Ten years after the publication of the first GOLD strategy (Global Strategy for the Diagnosis, Management, and Prevention of COPD) for chronic obstructive pulmonary disease (COPD), the new revision published on the GOLD website at the end of 2011 represents a significant change in the diagnostic approach, clinical evaluation and therapeutic treatment of the disease. This revision debates not only the most significant aspects, which remain relatively intact, but also, and in particular, those that have been substantially modified compared with the GOLD revision from 2006.
Transcurridos 10 años desde la aparición de la primera estrategia GOLD (Global Strategy for the Diagnosis, Management, and Prevention of COPD) sobre la enfermedad pulmonar obstructiva crónica (EPOC), la nueva revisión publicada en la web de GOLD a finales del año 2011 supone un cambio significativo en lo que respecta al abordaje diagnóstico, evaluación clínica y planteamiento terapéutico de la enfermedad. En esta revisión se debaten no solo los aspectos más significativos que permanecen relativamente intactos sino también, y sobre todo, los que se han modificado de forma sustancial respecto a la revisión GOLD de 2006.
Ten years after the publication of the first GOLD (Global Strategy for the Diagnosis, Management, and Prevention of COPD) report about chronic obstructive pulmonary disease (COPD),1 the new version published on the GOLD website in late December 2011 represents a change in paradigm for the diagnosis, clinical evaluation and therapeutic approach to the disease.2 This article reviews and discusses the aspects that are still relatively intact and especially those that have changed substantially compared with the previous 2006 GOLD Guidelines.3
Work MethodologyIn September 2009 and May and September 2010, the members of the GOLD Scientific Committee identified all the bibliographies that were considered most relevant for the creation of the new main recommendations for COPD, especially those referring to diagnosis and treatment. Thus, while the annual updates for 2009 and 2010 were being published,2 all the chapters were being thoroughly revised and modifications were proposed with the aim to reach a consensus on the changes necessary for the new version. There was the perception among the GOLD members that, over the course of the last decade, significant advances had been made in the understanding of the disease that should be reflected in a significant paradigm shift in the new 2011 version.
In the summer of 2010, a subcommittee was created to prepare a draft with the proposed new chapters, whose content was presented at a symposium at the 2010 annual congress of the European Respiratory Society, in Barcelona. This subcommittee worked on these new recommendations until the spring of 2011. During this period of time, the GOLD Executive Committee and the National GOLD Representatives were informed about the most important aspects of these new recommendations and, in summer 2011, the National GOLD Representatives, together with other international experts, reviewed a very advanced version of the draft. In September 2011, The GOLD Scientific Committee reviewed all the comments and criticisms received and wrote the final text, which was made public at a symposium of the Asian Pacific Society of Respirology (APSR) at their annual congress in November 2011 in Shanghai.
Changes to the Structure of the DocumentThis new version is approximately 20% less voluminous than the 2007 version, both in length (down from 92 to 74 pages) and in bibliographic references (from 591 to 503). At the same time, however, the document includes new chapters. Chapter 1, which is the Background, has been substantially reduced, which means that if readers were interested in finding out more information about the physiopathology and biopathology of the disease, they would have to consult the numerous publications written about the topic during the last decade. Chapter 2 deals with the Diagnosis and evaluation of COPD. The definition of COPD varies very little from previous versions, although the word order has been modified to give greater clarity. On the other hand, significant changes have been made in the Evaluation of COPD, which now pivots around the impact of the symptoms, future risk of exacerbations, the severity of spirometric anomalies and the identification of comorbidities. There is a new chapter (Chapter 3) about Therapeutic options, which presents all the necessary information about pharmacological and non-pharmacological aspects, including drug side effects. Chapter 4 discusses the Treatment of stable COPD based on the new recommendations for the evaluation of these patients (Chapter 2). Finally, two new chapters are included that deal with the Treatment of exacerbations (Chapter 5) and the associated Comorbidities (Chapter 6).
Conceptual ChangesDefinition and DiagnosisIn this new 2011 version, the definition of COPD is practically unchanged from the earlier 20011 and 20063 versions, although the concept of COPD “systemic effects” is replaced with that of comorbidities. It also recognizes the extreme importance of exacerbation episodes of the disease in the course of its natural history.
The importance of airflow limitation in the definition and diagnosis of COPD is not only a basic pillar of the document, but it also is reinforced clearly and strictly stating that spirometry is an “essential requirement for the diagnosis” of COPD. It insists that the airflow limitation in COPD can only be reliably confirmed by spirometry, despite the fact that its availability for diagnosing COPD in clinical practice is neither uniform nor generalized. It goes even further by considering that, if spirometry is not used, a great disservice is done to the medical community and, ultimately, to all patients.
Therapeutic ObjectivesOne of the fundamental changes of these new 2011 GOLD guidelines has been to summarize all the therapeutic objectives of previous versions into two main ones: (a) to minimize (or avoid) the impact of the symptoms on the patient's state of health; and (b) to reduce the future risk of adverse situations for health, such as exacerbation episodes or mortality caused by the disease.4 This approach has a direct impact on the proposed clinical assessment of COPD patients by the 2011 GOLD strategy, as discussed in detail in the section below.
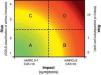
Clinical Evaluation of Chronic Obstructive Pulmonary Disease PatientsOne of the fundamental changes of the 2011 GOLD guidelines is to propose a multidimensional clinical evaluation of COPD patients including (although optimizing) the unidimensional proposal of previous editions based, fundamentally, on spirometric findings. Thus, in the context of the 2 therapeutic objectives previously discussed, this new edition proposes assessing (Fig. 1): (a) the impact of the disease on symptoms and the patient's state of health; and (b) the risk of future events (exacerbations and mortality). To do so, the following tools are recommended.
Clinical evaluation of COPD patients proposed by the new 2011 GOLD strategy. Letters A–D represent the 4 patient categories according to the presence of symptoms (few [patients A and C] or many [patients B and D]) and risk of FEV1<50% the reference value or number of exacerbations (low [patients A and B] or high [patients C and D]). For more information, see the original text at http://www.goldcopd.org. CAT (COPD Assessment Test): abbreviated COPD quality of life questionnaire; mMRC (modified Medical Research Council): modified MRC dyspnea scale. Used with the permission of the Global Strategy for Diagnosis, Management and Prevention of COPD 2011, Global Initiative for Chronic Obstructive Lung Disease (GOLD), www.goldcopd.org.
Although improvement of symptoms and health state were two of the main objectives for the treatment recommended by GOLD in earlier editions, the impact of the disease in patients (e.g. symptoms and health state) was not contemplated in therapeutic decision-making. Meanwhile, their use as an evaluational tool was always considered a complex process and was practically relegated to the world of clinical assays. This circumstance has changed in the new 2011 version. Today there are new questionnaires for quantifying the impact of the disease and the state of health on patients that can be used in clinical practice, such as the British modified Medical Research Council (mMRC) scale5 or the COPD Assessment Test (CAT),6 respectively, the later with a much shorter format than the classic Saint George's Respiratory Questionnaire (SGRQ).7 All of them are easy to use in clinical practice and there are validated translations available for the most common languages.
Airflow Limitation (GOLD Grades)One of the strengths of the original GOLD strategy was the simple, intuitive proposal of the spirometric classification of COPD severity. For this reason, the old spirometric classification of airflow in 4 grades (GOLD 1, mild; GOLD 2, moderate; GOLD 3, severe, and GOLD 4, very severe) remains in the 2011 version. Nevertheless, it has been demonstrated that the FEV1 value is not a reliable marker for dyspnea severity (the cardinal symptom of COPD), limitation of physical activity or the deterioration in quality of life. Thus, the new 2011 GOLD version replaces the old term “stage” for the new one of “grade”, while maintaining the original spirometric classification, as a solid predictor for the risk of future events (Fig. 1), such as exacerbations and death. We should highlight that blood gas criteria, which were contemplated in the spirometry in all the previous editions, have now been suppressed inasmuch as their inclusion in the 3 spirometric criteria is arbitrary.
The set post-bronchodilator FEV1/FVC ratio (<0.70) remains as a recommended cut-point in order to define the presence of airflow limitation, although its use in older individuals (>50–60 years) may provide false COPD diagnoses due to the fact that, as is known, the normal aging process affects both lung volumes as well as airflows. Contrarily, in younger adults (<45 years) the use of this ratio may make the COPD diagnosis go unnoticed.8
Risk of ExacerbationsThe exacerbation episodes that some COPD patients present have a very significant deleterious effect on their state of health as well as clinical-functional decline, vital prognosis and socioeconomic costs. A recent study9 has shown that those with frequent exacerbations (2 or more per year) constitute a defined, stable group with a poorer prognosis, therefore the 2011 GOLD Guidelines include the assessment of the frequency of exacerbations as a risk factor in addition to the spirometric criterion (Fig. 1). The best method for identifying frequent exacerbators is by directly asking the patient about his/her medical history.9
Combined Clinical Evaluation (Fig. 1)The new multidimensional clinical evaluation system for COPD patients proposed by the new GOLD version is a very significant change over previous editions, although it maintains a certain link with these by continuing to include spirometry testing. This new system is based on the joint evaluation of the impact of patients’ symptoms on their state of health and the risk of future adverse events on health. For this latter proposition, 2 variables are proposed (severity of airflow limitation and frequency of exacerbations) and to modulate the treatment use whichever of the two that is associated with greater risk. This new therapeutic approach does not require sophisticated technology, and it therefore can be applied in any clinical situation and place. Furthermore, it situates the treatment of COPD within the context of a more personalized clinical practice that is closer to the individual needs of each patient. Although an alternative strategy based on phenotypes10,11 was discussed, it was not considered because the scientific evidence supporting phenotypes is still incomplete.
Treatment of Stable Chronic Obstructive Pulmonary DiseaseThere is a continued emphasis on the importance of identifying and reducing risk factors, among which smoking is the most influential in the development of COPD in our setting. Thus, its eradication represents one of the most difficult challenges for the prevention and control of COPD. Nevertheless, the relevance of other risk factors is highlighted to keep these in mind as much as possible. They include occupational dusts, certain chemical products and inhalation of air in the home that is polluted with biomass (smoke from wood fires, etc.) used for cooking or heating in poorly ventilated rooms. This latter circumstance is especially relevant in women in developing countries.
Unlike earlier editions that based the therapeutic recommendations almost exclusively on spirometric anomalies,12 in this new edition they are now based on multidimensional evaluation, as previously commented (Fig. 1). The guidelines now identify 4 different patient categories (A, B, C and D), combining symptoms (few or many) with risk (low or high), so that the new possible therapeutic recommendations adapt to each of the categories. At the same time, they are divided into three possibilities: (a) an initial recommendation; (b) ALTERNATIVE option; and (c) other POSSIBLE alternatives.
Treating ExacerbationsThe definition and diagnosis of exacerbations remain unchanged from those proposed one decade ago.13 The need for appropriate oxygen therapy for the more critical situations is emphasized, above all in patients with acute respiratory failure. The document also underlines the solid scientific evidence for using non-invasive ventilation in the exacerbations that run their course with hypercapnic respiratory failure. It also includes proposals for the later follow-up of these acute episodes and the prevention of future exacerbations.
Treating ComorbiditiesDue to their clinical importance, for the first time a whole chapter is dedicated to the treatment of comorbidities in COPD: cardiovascular diseases, osteoporosis, anxiety and depression, lung cancer, infections, metabolic syndrome and diabetes mellitus.14 Basically, it is recommended that these comorbidities should be approached therapeutically, as would be done in any other clinical situation, regardless of the presence of COPD.
ConclusionsThe 2011 revision of the GOLD strategy is the evolution of a series of recommendations based on the best scientific evidence available for the diagnosis and treatment of COPD which was initiated over a decade ago. In this version, very significant changes are introduced in the clinical evaluation of patients, which goes from being unidimensional (e.g. airflow limitation) to multidimensional (e.g. symptoms, spirometry, exacerbations and comorbidities). This new proposal for clinical assessment represents a considerable change in the therapeutic recommendations for patients with stable COPD. Furthermore, this new edition includes new and specific chapters that are dedicated to the treatment of COPD exacerbations and its most frequent comorbidities. Therefore, in our modest opinion, the new 2011 GOLD strategy can truly be considered a change of paradigm.
The complete report of the 2011 GOLD Revision can be consulted on their website (http://www.goldcopd.org). The site also offers the GOLD Pocket Guide for general consultations of health-care professionals, patients and family members. Lastly, the website includes a very complete collection of more than 100 slides for educational use that have been transplanted into Spanish by the current Spanish National GOLD representative, Dr. Juan Pablo de Torres (Pamplona).
Conflict of InterestsRR-R has given conferences for Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Kyorin, Novartis and Pfizer. He has also consulted for Almirall, Boehringer Ingelheim, Dey, Merck, Novartis, Nycomed, Pearl Therapeutics and Pfizer, and has received donations from Almirall and Esteve related with COPD projects. AA has given conferences for Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Nycomed and Sepracor. He has consulted for Almirall, AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Nycomed, Roche and Sepracor, and has received donations from Almirall, GlaxoSmithKline and Nycomed related with COPD projects.




![Clinical evaluation of COPD patients proposed by the new 2011 GOLD strategy. Letters A–D represent the 4 patient categories according to the presence of symptoms (few [patients A and C] or many [patients B and D]) and risk of FEV1<50% the reference value or number of exacerbations (low [patients A and B] or high [patients C and D]). For more information, see the original text at http://www.goldcopd.org. CAT (COPD Assessment Test): abbreviated COPD quality of life questionnaire; mMRC (modified Medical Research Council): modified MRC dyspnea scale. Used with the permission of the Global Strategy for Diagnosis, Management and Prevention of COPD 2011, Global Initiative for Chronic Obstructive Lung Disease (GOLD), www.goldcopd.org.](https://static.elsevier.es/multimedia/15792129/0000004800000008/v1_201305150600/S1579212912000997/v1_201305150600/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w98FxLWLw1xoW2PaQDYY7RZU=)








