Tuberculosis (TB) continues to be a worldwide health problem and is the greatest infectious cause of death among young people and adults.1
Although TB treatment is free, patients will often stop treatment due to the inability of the patient and his/her relatives to provide the resources necessary to survive.2 Studies have shown that poverty and TB are closely linked, since the conditions under which poor populations live make them prone to the onset of the disease.1,3 The economic impact of TB arises from the fact that the majority of those affected are part of the labour force.1 Therefore, incentives have been employed by national TB control programs as a means of encouraging patients to adhere to treatment, helping to minimize the costs associated with the disease, as well as providing support to their families during the course of treatment.4
The consequences of the armed conflict that has occurred in Angola for about three decades has affected mainly the migration of the rural population to other regions, and the destruction of social infrastructures and traditional systems of economic activity.5In addition, the destruction of roads has led to the shortage of basic and other essential goods, giving rise to dramatic humanitarian situations.6 In this sense, the government has focused its attention on the affected populations, with the support of international institutions, mainly the United Nations Organizations (UN), through the World Food Program (WFP).6 Throughout the 1990s, WFP provided Angola with logistical support for intervention among populations in critical areas.
Since 2002, after the signing of the peace agreement in Angola,7 WFP has developed a humanitarian aid plan for TB patients hospitalized at the Huambo Sanatorium hospital and those who were being treated at the Anti-Tuberculosis Dispensary (ATD) outpatient clinic. This aid lasted 6 years and consisted in the distribution of a basic food basket that patients took home once a month during the outpatient treatment period. Inpatients received the prepared food at the hospital.
The program's implementation had as its purpose increasing the adherence of TB patients to the Directly Observed Treatment (DOT) and improving the success rates of anti-tuberculosis treatment.8
Due to lack of funding, WFP was forced to end humanitarian aid in Angola by the end of 2006, ahead of schedule. The government then assumed responsibility for providing the basic food basket to patients through the Ministry of Planning and the Ministry of Social Assistance and Reintegration (MINARS) until 2008.9 Since 2009 there has been no further incentive for TB patients.
The objective of this study was to evaluate the effect of incentives (basic food basket) on the treatment outcome of patients with TB in the ATD, Huambo.
A retrospective study is carried out. The study included 19739 cases of TB that were treated in the period between 2002 and 2014, in the ATD, Huambo. The study time was divided into two periods, the first one referring to the years 2002–2008, the period in which the basic baskets were distributed, and the second period referring to the years 2009–2014, during which there were no basic baskets. Data on the total TB cases and treatment outcomes were collected through the annual ATD reports, Huambo.
Treatment results were defined according to the WHO guidelines.10
The data available was analyzed through descriptive statistics. Mann–Whitney U test was used for group comparison.
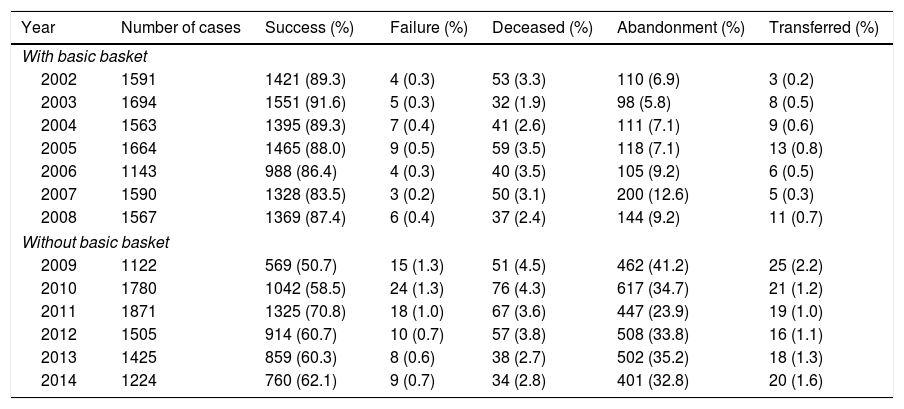
The results of the treatment of 19739 cases of TB were evaluated. In both periods, the median of therapeutic success (88% versus 60.5%, P=.001), the median of failure (0.3% versus 0.85%, P=.002) and the median of dropouts (7.1% versus 34.25%, P=.001) were significantly different. No difference was found in the deceased (3.1% versus 3.7%, P=.073). The results of the patients’ treatment are shown in Table 1.
Results of the Patients’ Treatment, Diagnosed With TB in the DAT, Huambo, During the Period From 2002 to 2014.
| Year | Number of cases | Success (%) | Failure (%) | Deceased (%) | Abandonment (%) | Transferred (%) |
|---|---|---|---|---|---|---|
| With basic basket | ||||||
| 2002 | 1591 | 1421 (89.3) | 4 (0.3) | 53 (3.3) | 110 (6.9) | 3 (0.2) |
| 2003 | 1694 | 1551 (91.6) | 5 (0.3) | 32 (1.9) | 98 (5.8) | 8 (0.5) |
| 2004 | 1563 | 1395 (89.3) | 7 (0.4) | 41 (2.6) | 111 (7.1) | 9 (0.6) |
| 2005 | 1664 | 1465 (88.0) | 9 (0.5) | 59 (3.5) | 118 (7.1) | 13 (0.8) |
| 2006 | 1143 | 988 (86.4) | 4 (0.3) | 40 (3.5) | 105 (9.2) | 6 (0.5) |
| 2007 | 1590 | 1328 (83.5) | 3 (0.2) | 50 (3.1) | 200 (12.6) | 5 (0.3) |
| 2008 | 1567 | 1369 (87.4) | 6 (0.4) | 37 (2.4) | 144 (9.2) | 11 (0.7) |
| Without basic basket | ||||||
| 2009 | 1122 | 569 (50.7) | 15 (1.3) | 51 (4.5) | 462 (41.2) | 25 (2.2) |
| 2010 | 1780 | 1042 (58.5) | 24 (1.3) | 76 (4.3) | 617 (34.7) | 21 (1.2) |
| 2011 | 1871 | 1325 (70.8) | 18 (1.0) | 67 (3.6) | 447 (23.9) | 19 (1.0) |
| 2012 | 1505 | 914 (60.7) | 10 (0.7) | 57 (3.8) | 508 (33.8) | 16 (1.1) |
| 2013 | 1425 | 859 (60.3) | 8 (0.6) | 38 (2.7) | 502 (35.2) | 18 (1.3) |
| 2014 | 1224 | 760 (62.1) | 9 (0.7) | 34 (2.8) | 401 (32.8) | 20 (1.6) |
Our study showed that between 2002 and 2008, when basic food baskets were distributed to TB patients, the success rate of treatment was higher than in the period from 2009 to 2014, when there were no food baskets. With the removal of such incentives to patients, there was a considerable increase in treatment withdrawal. Similar to our study, a study conducted in Afghanistan found that the treatment success increased from the moment that the WFP introduced food assistance to TB patients.4 In Brazil, the provision of basic food baskets significantly increased adherence to TB treatment.11 Other studies have also shown the positive impact of incentives on patients’ adherence to TB treatment,12,13 taking into account the socio-economic difficulties experienced by these vulnerable groups.3
We assume that the incentive impact assessment in the outcome of treatment in our study was limited to the analysis of grouped data and that the sociodemographic and socioeconomic data of each patient would need to be assessed for a more complete analysis. However, our analysis strongly suggests the importance of incentives in patients’ adherence to treatment, and therapeutic success against TB.