cardiopulmonary transplantations were excluded. The evolution of cardiopulmonary transplantations is contained in the annual reports of the Spanish Heart Transplant Registry, which includes both heart as well as cardiopulmonary transplantations done in Spain since 1984.3
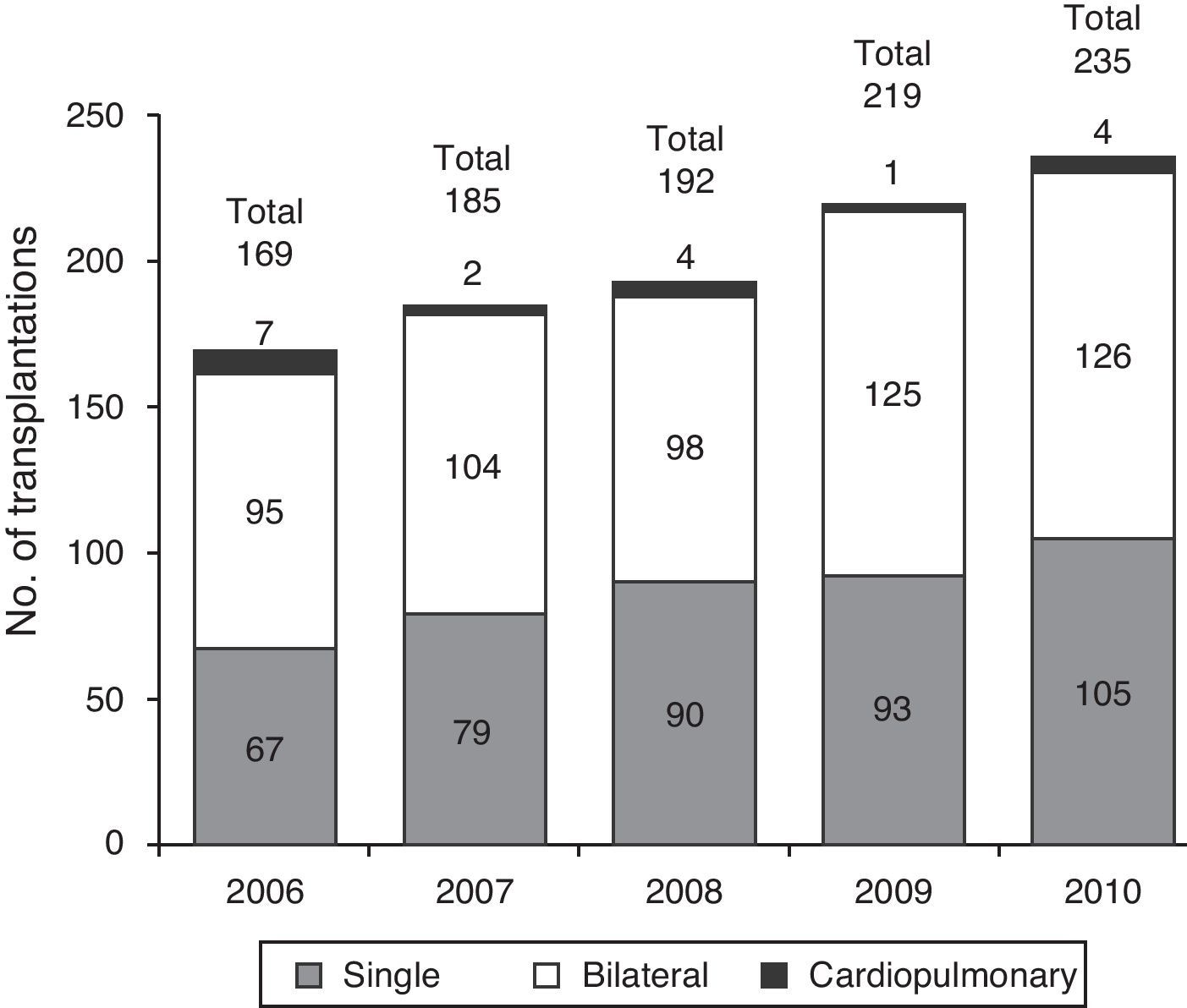
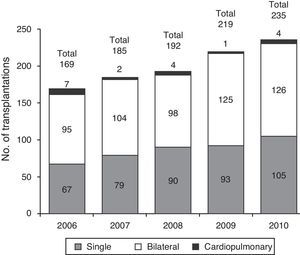
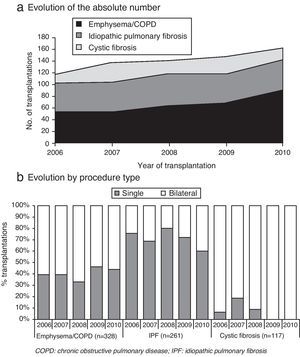
Transplantation Centers and ActivityIn the 5 years analyzed, a total of 1000 lung transplantations have been performed in Spain, with a progressive increase in activity over time (Fig. 1), an increase that was homogenous in the activity of all the groups (Table 1).
Activity of the Participating Centers (Spanish Lung Transplant Registry, 2006–2010).
| 2006 | 2007 | 2008 | 2009 | 2010 | Total | |
| H. Vall d’Hebron, Barcelona | 23 | 41 | 48 | 41 | 59 | 212 |
| H. Vall d’Hebron Infantil, Barcelona | 4 | 2 | 3 | 10 | 2 | 21 |
| C.H.U. A Coruña, A Coruña | 23 | 35 | 40 | 40 | 46 | 184 |
| H. Puerta del Hierro, Madrid | 46 | 35 | 31 | 34 | 35 | 181 |
| H. Marqués de Valdecilla, Santander | 25 | 16 | 23 | 33 | 30 | 127 |
| H. La Fe, Valencia | 26 | 30 | 23 | 24 | 24 | 127 |
| H. Reina Sofía, Córdoba | 22 | 26 | 23 | 27 | 25 | 123 |
| H. Doce de Octubre, Madrid | 1 | 10 | 14 | 25 | ||
| Total | 169 | 185 | 192 | 219 | 235 | 1000 |
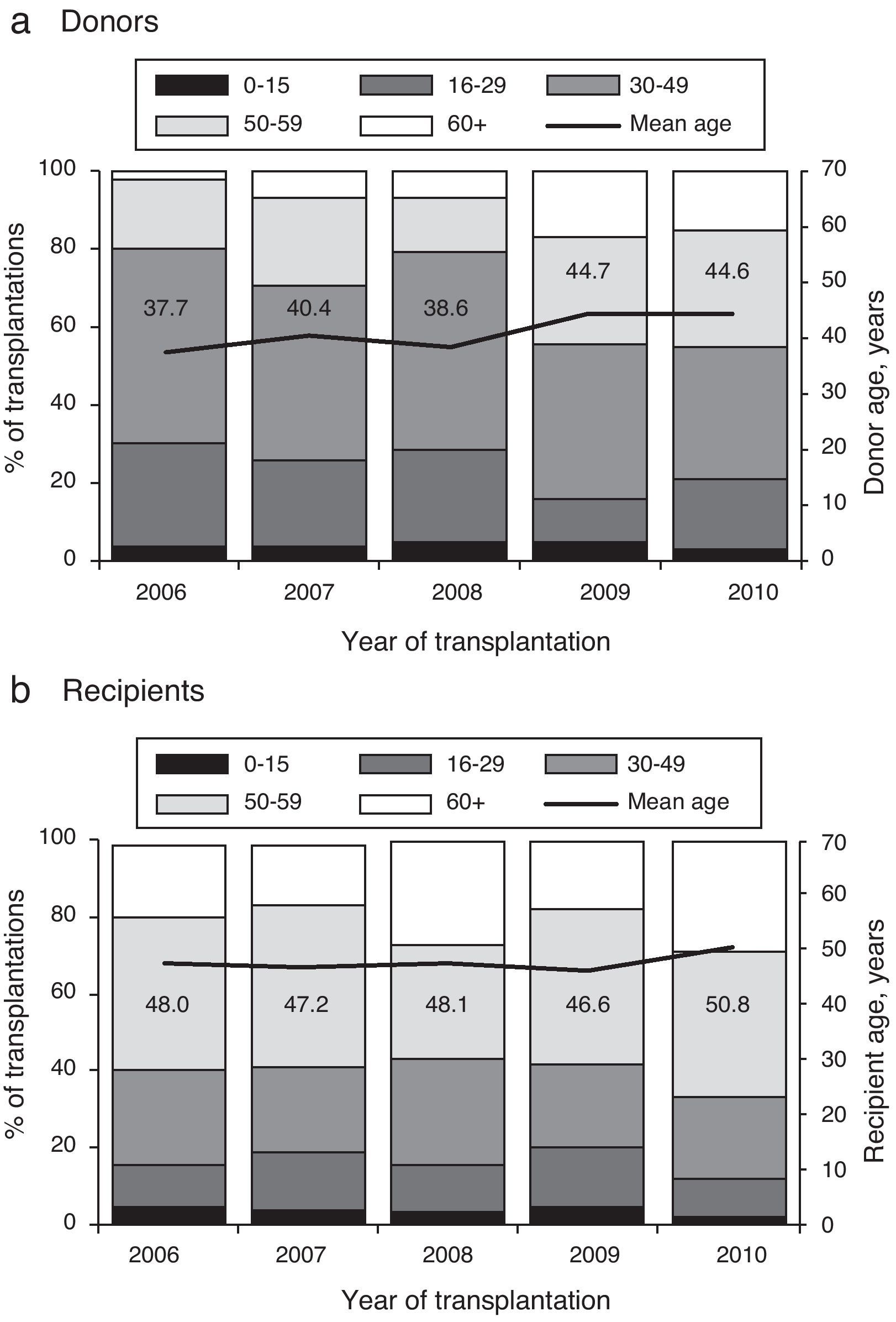
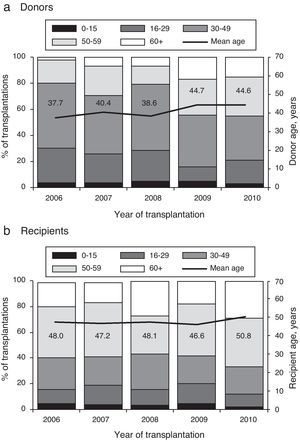
Mean donor age was 41.7 (SD, 14.6), and although this initially remained stable, it presented an increase of approximately 5 years, which remained stable in the last 2 years. The increase is fundamentally due to an increase in the number of donors from older age groups (Fig. 2a). The mean age of the recipients was 48.2 (SD, 14.7), and there were no significant changes during the study period, except for a slight increase detected in the last year (Fig. 2b).
Adult Lung TransplantationAdult lung transplantations are those in which the recipient is 15 years of age or older at the time of the transplantation. In the time period analyzed, a total of 951 adult lung transplantations were performed. There is no information available in the registry for one of these cases, and the adult lung transplantation analysis, therefore, refers to 950 patients.
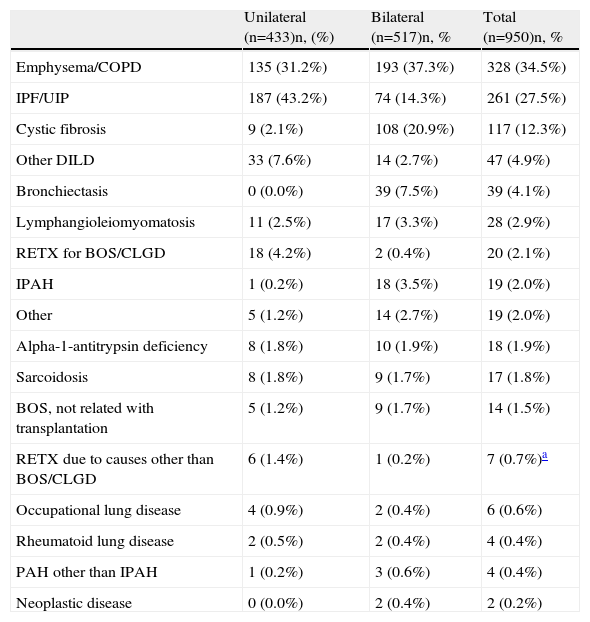
Indications and Transplantation TypeThe most frequent indication for lung transplantation in Spanish adults is emphysema/COPD, followed by idiopathic pulmonary fibrosis. These two diseases represent more than 60% of total LT indications (Table 2).
Distribution of Diagnoses and Transplantation Procedures of Adult Lung Transplant Recipients (Spanish Lung Transplant Registry, 2006–2010).
| Unilateral (n=433)n, (%) | Bilateral (n=517)n, % | Total (n=950)n, % | |
| Emphysema/COPD | 135 (31.2%) | 193 (37.3%) | 328 (34.5%) |
| IPF/UIP | 187 (43.2%) | 74 (14.3%) | 261 (27.5%) |
| Cystic fibrosis | 9 (2.1%) | 108 (20.9%) | 117 (12.3%) |
| Other DILD | 33 (7.6%) | 14 (2.7%) | 47 (4.9%) |
| Bronchiectasis | 0 (0.0%) | 39 (7.5%) | 39 (4.1%) |
| Lymphangioleiomyomatosis | 11 (2.5%) | 17 (3.3%) | 28 (2.9%) |
| RETX for BOS/CLGD | 18 (4.2%) | 2 (0.4%) | 20 (2.1%) |
| IPAH | 1 (0.2%) | 18 (3.5%) | 19 (2.0%) |
| Other | 5 (1.2%) | 14 (2.7%) | 19 (2.0%) |
| Alpha-1-antitrypsin deficiency | 8 (1.8%) | 10 (1.9%) | 18 (1.9%) |
| Sarcoidosis | 8 (1.8%) | 9 (1.7%) | 17 (1.8%) |
| BOS, not related with transplantation | 5 (1.2%) | 9 (1.7%) | 14 (1.5%) |
| RETX due to causes other than BOS/CLGD | 6 (1.4%) | 1 (0.2%) | 7 (0.7%)a |
| Occupational lung disease | 4 (0.9%) | 2 (0.4%) | 6 (0.6%) |
| Rheumatoid lung disease | 2 (0.5%) | 2 (0.4%) | 4 (0.4%) |
| PAH other than IPAH | 1 (0.2%) | 3 (0.6%) | 4 (0.4%) |
| Neoplastic disease | 0 (0.0%) | 2 (0.4%) | 2 (0.2%) |
COPD: chronic obstructive pulmonary disease; IPF/UIP: idiopathic pulmonary fibrosis/usual interstitial pneumonia; DILD: diffuse interstitial lung disease; RETX: re-transplantation; BOS/CLGD: bronchiolitis obliterans syndrome/chronic lung graft dysfunction; IPAH: idiopathic pulmonary arterial hypertension; PAH: pulmonary arterial hypertension.
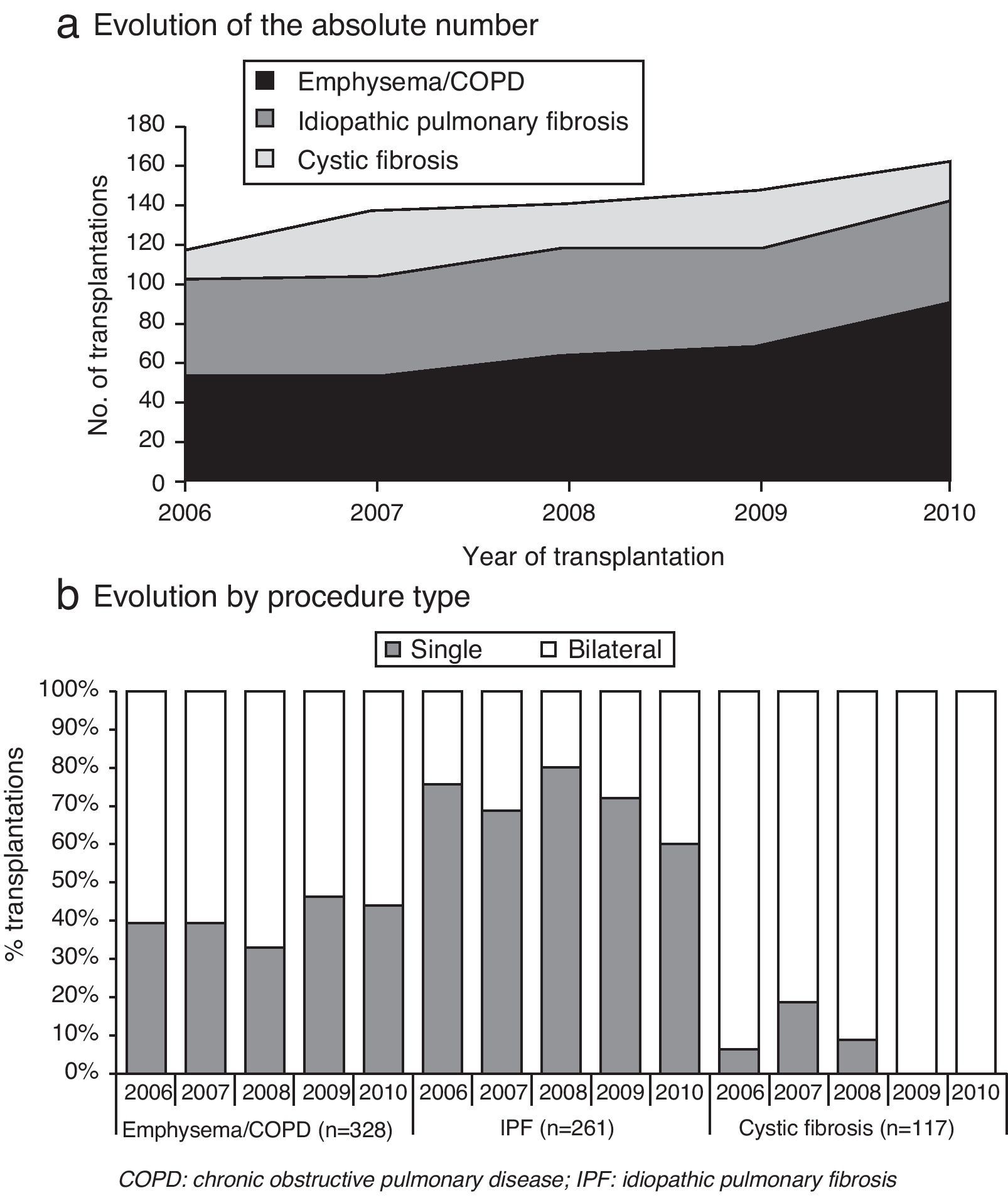
Fig. 3a shows the evolution over time of the main indications for lung transplantation. A progressive increase is observed in the indication for transplant due to emphysema/COPD that is relatively stable and greater than other indications.
The procedure type varies depending on the indication for transplantation (Fig. 3b). Bilateral transplant is the most frequent indication in cases of cystic fibrosis, which represents 100% of the cases in 2009 and 2010. Single-lung transplants predominate in patients with pulmonary fibrosis, although bilateral transplants seem to be increasing in frequency in the last 2 years. In emphysema/COPD, the distribution is almost 50% for each type of procedure.
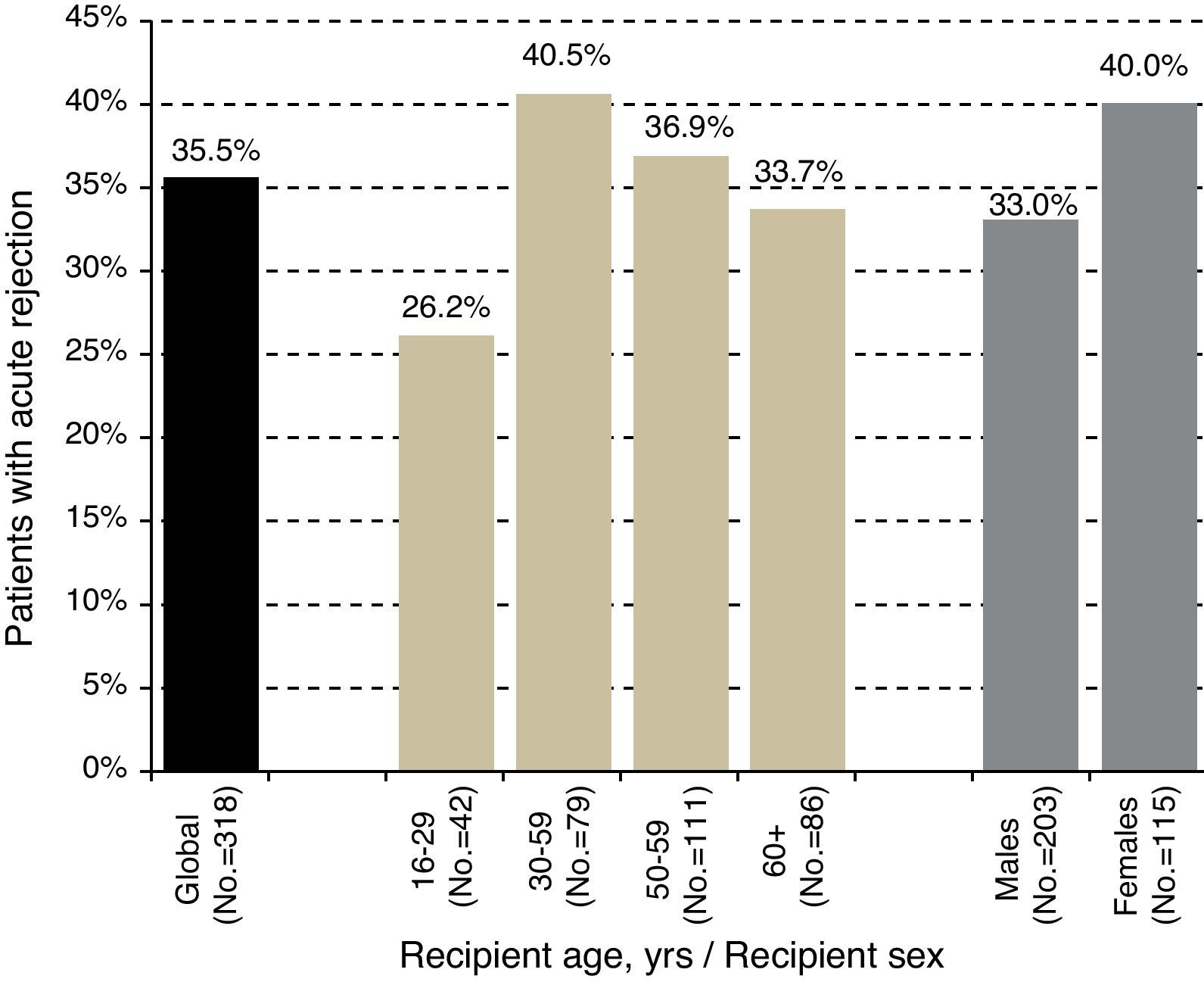
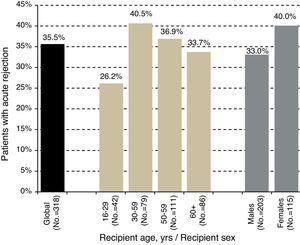
Acute RejectionApproximately one-third of patients who survived the first year port-transplantation have experienced at least one documented episode of acute rejection in this period, as shown in Fig. 4. This figure also presents this percentage broken down according to recipient sex and age groups.
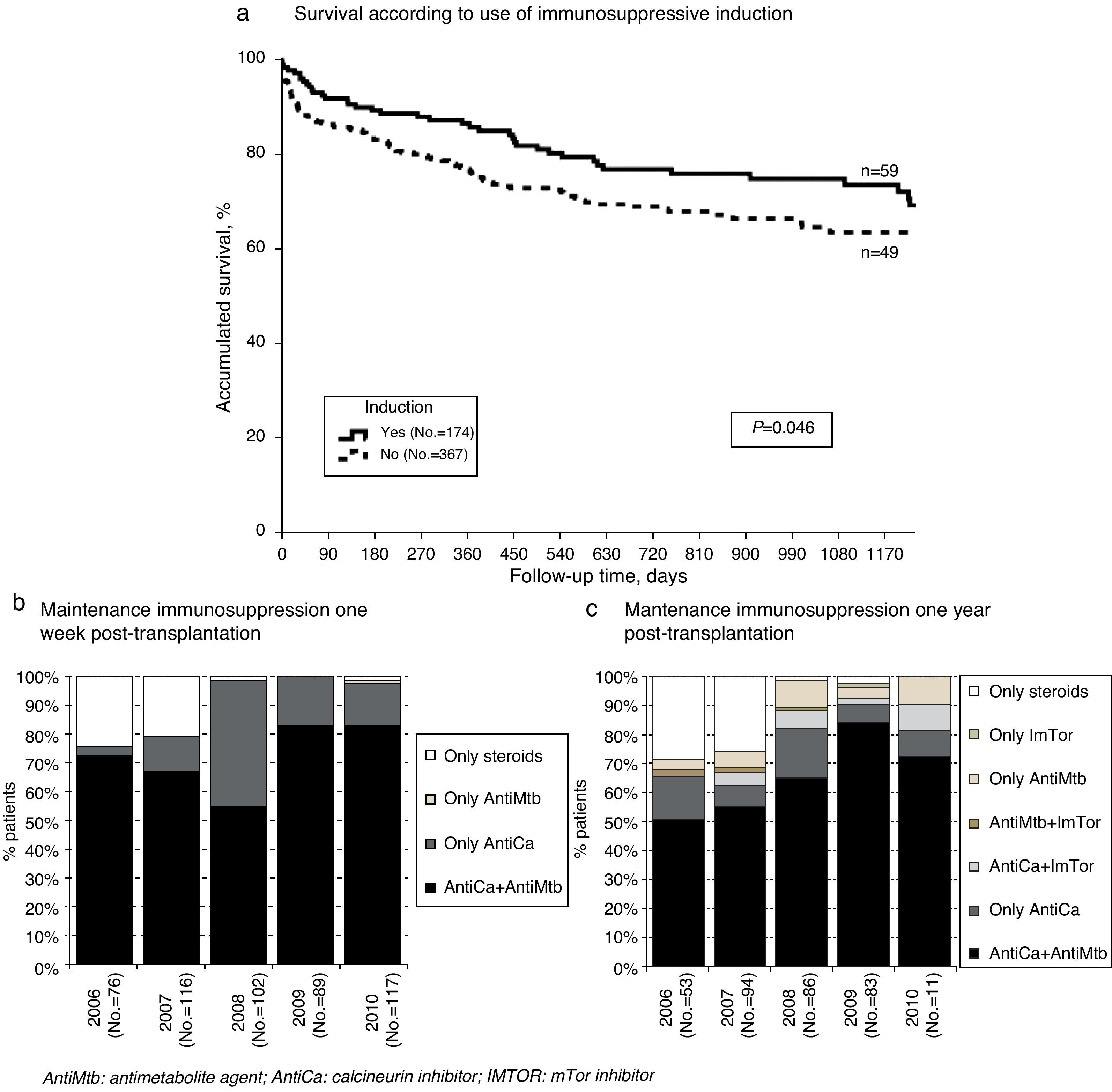
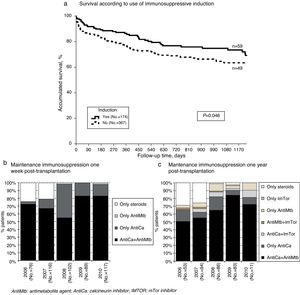
ImmunosuppressionWe have data available regarding induction immunosuppressive therapy for 541 adult lung transplant recipients (57% of the total), which may affect the representative nature of the sample in this section. Out of the 541, 32% received induction therapy, mainly anti-CD25 monoclonal antibody (basiliximab). The survival analysis shows a significant improvement in the patients who received induction therapy compared with those who did not receive this treatment (Fig. 5a); the difference is established between both groups between days 15 and 45 post-transplantation, after which it remained stable.
Survival curve associated with immunosuppressive induction (a); maintenance immunosuppression used in adult lung transplant recipients one week (b) and one year (c) post-transplantation (% patients) (regardless of the use of steroids in the combination) (Spanish Lung Transplant Registry, 2006–2010).
Most patients received triple immunosuppressive maintenance therapy, including steroids and a calcineurin inhibitor+an antimetabolic agent (Fig. 5b and c). Tacrolimus, together with mycophenolate mofetil or mycophenolic acid, has been predominantly used in recent years.
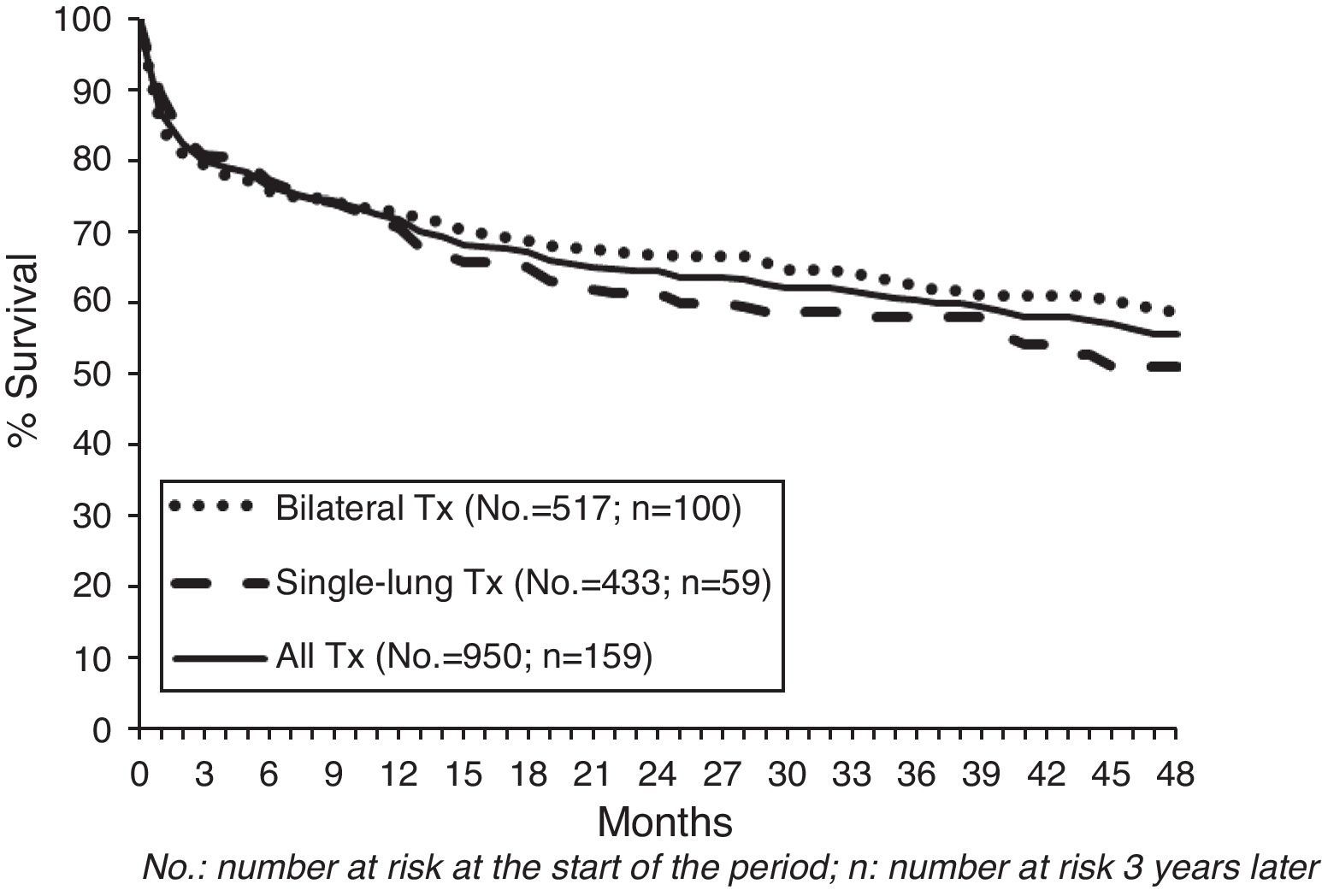
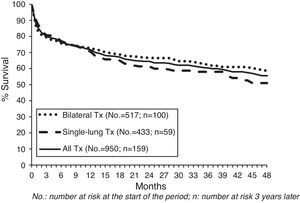
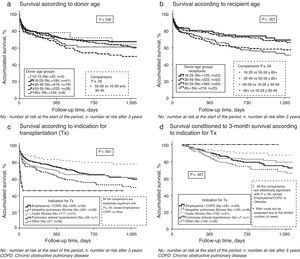
SurvivalFig. 6 shows the survival of adult lung transplant patients in Spain between 2006 and 2010. There are no significant differences in the survival observed between single-lung or bilateral transplantations. As in other registries, a tendency was observed toward presenting greater survival in patients with bilateral transplants (P=.190). However, other important factors should be considered, such as age (bilateral recipients are younger) that impact survival and may be a cause for bias in the results.
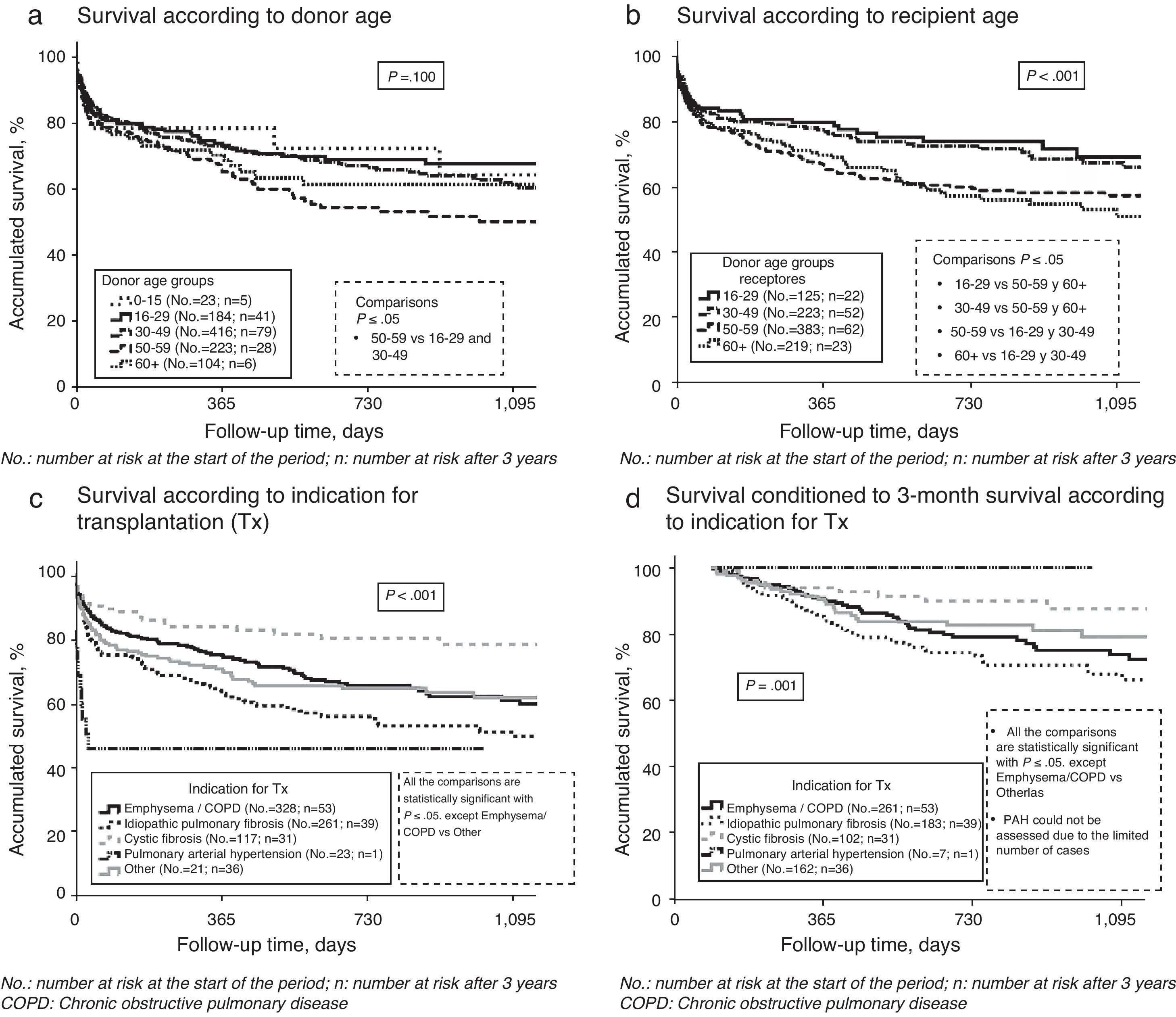
Unadjusted survival rates for 3 months, one year and 3 years were 79.9%, 71.7%, and 60.1%, respectively. In the patients who survive until the third month, one-year survival is 89.7% and 3-year survival is 75.2%. Better survival is observed when the recipients are under the age of 50 at the time of the transplantation (Fig. 7b).
Survival is different depending on the disease indicating the transplantation (Fig. 7c). Those receiving transplants due to idiopathic pulmonary hypertension have the poorest survival: 46% at three months. The limited number of cases with this indication for transplantation means that these data should be analyzed with caution, although in the literature greater perioperative mortality in this pathology.2 At the opposite extreme, with the best post-transplant survival rates, there are transplanted cystic fibrosis patients. When we analyze the conditioned survival starting at the third month post-transplantation (Fig. 7d), the differences are not as notable, although cystic fibrosis is still the indication with the greatest survival. This could be related with the fact that these patients are generally younger, although the difference also remains after adjusting for recipient age.
No statistically significant differences are observed in survival according to donor age (Fig. 7a), although the group of donors aged 50–59 present the poorest results. The better survival observed with donors aged 60 or older compared with the preceding age group may be due to the fact that these older donors are only selected if they meet all the criteria for suitability except for age, and thus may possibly present better overall characteristics despite their advanced age. When the donor cut-off age is set at 55, the limit that is usually used for “ideal” donors, there seems to be an observed tendency toward shorter survival in patients transplanted from older donors (P=.138).
As for CMV serostatus pairing between donor and recipient, the serologic state of the donor seems to have a greater influence (P=.099) than pairing itself (P=.244) and better results are seen when the donor is negative, although the difference does not reach statistical significance. It is important to take into account that this datum was not available for all recipients (n=514), and it is therefore recommended to interpret these results with caution as this limitation may introduce bias.
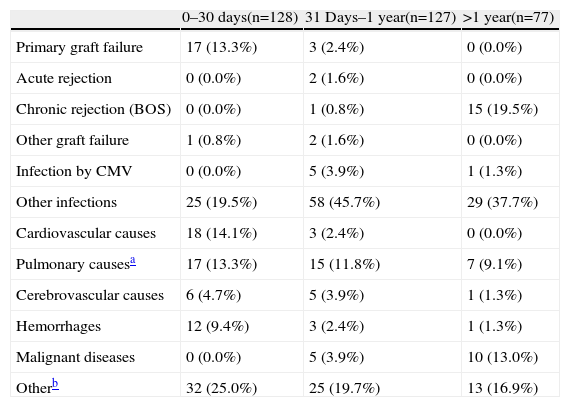
Causes of Death and Risk Factors for Mortality Within the First YearThe causes of death are presented in Table 3. Infections were the most frequent cause of mortality in the 3 periods analyzed.
Causes of Death of the Adult Lung Transplant Recipient (Spanish Lung Transplant Registry, 2006–2010).
| 0–30 days(n=128) | 31 Days–1 year(n=127) | >1 year(n=77) | |
| Primary graft failure | 17 (13.3%) | 3 (2.4%) | 0 (0.0%) |
| Acute rejection | 0 (0.0%) | 2 (1.6%) | 0 (0.0%) |
| Chronic rejection (BOS) | 0 (0.0%) | 1 (0.8%) | 15 (19.5%) |
| Other graft failure | 1 (0.8%) | 2 (1.6%) | 0 (0.0%) |
| Infection by CMV | 0 (0.0%) | 5 (3.9%) | 1 (1.3%) |
| Other infections | 25 (19.5%) | 58 (45.7%) | 29 (37.7%) |
| Cardiovascular causes | 18 (14.1%) | 3 (2.4%) | 0 (0.0%) |
| Pulmonary causesa | 17 (13.3%) | 15 (11.8%) | 7 (9.1%) |
| Cerebrovascular causes | 6 (4.7%) | 5 (3.9%) | 1 (1.3%) |
| Hemorrhages | 12 (9.4%) | 3 (2.4%) | 1 (1.3%) |
| Malignant diseases | 0 (0.0%) | 5 (3.9%) | 10 (13.0%) |
| Otherb | 32 (25.0%) | 25 (19.7%) | 13 (16.9%) |
BOS: bronchiolitis obliterans syndrome; CMV: cytomegalovirus.
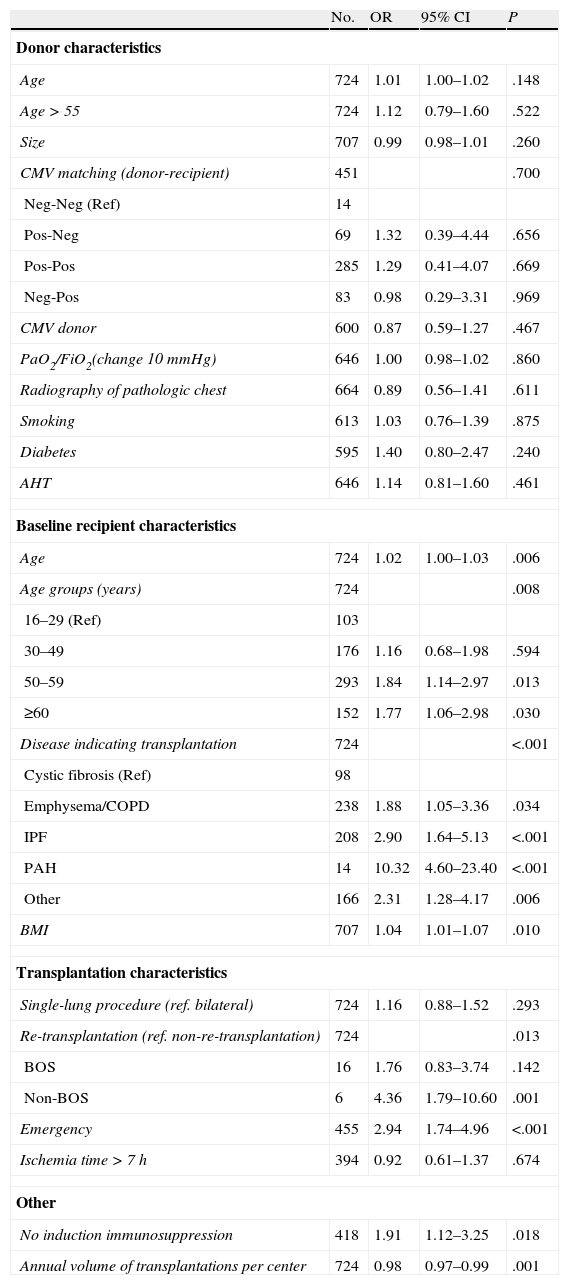
A univariate study was done of the risk factors for mortality one year post-transplant (Table 4). As explained in the methodology, to ensure a one-year follow-up we only included in the analysis those transplants done between 2006 and 2009. The analysis includes several variables from the donor, recipient and the transplantation procedure itself. The influence of other factors was also analyzed, like the use or not of induction immunosuppressive therapies and the volume of annual transplantations done by the transplant centers.
Variables Included in the Study of the Risk Factors for One-year Mortality of the Adult Lung Transplant Recipients (Spanish Lung Transplant Registry, 2006–2009).
| No. | OR | 95% CI | P | |
| Donor characteristics | ||||
| Age | 724 | 1.01 | 1.00–1.02 | .148 |
| Age>55 | 724 | 1.12 | 0.79–1.60 | .522 |
| Size | 707 | 0.99 | 0.98–1.01 | .260 |
| CMV matching (donor-recipient) | 451 | .700 | ||
| Neg-Neg (Ref) | 14 | |||
| Pos-Neg | 69 | 1.32 | 0.39–4.44 | .656 |
| Pos-Pos | 285 | 1.29 | 0.41–4.07 | .669 |
| Neg-Pos | 83 | 0.98 | 0.29–3.31 | .969 |
| CMV donor | 600 | 0.87 | 0.59–1.27 | .467 |
| PaO2/FiO2(change 10mmHg) | 646 | 1.00 | 0.98–1.02 | .860 |
| Radiography of pathologic chest | 664 | 0.89 | 0.56–1.41 | .611 |
| Smoking | 613 | 1.03 | 0.76–1.39 | .875 |
| Diabetes | 595 | 1.40 | 0.80–2.47 | .240 |
| AHT | 646 | 1.14 | 0.81–1.60 | .461 |
| Baseline recipient characteristics | ||||
| Age | 724 | 1.02 | 1.00–1.03 | .006 |
| Age groups (years) | 724 | .008 | ||
| 16–29 (Ref) | 103 | |||
| 30–49 | 176 | 1.16 | 0.68–1.98 | .594 |
| 50–59 | 293 | 1.84 | 1.14–2.97 | .013 |
| ≥60 | 152 | 1.77 | 1.06–2.98 | .030 |
| Disease indicating transplantation | 724 | <.001 | ||
| Cystic fibrosis (Ref) | 98 | |||
| Emphysema/COPD | 238 | 1.88 | 1.05–3.36 | .034 |
| IPF | 208 | 2.90 | 1.64–5.13 | <.001 |
| PAH | 14 | 10.32 | 4.60–23.40 | <.001 |
| Other | 166 | 2.31 | 1.28–4.17 | .006 |
| BMI | 707 | 1.04 | 1.01–1.07 | .010 |
| Transplantation characteristics | ||||
| Single-lung procedure (ref. bilateral) | 724 | 1.16 | 0.88–1.52 | .293 |
| Re-transplantation (ref. non-re-transplantation) | 724 | .013 | ||
| BOS | 16 | 1.76 | 0.83–3.74 | .142 |
| Non-BOS | 6 | 4.36 | 1.79–10.60 | .001 |
| Emergency | 455 | 2.94 | 1.74–4.96 | <.001 |
| Ischemia time>7h | 394 | 0.92 | 0.61–1.37 | .674 |
| Other | ||||
| No induction immunosuppression | 418 | 1.91 | 1.12–3.25 | .018 |
| Annual volume of transplantations per center | 724 | 0.98 | 0.97–0.99 | .001 |
Ref: reference value; CMV: cytomegalovirus; AHT: arterial hypertension; COPD: chronic obstructive pulmonary disease; IPF: idiopathic pulmonary fibrosis; PAH: pulmonary arterial hypertension; BMI: body mass index; BOS: bronchiolitis obliterans syndrome. Test used: Cox proportional hazards model.
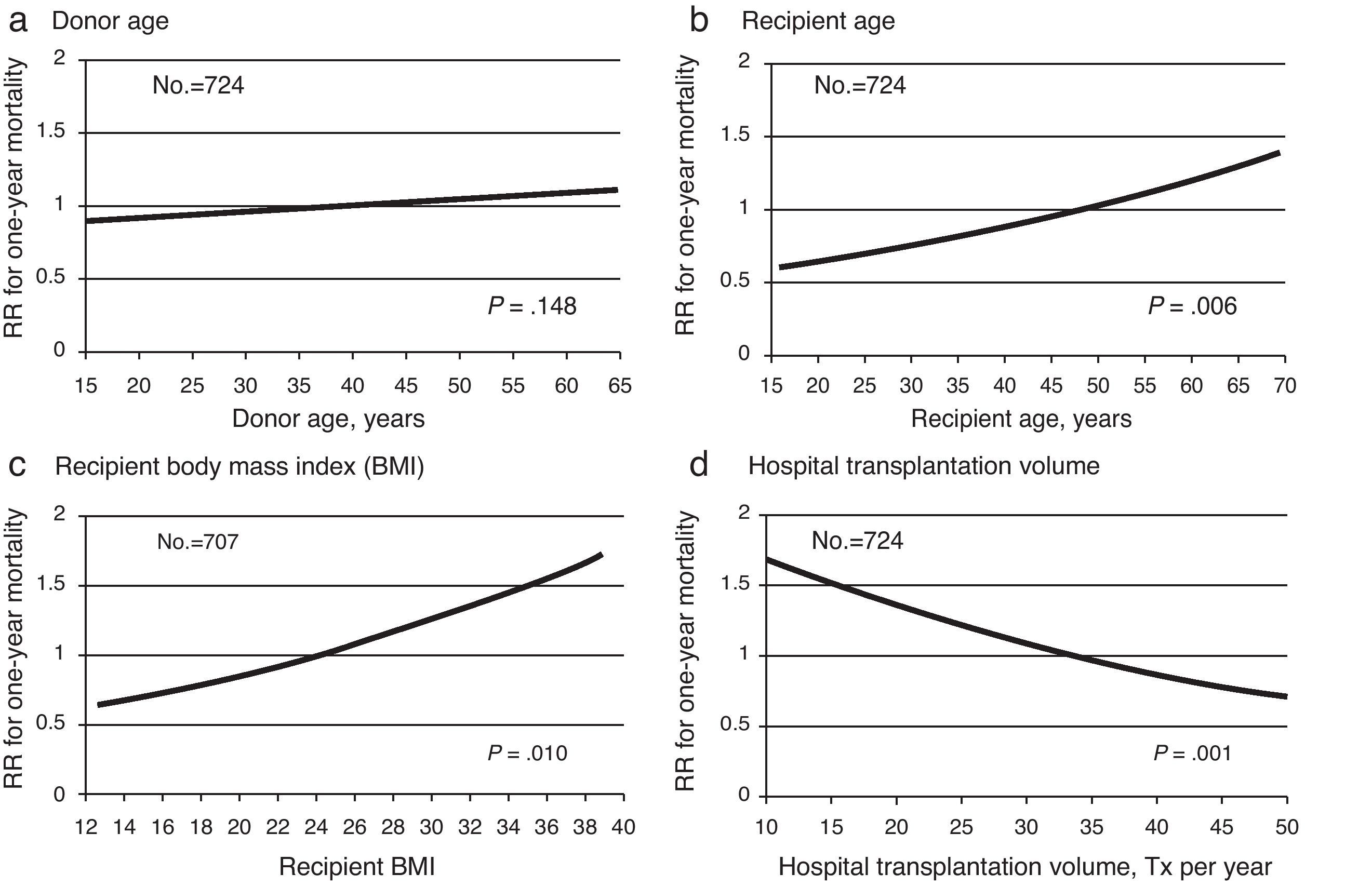
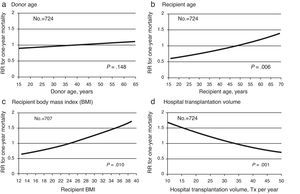
No association was found between the majority of the donor characteristics and one-year mortality in the adult lung transplant recipients. Only age seems to present a tendency to influence said mortality (Fig. 8a).
A poorer result is observed in the recipients aged between 50 and 59. In fact, there is a significant relationship (P=.006) between the age of the recipient and mortality one year after transplantation (Fig. 8b). Fig. 8c shows the directly proportional relationship obtained between recipient BMI and mortality in this time period.
All the indications for transplantation presented greater one-year mortality than cystic fibrosis. Re-transplantations due to acute problems in the immediate post-transplantation period, especially due to primary graft failure (generally related with procedures done in emergency situations), present a survival that is approximately 4 times lower than those who were not re-transplanted within the first year. It is important to highlight that re-transplantation due to chronic graft deterioration (bronchiolitis obliterans syndrome) does not present poorer one-year survival.
The number of transplantations done annually at the transplantation hospitals is also related with one-year survival (P=.001), and the results are generally better as the annual transplantation activity increases (Fig. 8d). A study done with data from the United Network for Organ Sharing (UNOS) registry found this same association.4
NeoplasmsTwelve cases of malignant neoplasms have been reported in the patients who survived one year after transplantation, which represents an incidence of 3.2%. The origins of the neoplasms were: 6 cases of lymphoproliferative disease (including one Kaposi's sarcoma), 5 organ carcinomas and a cutaneous basal-cell carcinoma.
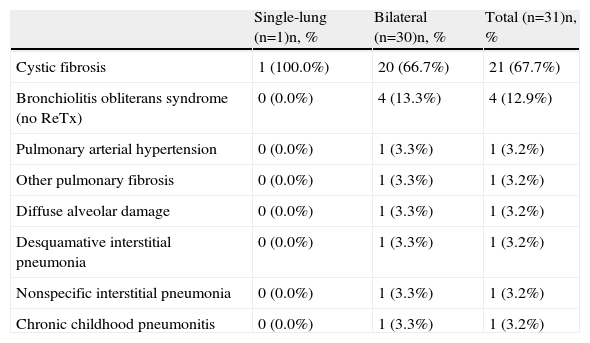
Pediatric Lung TransplantationPediatric lung transplantation is defined as those transplantations done in recipients under the age of 16 at the time of transplantation. The registry compiles a total of 31 pediatric lung transplantations between the years 2006 and 2010. As for the age of the recipients, one was under the age of 1 (3%), 7 were between 2 and 10 (23%) and 23 were between 11 and 15 (74%).
Indications and Type of TransplantationThe most frequent cause of lung transplantation in the patients under the age of 16 was cystic fibrosis, and the procedure used in more than 95% of the cases was bilateral transplantation (Table 5).
Distribution of Diagnoses and Transplantation Types in the Pediatric Lung Transplant Recipients (Aged <16) (Spanish Lung Transplant Registry, 2006–2010).
| Single-lung (n=1)n, % | Bilateral (n=30)n, % | Total (n=31)n, % | |
| Cystic fibrosis | 1 (100.0%) | 20 (66.7%) | 21 (67.7%) |
| Bronchiolitis obliterans syndrome (no ReTx) | 0 (0.0%) | 4 (13.3%) | 4 (12.9%) |
| Pulmonary arterial hypertension | 0 (0.0%) | 1 (3.3%) | 1 (3.2%) |
| Other pulmonary fibrosis | 0 (0.0%) | 1 (3.3%) | 1 (3.2%) |
| Diffuse alveolar damage | 0 (0.0%) | 1 (3.3%) | 1 (3.2%) |
| Desquamative interstitial pneumonia | 0 (0.0%) | 1 (3.3%) | 1 (3.2%) |
| Nonspecific interstitial pneumonia | 0 (0.0%) | 1 (3.3%) | 1 (3.2%) |
| Chronic childhood pneumonitis | 0 (0.0%) | 1 (3.3%) | 1 (3.2%) |
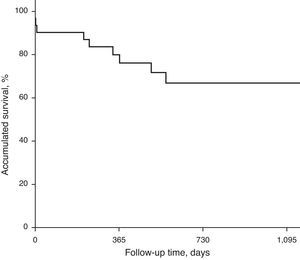
The survival curve of the pediatric transplantations is shown in Fig. 9. The unadjusted survival rates at 3 months, 1 year and 3 years are 90.3%, 80%, and 66.9%, with an No. at risk of 27, 21, and 4, respectively.
The limited number of pediatric transplantations does not allow for more detailed analyses.
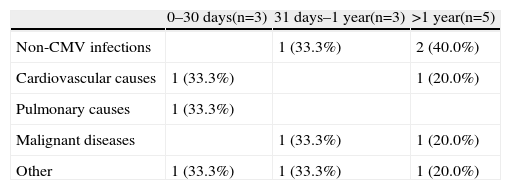
Causes of DeathThere were 11 deaths among the 31 pediatric transplant recipients between the years of 2006 and 2010. Details about the causes of death are given in Table 6.
Causes of Death of the Pediatric Lung Transplant Recipients (aged <16) (Spanish Lung Transplant Registry, 2006–2010).
| 0–30 days(n=3) | 31 days–1 year(n=3) | >1 year(n=5) | |
| Non-CMV infections | 1 (33.3%) | 2 (40.0%) | |
| Cardiovascular causes | 1 (33.3%) | 1 (20.0%) | |
| Pulmonary causes | 1 (33.3%) | ||
| Malignant diseases | 1 (33.3%) | 1 (20.0%) | |
| Other | 1 (33.3%) | 1 (33.3%) | 1 (20.0%) |
CMV: cytomegalovirus.
The limited number of pediatric transplantations does not allow for the study of mortality risk factors.
NeoplasmsThree cases were reported of malignant disease between the 14 patients with more than one year of follow-up, which was determined to be post-transplantation lymphoproliferative disease in each case.
ConclusionsThe data of the present registry are the first published information about global lung transplantation results in Spain. Overall, these data are comparable with the international experience published in the literature and they confirm the consolidation of lung transplantation in Spain as a therapeutic option for advanced chronic respiratory disease, both in children as well as in adults.
Results from the SLTR will be published periodically so that the lung transplantation results are up-to-date and may be an aid for both patients and professionals, while serving as a quality control of the transplantation process.
Conflict of InterestThe authors declare having no conflict of interest.
| H. A Coruña, A Coruña | José María Borro, Mercedes de la Torre, Cristina Quiñones, María Delgado, José García, Covadonga Lemos |
| H. Doce de Octubre, Madrid | Alicia de Pablo, Pablo Gámez, José Luis Martín de Nicolás, Virginia Pérez |
| H. La Fe, Valencia | Pilar Morales, Juan Pastor, Amparo Solé |
| H. Marqués de Valdecilla, Santander | Felipe Zurbano, David Iturbe, José Manuel Cifrián, Sonia Fernández |
| H. Puerta de Hierro, Madrid | Piedad Ussetti, Andrés Varela, Christian Gómez, Cristina Escudero |
| H. Reina Sofía, Córdoba | Francisco Santos, Javier Redel, José Manuel Vaquero, Ángel Salvatierra |
| H. Vall d’Hebron, Barcelona | Antonio Román, Mercedes Canela, Juan Solé, Sonia López |
| H. Vall d’Hebron Infantil, Barcelona | Antonio Moreno, Mercedes Canela, Juan Solé, Alba Torrent |
| National Transplant Organization | Elisabeth Coll, Rosa Resino |
Please cite this article as: Coll E, et al. Registro Español de Trasplante Pulmonar: primer informe de resultados (2006–2010). Arch Bronconeumol. 2013;49:70–8.