The objective of this study was to determine the level of knowledge about chronic obstructive pulmonary disease (COPD) and its determinants in the general population of Spain, and to compare it with a similar survey conducted in 2002.
MethodsWe conducted a cross-sectional, observational, epidemiological study in September 2011 by means of a telephone interview with a representative sample of individuals aged 40–80years living in all 17 regions of Spain.
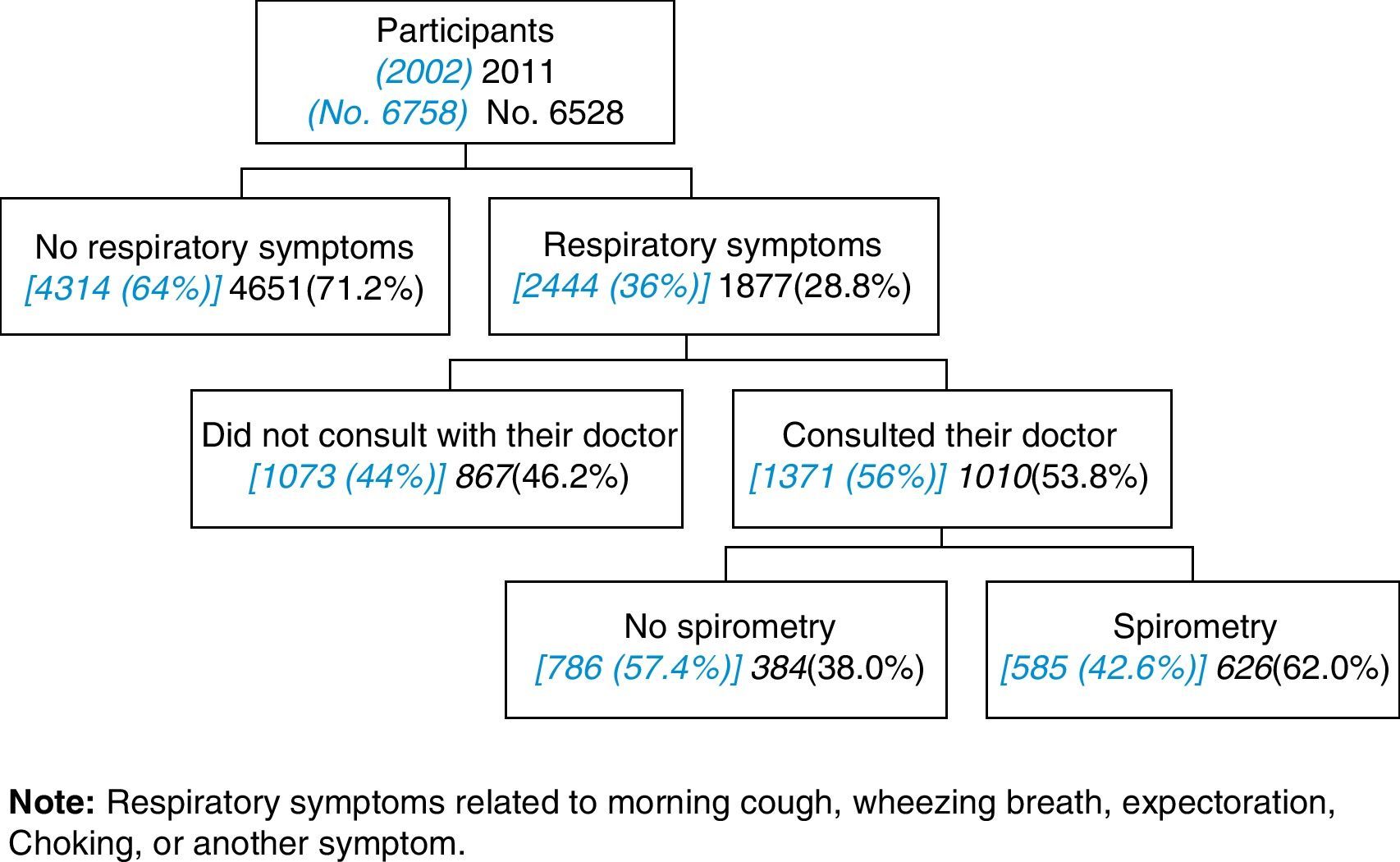
ResultsA total of 6528 responses were obtained (response rate of 13.1%), 53% of respondents were females with a mean age of 59.8years. Regarding tobacco use, 19.4% were current smokers while 27.9% reported being former smokers. Only 17.0% spontaneously recognized the term “COPD”. Valencia was the region with the highest degree of ignorance regarding COPD (91%), while Aragon had the lowest (73.7%). Nevertheless, COPD is considered a severe disease, following angina pectoris in severity. Upon comparing these results with the previous survey from 2002, we observed significant improvements in the knowledge and understanding of COPD (8.6% vs 17.0%), with a marked variability between the regions (P<.05). Currently, only 4.7% of the Spanish population knows that there is a National Strategy for COPD, although 86.0% have a favorable or very favorable opinion about the new Anti-tobacco Law.
ConclusionThe lack of knowledge about COPD and its determinants in the general population remains high compared to 2002; thus, more and better educational and awareness programs are necessary.
El objetivo de este estudio fue determinar el nivel de conocimiento actual sobre la enfermedad pulmonar obstructiva crónica (EPOC) y sus determinantes en la población general de España, y compararlo con una encuesta similar realizada en 2002.
MétodosEn septiembre de 2011 se realizó un estudio epidemiológico observacional transversal, mediante entrevista telefónica, con una muestra representativa de entre 40 y 80 años de dad en las 17 comunidades autónomas.
ResultadosSe obtuvo un total de 6.528 respuestas (porcentaje de respuesta del 13,1%), con el 53% de mujeres y una edad media de 59,8 años. Respecto al tabaco, el 19,4% eran fumadores actuales, mientras que el 27,9% referían ser ex fumadores. Solo el 17,0% refería espontáneamente que conocía el término EPOC. La Comunidad Valenciana era la que tenía un mayor grado de desconocimiento de la EPOC (91%), mientras que Aragón era la que lo tenía menor (73,7%). Pese a todo, la EPOC está considerada una enfermedad grave, solo por debajo de la angina de pecho. Comparando estos resultados con la encuesta anterior de 2002, se aprecian mejoras significativas respecto al conocimiento de la EPOC (8,6 vs. 17,0%), con una marcada variabilidad según la comunidad autónoma (p<0,05). Actualmente tan solo el 4,7% de la población española conoce que existe la Estrategia Nacional de EPOC, aunque el 86,0% tiene una opinión favorable/muy favorable sobre la nueva Ley antitabaco.
ConclusiónEl desconocimiento sobre la EPOC y sus determinantes en la población general se mantiene elevado respecto a 2002, por lo que son necesarias más y mejores intervenciones divulgativas y de concienciación.
COPD is a health-care problem, both at the individual as well as the population level.1 There are currently estimated to be 210 million people with COPD world-wide.2 The limited use of spirometry as a populational screening tool is partially responsible for the surprisingly high and homogenous underdiagnosis of COPD, which is from 80% to 90% in several regions of the world and in various scenarios. Therefore, estimating the number of people with COPD is useful, but these data must be used with caution.3 In general, the prevalence of COPD in the general population is estimated to be from 8% to 10% or more among those over the age of 40.
The EPI-SCAN study has estimated that the current prevalence of COPD in Spain in the population aged 40–80 was 10.2% (15.1% in males and 5.7% in women),4 meaning that there are currently 2185764 people with COPD in Spain, representing some 1.57 million men and more than 600000 women. Compared with the previous IBERPOC study,5 the underdiagnosis of COPD in Spain went down slightly, from 78% to 73%, although a great reduction in undertreatment was observed in this 10-year period, from 81% to 54% (P<.05).6 As for its main cause, smoking is estimated to cause 60000 deaths annually in Spain, and it is considered the most important cause of COPD and lung cancer.7
The underdiagnosis of COPD may be related with the lack of understanding of the disease and its determinants in the general population, as demonstrated in a study done in Spain in 2002.8 The study concluded that, in Spain, many people with respiratory symptoms did not request medical care and did not try to quit smoking, and also that there was a general lack of knowledge about COPD, and recommended that doctors more actively inform their patients about COPD and increase the use of spirometry.
The COPD Strategy of the National Healthcare System (NHS), approved June 3, 2009 by the Interregional NHS Council,9 sets as one of its priorities the development of strategies, objectives and recommendations in COPD for its application in the provinces. Likewise, the new Spanish COPD guidelines (GesEPOC) emphasize the role that the Strategy may play in the diffusion of information about this disease amongst the general population.10
The main objective of this CONOCEPOC study is to determine the current level of knowledge and understanding about COPD as well as its determinants in the general Spanish population. The secondary objectives were to analyze the changes observed almost ten years later, and at the same time to increase awareness about the importance of COPD. As a whole, the CONOCEPOC initiative intends to promote correct, early diagnoses of COPD in Spain.
MethodsCONOCEPOC is an observational, cross-sectional epidemiologic study done in September 2011 following an identical design to the study done in 2002.8 The inclusion criteria for participating in CONOCEPOC were men and women aged 40 and older who agreed to answer a telephone survey. In short, the survey was done in the 17 Autonomous Communities (provinces) in Spain. Participation was voluntary, confidential and anonymous, using randomized dialing of home phone numbers.11 In Spain, 80.6% of residences have a home phone.12 The sample was done with the following stratification criteria: sex, age according to decade (40–50, 51–60, 61–70 and >70); place of residence in a rural (<10000 inhabitants) or urban (≥10000 inhabitants) area. We obtained quotas of equal age, sex and place of residence within each of the 17 Spanish Autonomous Communities, requiring a total of 384 responses in each. This sample size offers precision in the samples by Community in population estimates with an error of 5% and a power of 80% for prevalences of different variables higher than 5%; thus the overall sample obtained is representative of each of the autonomous communities and is stratified by age groups and setting (rural vs urban).
Field WorkThe telephone interview was done by capable, previously trained interviewers. The phoning schedule was from 2pm to 9:30pm on business days, with an approximate duration of 15min per interview. After dialing a random home phone number in the corresponding Autonomous Community, there were several possible outcomes. If the number did not belong to a residence, the number was randomly substituted; if no one answered the phone and if after a maximum of 4 tries there was still no answer, the number was considered not contacted; another possible outcome was the subject's refusal to be interviewed. Last of all, a person who would be eligible for the interview may have not been at home at the time of the call, and the number was therefore considered to be a “postponed call”, and the day and time for the second phone call were recorded. If at the home there were more than one person over the age of 40, the interviewer requested their age and sex and selected from a list of random numbers which would be interviewed. With all these possible situations, the field work continued until the established quotas had been met.
The questions of the survey that were related with respiratory symptoms and diagnosis were based on the European Coal and Steel Community (ECSC) questionnaire, which has been translated to Spanish and validated,13 with additional questions about the knowledge of COPD, spirometry use and the perception of the severity of other chronic diseases, which was identical to the survey used previously.8 Last of all, current questions were added with regard to the knowledge of the National COPD Strategy and the new Anti-Tobacco Law.14 The complete questionnaire is included in the Appendix. The participants were asked about their spontaneous knowledge of COPD and other respiratory diseases that are considered severe or frequent, with no guidance from the interviewer. Those that spontaneously knew about COPD were asked to enumerate the symptoms that are directly related with the disease. The “suggested” knowledge about COPD was researched in the interviewees who did not show spontaneous knowledge about COPD. As in the survey from 2002,8 a high risk for COPD was defined as participants over the age of 55 with an accumulated consumption of tobacco use of at least 20 pack-years, who referred respiratory symptoms (morning cough, wheezing, expectoration, breathlessness or another symptom).
Statistical AnalysisThis is a descriptive study, and initially an analysis was done of tabulations and intervals in order to control the data quality. Later, frequencies were obtained of the categorical variables, while in the continuous variables central tendency (mean and median) and dispersion (standard deviation and minimum-maximum) were evaluated. The Chi-squared test was used to analyze the relationship between categorical variables. For the continuous variables, ANOVA was used in comparisons of three or more groups and the Student's t test was used for bivariate comparisons. Last of all, logistic regression was generated in order to explain that the independent variable have an unfavorable/very unfavorable opinion about the Anti-Tobacco Law according to a series of explicative variables, with adjustment by the “Introducir” method. All the statistical comparisons with a probability for error of less than 5% were considered significant.
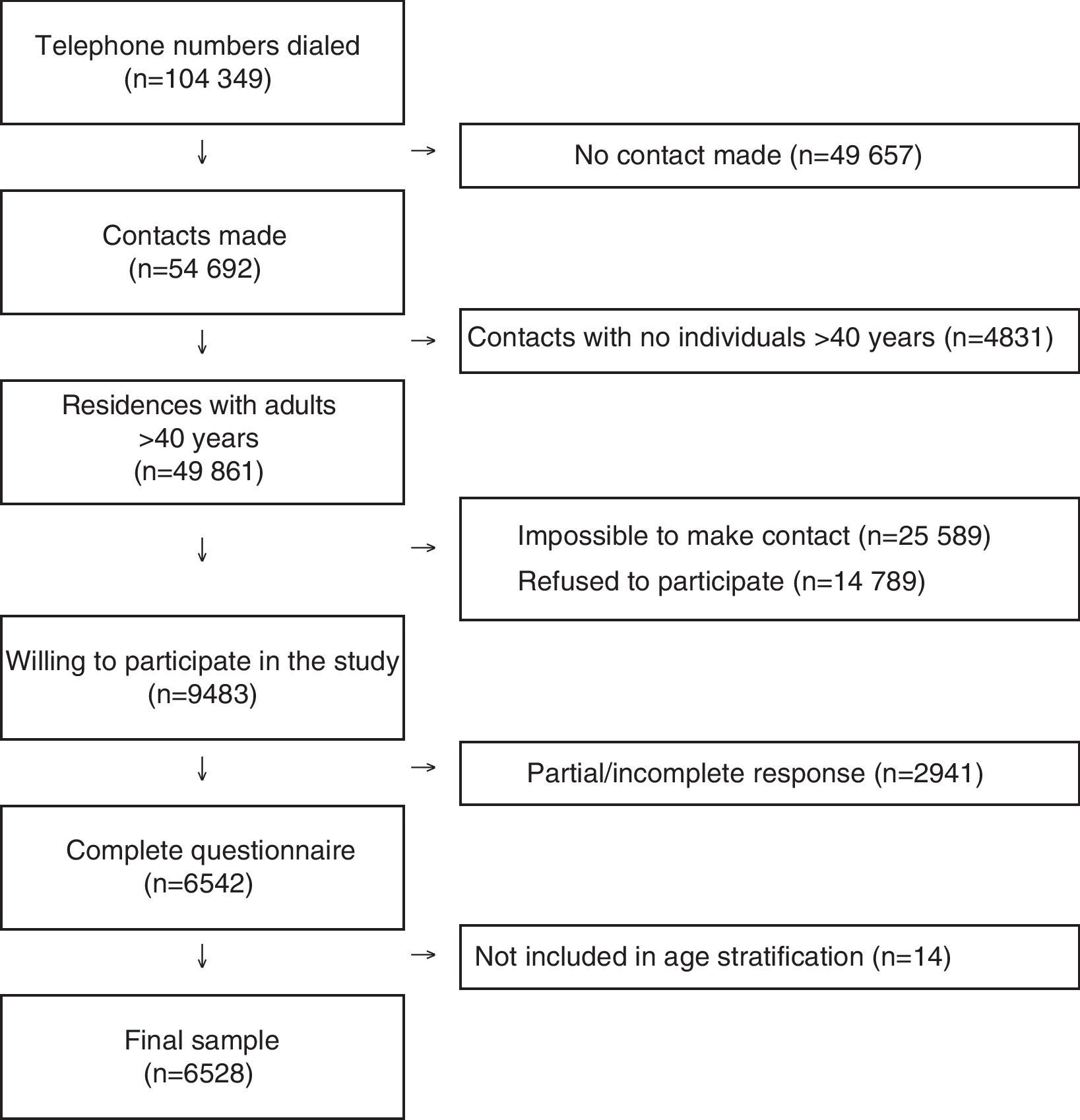
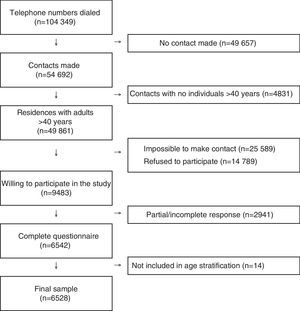
ResultsOut of a total of 104349 telephone contacts, a final sample was obtained of 6528 participants, with a response percentage of 13.1%, meaning 6528 final responses from 49861 residences identified with adults over the age of 40. The STROBE flow diagram of participants and non-participants are presented in Fig. 1.
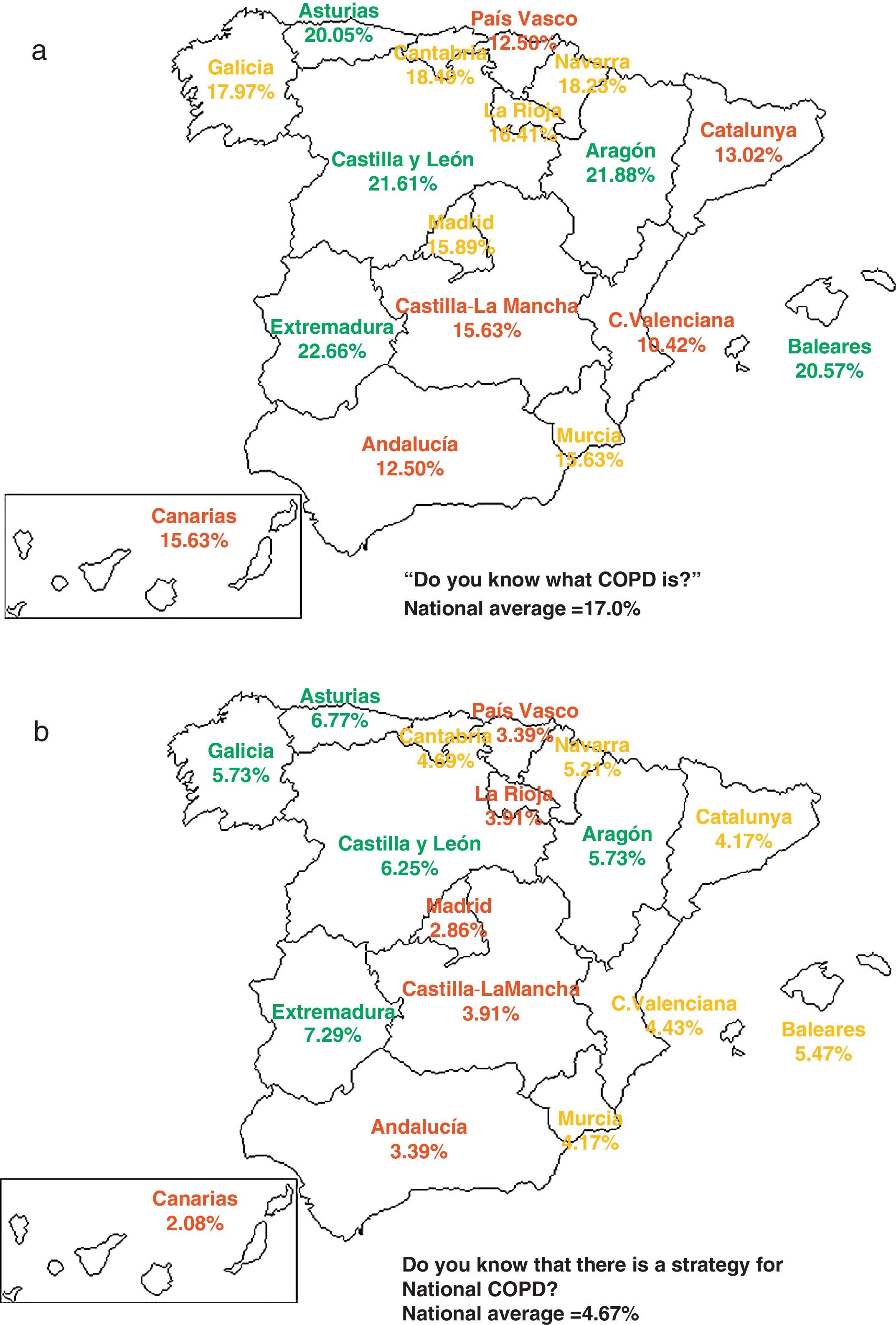
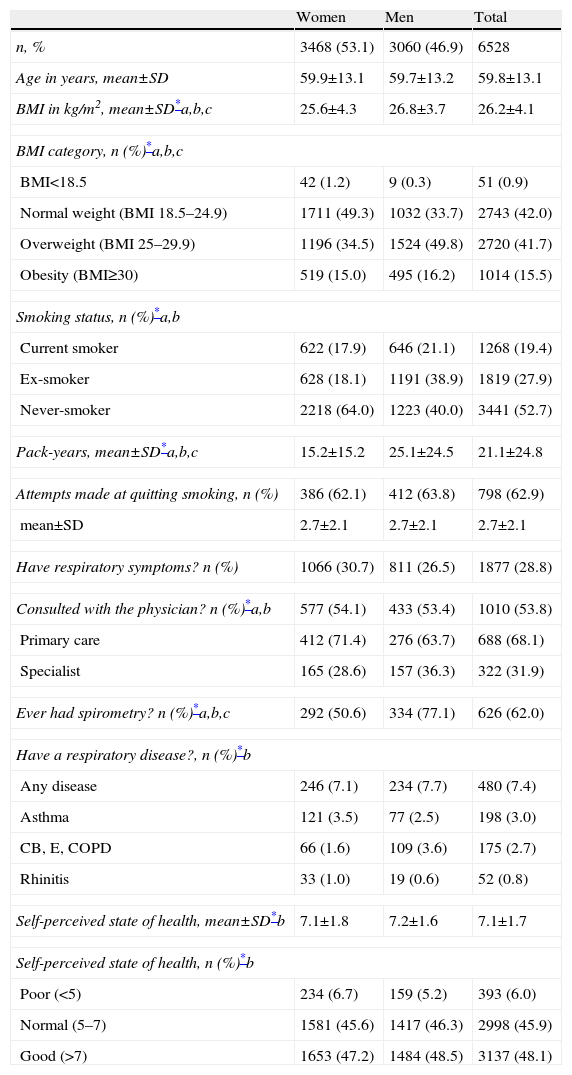
53.1% of participants were women, and the mean age of the population was 59.8. Table 1 presents the distribution of other sociodemographic, clinical and smoking variables according to sex. As for tobacco use, 19.4% were current smokers (17.9% in women and 21.1% in men) while 27.9% reported being ex-smokers (18.1% in women and 38.9% in men) (P<.05). Tobacco exposure measured in pack-years was greater in men (25.1±24.5) than in women (15.2±15.2) (P<.05). In smokers, 62.9% had tried to kick the habit, with a mean±SD number of attempts of 2.7±2.1, which was the same for both sexes. Only 9.6% of participants reported having had a spirometry at some time, including 8.4% of women and 10.9% of men (P<.05), distributed into three strata: 7.3% in those without respiratory symptoms or diagnoses; 68.2% in those with COPD diagnosis; and 47.2% in those with high risk for COPD (see Methods). From among the participants who reported respiratory symptoms, 53.8% had consulted a doctor, more often in Primary (68.1%) than in Specialized Care (31.9%). And among those who reported respiratory symptoms and had consulted a doctor, 62% had done a spirometry. There were no differences in the self-declared respiratory diseases or in the state of health for either sex or region, but there were differences depending on age groups (Table 1).
Sociodemographic Characteristics of the Participants.
| Women | Men | Total | |
| n, % | 3468 (53.1) | 3060 (46.9) | 6528 |
| Age in years, mean±SD | 59.9±13.1 | 59.7±13.2 | 59.8±13.1 |
| BMI in kg/m2, mean±SD*a,b,c | 25.6±4.3 | 26.8±3.7 | 26.2±4.1 |
| BMI category, n (%)*a,b,c | |||
| BMI<18.5 | 42 (1.2) | 9 (0.3) | 51 (0.9) |
| Normal weight (BMI 18.5–24.9) | 1711 (49.3) | 1032 (33.7) | 2743 (42.0) |
| Overweight (BMI 25–29.9) | 1196 (34.5) | 1524 (49.8) | 2720 (41.7) |
| Obesity (BMI≥30) | 519 (15.0) | 495 (16.2) | 1014 (15.5) |
| Smoking status, n (%)*a,b | |||
| Current smoker | 622 (17.9) | 646 (21.1) | 1268 (19.4) |
| Ex-smoker | 628 (18.1) | 1191 (38.9) | 1819 (27.9) |
| Never-smoker | 2218 (64.0) | 1223 (40.0) | 3441 (52.7) |
| Pack-years, mean±SD*a,b,c | 15.2±15.2 | 25.1±24.5 | 21.1±24.8 |
| Attempts made at quitting smoking, n (%) | 386 (62.1) | 412 (63.8) | 798 (62.9) |
| mean±SD | 2.7±2.1 | 2.7±2.1 | 2.7±2.1 |
| Have respiratory symptoms? n (%) | 1066 (30.7) | 811 (26.5) | 1877 (28.8) |
| Consulted with the physician? n (%)*a,b | 577 (54.1) | 433 (53.4) | 1010 (53.8) |
| Primary care | 412 (71.4) | 276 (63.7) | 688 (68.1) |
| Specialist | 165 (28.6) | 157 (36.3) | 322 (31.9) |
| Ever had spirometry? n (%)*a,b,c | 292 (50.6) | 334 (77.1) | 626 (62.0) |
| Have a respiratory disease?, n (%)*b | |||
| Any disease | 246 (7.1) | 234 (7.7) | 480 (7.4) |
| Asthma | 121 (3.5) | 77 (2.5) | 198 (3.0) |
| CB, E, COPD | 66 (1.6) | 109 (3.6) | 175 (2.7) |
| Rhinitis | 33 (1.0) | 19 (0.6) | 52 (0.8) |
| Self-perceived state of health, mean±SD*b | 7.1±1.8 | 7.2±1.6 | 7.1±1.7 |
| Self-perceived state of health, n (%)*b | |||
| Poor (<5) | 234 (6.7) | 159 (5.2) | 393 (6.0) |
| Normal (5–7) | 1581 (45.6) | 1417 (46.3) | 2998 (45.9) |
| Good (>7) | 1653 (47.2) | 1484 (48.5) | 3137 (48.1) |
Indicates statistically significant differences (P<.05) in the comparison (a) by sex, (b) by age, and (c) by Autonomous Communities. The variables for pack-years and attempts at quitting smoking are calculated only in the subgroup of smokers and ex-smokers. Also, with those who reported respiratory symptoms, it is shown whether a doctor was consulted (either Primary or Specialized Care) and if a spirometry had been done. CB: chronic bronchitis; E: emphysema.
It is interesting to observe that the diagnostic flow of the participants with respiratory symptoms who consulted with their physicians remains nearly the same compared to the previous survey (56% in 2002, and currently 53.8%), but there is an observed substantial increase in the use of spirometry in the subjects who consulted with their doctors due to respiratory symptoms (42.6% in 2002 and 62.0% at present) (P<.05) (Fig. 2).
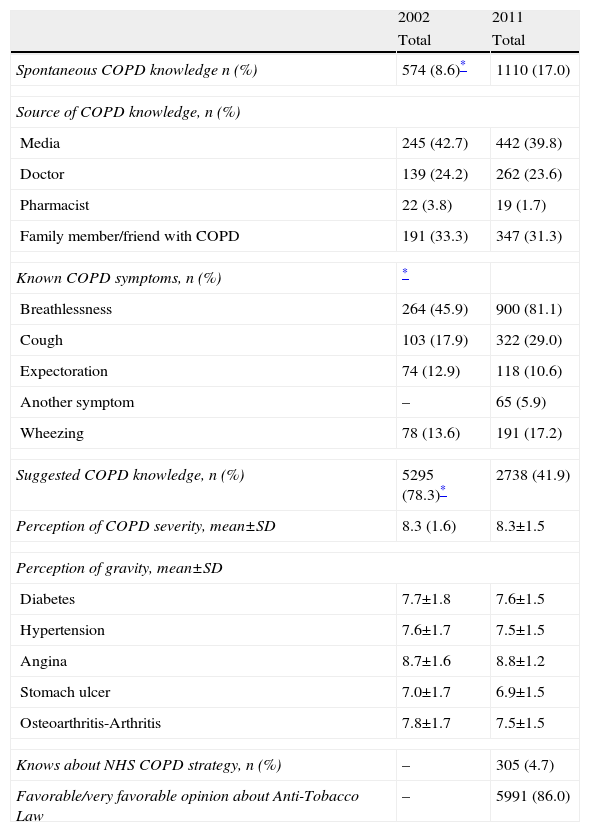
As for spontaneous knowledge about COPD, it was higher in women (18.1%) than in men (15.7%) (P<.05) (Table 2), and showed a decreasing tendency with age: 19.9% between 40 and 50, 23.6% between 51 and 60, 16.4% between 61 and 70 and only 8.8% in those over 70 (Chi2 tendency P<.05). Of these, 39.8% knew of COPD through the media. Knowledge of COPD showed great geographical variability (Fig. 3): residents in the province of Valencia knew the least about COPD (10.4%), while Aragón was the province to have the highest percentage of residents who knew about COPD (21.9%) (P<.05). From among those who declared knowing about COPD, their knowledge of the symptoms may be considered acceptable, as they were able to identify breathlessness (81.1%), cough (29.0%) and expectoration (10.6%) as the main symptoms of COPD, results that show improvement over those obtained in 2002 (P<.05). In fact, the perception of severity of COPD was very high 8.3±1.5, and only surpassed by angina, while in both sexes the perception of diabetes severity remained above the perception of severity of diabetes, hypertension, stomach ulcer and osteoarthritis/arthritis (Table 2).
Knowledge About COPD and Smoking in 2011, and Changes Versus 2002.
| 2002 | 2011 | |
| Total | Total | |
| Spontaneous COPD knowledge n (%) | 574 (8.6)* | 1110 (17.0) |
| Source of COPD knowledge, n (%) | ||
| Media | 245 (42.7) | 442 (39.8) |
| Doctor | 139 (24.2) | 262 (23.6) |
| Pharmacist | 22 (3.8) | 19 (1.7) |
| Family member/friend with COPD | 191 (33.3) | 347 (31.3) |
| Known COPD symptoms, n (%) | * | |
| Breathlessness | 264 (45.9) | 900 (81.1) |
| Cough | 103 (17.9) | 322 (29.0) |
| Expectoration | 74 (12.9) | 118 (10.6) |
| Another symptom | – | 65 (5.9) |
| Wheezing | 78 (13.6) | 191 (17.2) |
| Suggested COPD knowledge, n (%) | 5295 (78.3)* | 2738 (41.9) |
| Perception of COPD severity, mean±SD | 8.3 (1.6) | 8.3±1.5 |
| Perception of gravity, mean±SD | ||
| Diabetes | 7.7±1.8 | 7.6±1.5 |
| Hypertension | 7.6±1.7 | 7.5±1.5 |
| Angina | 8.7±1.6 | 8.8±1.2 |
| Stomach ulcer | 7.0±1.7 | 6.9±1.5 |
| Osteoarthritis-Arthritis | 7.8±1.7 | 7.5±1.5 |
| Knows about NHS COPD strategy, n (%) | – | 305 (4.7) |
| Favorable/very favorable opinion about Anti-Tobacco Law | – | 5991 (86.0) |
Only 4.7% of the population knows that there is a National COPD Strategy, and once again there was great geographical variability (Fig. 3). The Community of Madrid had the lowest degree of knowledge (2.9%), while Extremadura had the highest (7.3%) (P<.05).
Compared with the survey done in 2002, there are some significant changes seen in the current survey. The spontaneous knowledge about COPD doubled, going from 8.6% in 2002 to 17.0% in 2011 (P<.05) (Table 2). The knowledge about COPD symptoms also improved. In contrast, there were no significant differences in the source of knowledge of COPD or of the perception of its severity compared with other chronic diseases.
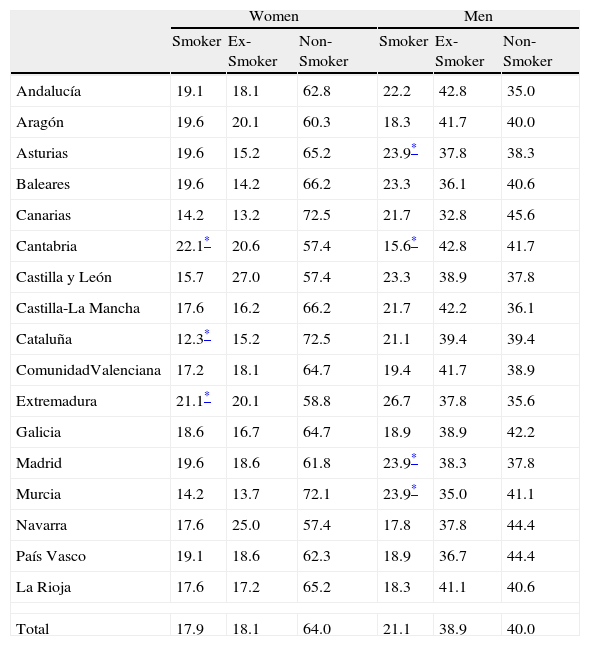
Due to the absence of current statistics, the prevalence of smoking has been described according to province (Table 3). In women, Cantabria and Extremadura presented the highest current prevalence of smoking (22.1% and 21.1%, respectively), while Catalonia was significantly lower at 12.3%. In men, the extremes were Asturias, Galicia and Madrid with 23.9% compared with the lowest in Cantabria at 15.6% (P<.05).
Prevalence of Smoking (%) by Sex According to Autonomous Community.
| Women | Men | |||||
| Smoker | Ex-Smoker | Non-Smoker | Smoker | Ex-Smoker | Non-Smoker | |
| Andalucía | 19.1 | 18.1 | 62.8 | 22.2 | 42.8 | 35.0 |
| Aragón | 19.6 | 20.1 | 60.3 | 18.3 | 41.7 | 40.0 |
| Asturias | 19.6 | 15.2 | 65.2 | 23.9* | 37.8 | 38.3 |
| Baleares | 19.6 | 14.2 | 66.2 | 23.3 | 36.1 | 40.6 |
| Canarias | 14.2 | 13.2 | 72.5 | 21.7 | 32.8 | 45.6 |
| Cantabria | 22.1* | 20.6 | 57.4 | 15.6* | 42.8 | 41.7 |
| Castilla y León | 15.7 | 27.0 | 57.4 | 23.3 | 38.9 | 37.8 |
| Castilla-La Mancha | 17.6 | 16.2 | 66.2 | 21.7 | 42.2 | 36.1 |
| Cataluña | 12.3* | 15.2 | 72.5 | 21.1 | 39.4 | 39.4 |
| ComunidadValenciana | 17.2 | 18.1 | 64.7 | 19.4 | 41.7 | 38.9 |
| Extremadura | 21.1* | 20.1 | 58.8 | 26.7 | 37.8 | 35.6 |
| Galicia | 18.6 | 16.7 | 64.7 | 18.9 | 38.9 | 42.2 |
| Madrid | 19.6 | 18.6 | 61.8 | 23.9* | 38.3 | 37.8 |
| Murcia | 14.2 | 13.7 | 72.1 | 23.9* | 35.0 | 41.1 |
| Navarra | 17.6 | 25.0 | 57.4 | 17.8 | 37.8 | 44.4 |
| País Vasco | 19.1 | 18.6 | 62.3 | 18.9 | 36.7 | 44.4 |
| La Rioja | 17.6 | 17.2 | 65.2 | 18.3 | 41.1 | 40.6 |
| Total | 17.9 | 18.1 | 64.0 | 21.1 | 38.9 | 40.0 |
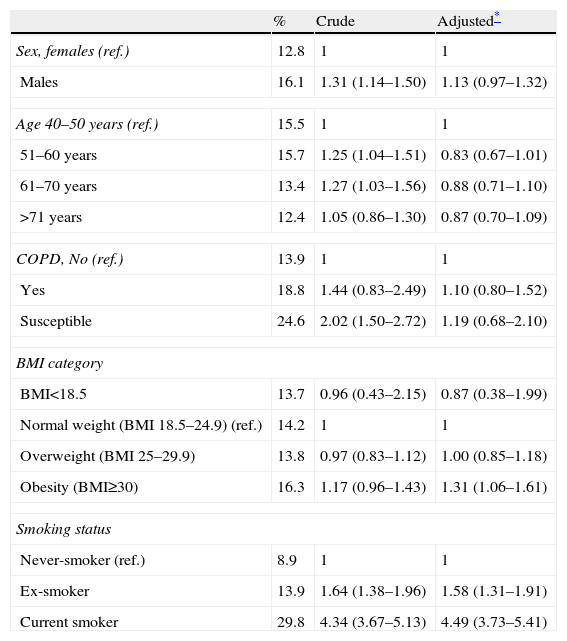
Finally, although the support received by the new Anti-Tobacco Law (Ley 42/2010, in place since January 2, 2011) was from 86% of the population, we explored the factors related with having an unfavorable/very unfavorable opinion in the remaining 14%. At the non-adjusted level, being male, young, with COPD or being susceptible to developing it, and being a current or ex-smoker was associated with this attitude. Nevertheless, in a multivariate analysis, only obesity (BMI>30kg/m2) and being either a current or ex-smoker maintained the association with an unfavorable/very unfavorable opinion of the new Anti-Tobacco Law (Table 4). These values maintained their magnitude and direction when we also adjusted for Autonomous Community (data not shown).
Factors Associated With Unfavorable/Very Unfavorable Opinions About the Anti-Tobacco Law.
| % | Crude | Adjusted* | |
| Sex, females (ref.) | 12.8 | 1 | 1 |
| Males | 16.1 | 1.31 (1.14–1.50) | 1.13 (0.97–1.32) |
| Age 40–50years (ref.) | 15.5 | 1 | 1 |
| 51–60years | 15.7 | 1.25 (1.04–1.51) | 0.83 (0.67–1.01) |
| 61–70years | 13.4 | 1.27 (1.03–1.56) | 0.88 (0.71–1.10) |
| >71years | 12.4 | 1.05 (0.86–1.30) | 0.87 (0.70–1.09) |
| COPD, No (ref.) | 13.9 | 1 | 1 |
| Yes | 18.8 | 1.44 (0.83–2.49) | 1.10 (0.80–1.52) |
| Susceptible | 24.6 | 2.02 (1.50–2.72) | 1.19 (0.68–2.10) |
| BMI category | |||
| BMI<18.5 | 13.7 | 0.96 (0.43–2.15) | 0.87 (0.38–1.99) |
| Normal weight (BMI 18.5–24.9) (ref.) | 14.2 | 1 | 1 |
| Overweight (BMI 25–29.9) | 13.8 | 0.97 (0.83–1.12) | 1.00 (0.85–1.18) |
| Obesity (BMI≥30) | 16.3 | 1.17 (0.96–1.43) | 1.31 (1.06–1.61) |
| Smoking status | |||
| Never-smoker (ref.) | 8.9 | 1 | 1 |
| Ex-smoker | 13.9 | 1.64 (1.38–1.96) | 1.58 (1.31–1.91) |
| Current smoker | 29.8 | 4.34 (3.67–5.13) | 4.49 (3.73–5.41) |
The main results of this survey are: only 17% of the Spanish population spontaneously knows anything about COPD, and the rates are higher among women and young adults than in older individuals. This represents a relative increase over the 8.6% observed in 2002,8 but it should still be considered a low percentage. The perception of severity of COPD is comparable to other frequent and severe diseases, such as angina. However, only half of people with symptoms who are compatible with COPD consult with their doctors, and only 62% of them had done spirometry. There is a notable variability by Autonomous Community about what COPD is and about the National COPD Strategy, although 86.0% of the population have a favorable/very favorable opinion about the new Anti-Tobacco Law. Last of all, the only individual factors that are independently associated with having an unfavorable/very unfavorable opinion about the new Anti-Tobacco Law were obesity and being either a current or ex-smoker.
Knowledge About Chronic Obstructive Pulmonary DiseaseCOPD continues to be unjustly considered a disease that is irreversible and of little therapeutic interest, whose treatment is mostly symptomatic and, aside from chronic oxygen therapy in patients with respiratory insufficiency and smoking cessation,15 many people continue to consider that there are no interventions that are able to modify the natural history of the disease. This vision is nihilist, and it is estimated that each year more than 18000 people each year die in Spain due to COPD. COPD is the fifth cause of death among males, with an annual rate of 60 deaths per 100000 inhabitants, and it is the seventh cause of death in women, with an annual rate of 17 deaths per 100000 inhabitants. According to the latest data from the National Institute of Statistics (NIS), the 382047 deaths in Spain in 2010 were 1.1% lower than in 2009, with 2886 fewer. Nonetheless, respiratory diseases were responsible for 10.5% of the deaths, becoming the third cause of death and provisionally 15662 deaths are attributed to COPD in 2010.16
Compared with other diseases like cancer or cardiovascular diseases, the secular absence of knowledge in the population about chest diseases in general, and of COPD in particular, mostly explain the historical disproportion between the magnitude of the problem and its low impact on public opinion, the reduced perception of a need for urgency in palliating the problem and the limited resources assigned for care and funding for research. Until 2006, respiratory diseases were not considered priority diseases in the Framework Programmes of the European Union, and only since February 2007 has the 7th Framework Programme incorporated respiratory diseases as a priority in European biomedical research for the first time.17 Another survey from 2000 in Spain and in seven other countries already highlighted the high load of COPD-related disease, even in adults younger than 65, which is still a potentially productive, working population.18 In particular, the results in Spain stood out due to the high cost associated with hospitalizations, which represented 84% of the direct costs of the disease. The study concluded that the implementation of measures for reducing the progression of the disease would also entail a reduction in its population load.19 Unlike the previous survey,8 there are no comparative series in Spain about the knowledge of COPD in the population, although another telephone survey done in March of 1999 coincided in showing that the term COPD was only recognized by 23% of the population.20 However, 94.3% recognized the term chronic bronchitis and 55.5% knew of pulmonary emphysema.
Bibliographic Review of Chronic Obstructive Pulmonary Disease and TobaccoAs for the trend in smoking in Spain, successive National Health Surveys from 1994, 1999 and 2007 in Spain showed evidence of a gradual reduction in the prevalence of smoking in men (42.1%, 39.1% and 32.2%, respectively) while there was an observed stagnation in women (24.7%, 24.6% and 22.1%, respectively).21 The latest official data are from 2009 by the European Health Survey,22 which concluded that in Spain 31.5% of the population aged 16 and older had smoked daily or occasionally in the last year. 27.3% smoked daily, 4.2% were occasional smokers, 20.2% were ex-smokers and 48.4% had never smoked. By sex, the percentage of smokers was 32.5% in men and 22.2% in women. Certainly, the results obtained in our survey are much lower (Table 3) than the abovementioned official results, and the method for obtaining them and their temporality merit caution in any comparison. However, our data, obtained nine months after the new law came into effect, show that 19.4% were current smokers (17.9% in women and 21.1% in men) while 27.9% reported being ex-smokers (18.1% in women and 38.9% in men) and they indicate a down-turning tendency that should be monitored.
Advantages and LimitationsOur study is populational and representative of the Spanish population, with more than 6000 responses from 384 participants in each of the 17 Autonomous Communities (provinces) in Spain. The study shows consistency in its results both internally and compared with the results from the 2002 survey. The sampling method of randomly dialing phone numbers is already considered the gold-standard technique and better than mailed surveys, while in our case it is probably also better than Internet surveys. However, some limitations should be considered regarding the successively small samples for age and sex because some estimators approach an estimated prevalence of less than 5%. Comparisons with the prevalence of smoking published in other media should be made with caution, as these are self-reported responses and have not been validated. In contrast, the latest official statistics date from 2009. As previously shown, the response percentage was 13.1%, which is sensitively lower than the previous survey from 2002, which was 38%.8 Nevertheless, this is considered acceptable for a randomly dialed telephone survey.11
ImplicationsThese results suggest an improvement, but much work is still necessary to raise public awareness about the relevance of respiratory diseases in general, and of COPD in particular. More emphasis should be placed on educating both men and seniors, where the spontaneous knowledge about COPD was significantly lower. This may also be said for the obese population and smokers or ex-smokers, who in addition had an unfavorable opinion about the new Anti-Tobacco Law. Proper implementation of recent legislation from January 2, 2011, which restricts smoking in public places as well as its publicity, should result in the future reduction of smoking in the Spanish population (as has been observed in Ireland, Italy or California) and consequently a reduction of the incidence of COPD. Moreover, the Spanish population is predicted to reach its maximum growth in 2050, with 53 million inhabitants, with a maximum aging around 2060.23 This will entail an increase in the population at risk for developing COPD, and thus the population load and resources necessary to manage these patients will either continue to remain at present rates or increase in future decades. Quality spirometry is a fundamental tool in primary and hospital care for detecting and confirming the limited airflow reversibility in individuals with respiratory symptoms and should be the beginning of the diagnostic and staging process in COPD.3,9
ConclusionThe lack of knowledge about COPD and its determinants in the general Spanish population is still high (at least since 2002), and therefore more and better interventions are necessary in order to raise public awareness.
FundingAlmirall S.A. has supported the CONOCEPOC study, while in 2002 it was Boehringer-Ingelheim and Pfizer who supported the study. The telephone surveys were done by Saatchi&Saatchi Health.
Conflict of InterestThe authors have no conflict of interest to declare.
We would like to thank the external reviewers of Archivos de Bronconeumología for their many constructive suggestions for modifications, which substantially improved the original manuscript.
Please cite this article as: Soriano JB, et al. Conocimientos de la población general sobre la enfermedad pulmonar obstructiva crónica y sus determinantes: situación actual y cambios recientes. Arch Bronconeumol. 2012;48:308-15.

![Diagnostic flow of participants with respiratory symptoms [in 2002] and in 2011. Diagnostic flow of participants with respiratory symptoms [in 2002] and in 2011.](https://static.elsevier.es/multimedia/15792129/0000004800000009/v1_201305150602/S1579212912001243/v1_201305150602/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w98FxLWLw1xoW2PaQDYY7RZU=)








